Information
Journal Policies
Comparison of the Hyperuricemic Effects of Erythropoietin and U-74389G
C. Tsompos1*, C. Panoulis2, K. Toutouzas3, A. Triantafyllou4, CG. Zografos5, K. Tsarea6, M. Karamperi6, A. Papalois6
2.Department of Obstetrics&Gynecology, Aretaieion Hospital, Athens University, Athens, Attiki, Hellas
3.Department of Surgery, Ippokrateion General Hospital, Athens University, Athens, Attiki, Hellas
4.Department of Biologic Chemistry, Athens University, Athens, Attiki, Hellas
5.Department of Surgery, Ippokrateion General Hospital, AthensUniversity, Athens, Attiki, Hellas
6.ExperimentalResearch Centre ELPEN Pharmaceuticals, S.A. Inc., Co., Pikermi, Attiki, Hellas
Copyright : © 2018 . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Aim: This study calculated the hyperuricemic capacities of 2 drugs: the erythropoietin (Epo) and the antioxidant lazaroid (L) drug U-74389G. The calculation was based on the results of 2 preliminary studies, each one of which estimated the hyperuricemic influence, after the respective drug usage in an induced ischemia reperfusion animal experiment.
Materials and Methods: The 2 main experimental endpoints at which the serum uric acid levels were evaluated was the 60th reperfusion min(for the groups A, C and E)and the 120th reperfusion min (for the groups B, D and F). Specially, the groups A and B were processed without drugs, groups C andD after Epo administration; whereas groups Eand F after the L administration.
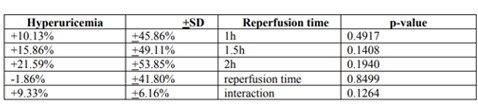
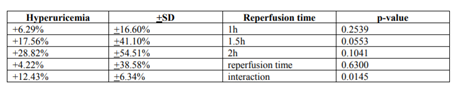
Results: The first preliminary study of Epo presented a non significant hyperuricemic effect by 9.33%+6.16% (p-value=0.1264). The second preliminary study of U-74389G presented a significant hyperuricemic effect by 12.43%+6.34% (p-value=0.0145). These 2 studies were co-evaluated since they came from the same experimental setting. The outcome of the co-evaluation was that U-74389G has 1.33234-fold more hyperuricemicpotency thanEpo (p-value=0.0000).
Conclusions: The anti-oxidant capacities of U-74389G enhance the acute hyperuricemic properties presenting 1.33234-fold more intentive hyperuricemia than Epo (p-value=0.0000).
ischemia; erythropoietin; U-74389G; serum uric acid levels; reperfusion,Nephrology
1. Introduction
The lazaroid U-74389G (L) is not famous for its hyperuricemic1 capacity (p-value=0.0145). U-74389G as a novel antioxidant factor, implicates exactly only 258 published studies. The ischemia reperfusion (IR) type of experiments was noted in18.60% of these studies. A tissue protective feature of U-74389G was obvious in these IR studies. The U-74389G chemically known as 21-[4-(2, 6-di-1-pyrrolidinyl-4-pyrimidinyl)-1-piperazinyl]-pregna-1, 4, 9(11)-triene-3, 20-dione maleate salt is an antioxidant complex, which prevents the lipid peroxidation either iron-dependent, or arachidonic acid-induced one. Animal kidney, liver, brain microvascular endothelial cells monolayers and heart models were protected by U-74389G afterIR injury. U-74389G also attenuates the leukocytes; down-regulates the proinflammatory gene; treats the endotoxin shock; produces cytokine; enhances the mononuclear immunity; protects the endothelium and presents anti shock property.
Erythropoietin (Epo) even if is not famous for itshypruricemicaction (p-value=0.1264), it can be used as a reference drug for comparison with U-74389G. Although Epo is met in over 30,327 published biomedical studies, only a 3.56% of them negotiate the known type of IR experiments. Nevertheless, Epo as a cytokine, it is worth of being studied about serum uric acid levels too.
This experimental work tried to compare the hyperuricemic effects of the above drugs on a rat induced IR protocol. They were tested by calculating the serum uric acid (SUA) levels increases.
2. Materials And Methods
The Vet licenses under 3693/12-11- 2010 & 14/10-1-2012 numbers, the granting company and the experiment location are mentioned in preliminary references[1,2]. The human animal care of Albino female Wistar rats, the 7 days pre-experimental ad libitum diet, the non-stop intra-experimental anesthesiologic techniques, the acidometry, the electrocardiogram, the oxygen supply and post-experimental euthanasia are also described in preliminary references. Rats were 16 – 18 weeks old. They were randomly assigned to six (6) groups consisted in N=10. The stage of 45 min hypoxia was common for all 6 groups. Afterwards, reperfusion of 60 min was followed in group A; reperfusion of 120 min in group B; immediate Epo intravenous (IV) administration and reperfusion of 60 min in group C; immediate EpoIV administration and reperfusion of 120 min in group D; immediate U-74389G IV administration and reperfusion of 60 min in group E; and immediate U-74389G IV administration and reperfusion of 120 min in group F. The dose height assessment for both drugs are described at preliminary studies as 10 mg/Kg body mass.
Ischemia was caused by laparotomic clamping the inferior aorta over renal arteries with forceps for 45 min. The clamp removal was restoring the inferior aorta patency and reperfusion. After exclusion of the blood flow, the protocol of IR was applied, as described above for each experimental group. The drugs were administered at the time of reperfusion; through inferior vena cava catheter. TheSUA levels (SUAl) were determined at 60th min of reperfusion (for A, C and E groups) and at 120th min of reperfusion (for B, D and F groups). However, the predicted SUAl values were not used since a weak relation was rised with animals’ mass (p-value=0.3436).
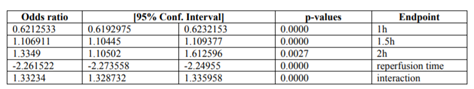
Table 1 presents the (%) hyperuricemic influence of Epo regarding reoxygenation time. Also, Table 2 presents the (%) hyperuricemic influence of U-74389G regarding reperfusion time. Chi-square tests were applied using the ratios which produced the (%) results per endpoint. The outcomes of chi-square tests are depicted at Table 3. The statistical analysis was performed by Stata 6.0 software [Stata 6.0, Stata Corp LP, Texas, USA].
3. Results
The successive application of chi-square tests revealed that U-74389G recessed the hyperuricemia by 0.6212533-fold [0.6192975 - 0.6232153] than Epo at 1h; however, it accentuated it by 1.106911-fold [1.10445 - 1.109377] at 1.5h, by 1.3349-fold [1.10502 - 1.612596], by 2.261522-fold [2.24955 - 2.273558] without drugs and by 1.33234-fold[1.328732 - 1.335958] whether all variables have been considered (p-value=0.0000).
4. Discussion
The unique available study investigating the hyperuricemic effect of U-74389G on SUAl was the preliminary one[1] . Although the most famous activities of neuroprotection and membranestabilization properties, it accumulates in the cell membrane, protecting vascular endothelium from peroxidative damage but hardly penetrates the blood-brain barrier. It elicits a beneficial effect in ototoxicity and Duchenne muscular dystrophy. It increases gamma-glutamyl transferase (γgt), superoxide dismutase (SOD) and glutathione (GSH) levels in oxygen-exposed cells. It treats septic states and acts as immunosuppressant in flap survival. It prevents the learning impairments, it delays the early synaptic transmission decay during hypoxia improving energetic state of neurons. It shows antiproliferative properties on brain cancer cells and is considered as a new promising anti inflammatory drug for the treatment of reperfusion syndrome in IR injuries.
The same authors confirmed[2] the short-term hyperuricemic effect of Epo preparations in non iron deficient individuals. Palmiere C et al proposed[3] several biochemical markers including serum uric acid as potentially useful markers to improve the diagnostic efficacy in hypothermia fatalities. Chen YR et al found[4] that multidisciplinary care (MDC) group had higher prescription rates of uric acid lower agents and erythropoietin-stimulating therapy in chronic kidney disease (CKD) patients. Lambers Heerspink HJ et al made drug targets specifically related with kidneys as the uric acid and erythropoietin, the subject of clinical trials in CKD patients. Sulikowska B et al found[6] subjects with both a fall in EPO and lower serum uric acid despite similar inflammation and fibrosis on biopsy than others in IgA nephropathy. Kmoch S et al described the autosomal dominant tubulointerstitial kidney disease, REN-related (ADTKD-REN) characterized[7] by: hypoproliferative anemia with low hemoglobin concentrations, found in most affected children by age one year; hyperuricemia (serum uric acid concentration >6 mg/dL) and gout, found in most (not all) affected individuals; and slowly progressive chronic tubulointerstitial kidney disease. Balaguer C et al found that treatment with simvastatin increased[8] the plasma levels of erythropoietin (Epo) by 61.90% p < 0.05 and reduced those of serum uric acid levels by 8.45% p < 0.01 in stable COPD patients. Fleming WE et al showed[9] that ROC curve analysis of EPO and uric acid as biomarkers, were superior than the Epworth Sleepiness Scale by at least 17.30% in screening for obstructive sleep apnea (OSA). Schaalan MF et al found the EPO levels decreased (77.8%) than control levels, whereas increased (1.9-fold) than pretreatment values and higher levels of uric acid (2.3-fold)[10] in septic acute kidney injury (AKI) patients. D'Arrigo G et al suggested[11] that vitamin Ecoated membranes significantly improved the erythropoietin resistance index but had no impact on other anemia parameters and serum uric acid levels.Georgatzakou HT et al assessed[12] that the antioxidant, antihemolytic and anti-apoptotic effects of high rhEPO doses blunted the more toxic uremic context and probably of serum uric acid levels in patients with end-stage renal disease (ESRD).Gounden V et al repeated the[13] vital role of kidneys in the excretion of waste products and toxins such as uric acid, as well as the production of hormones like erythropoietin. Fleming WE et al[14] utilized the concurrent elevations of HbA1c, CRP and EPO levels as an obstructive sleep apnea (OSA) screening tool superior than STOP-Bang questionnaires by 11.42%.
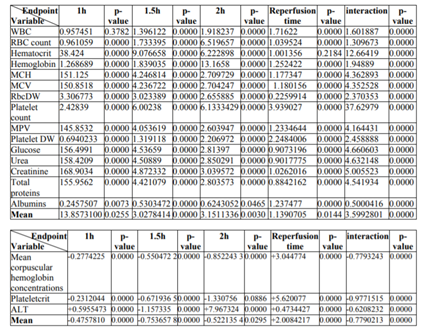
According to above, table 3 shows that U74389G accentuated by 1.33234-fold [1.328732 - 1.335958] the hyperuricemicpotency than Epo (p-value=0.0000); a trend accentuated along time, in Epo non-deficient rats. A meta-analysis of these ratios from the same experiment, for 15 other seric variables, provides comparable results (table 4)[15].
5. Conclusion
The anti-oxidant agent U-74389G not only was proved also more hyperuricemic by 4.660603-fold [4.655341-4.665871] than Epo (p-value =0.0000), but also this trend is accentuated along the short term time frame of the experiment in rats. A biochemical investigation remains about how U-74389G mediates in these actions.
References
- Τsompos C., Panoulis C., Τοutouzas K., Triantafyllou A., Ζografos G., Papalois A. The Effect of the Antioxidant Drug “U-74389G” on Uric acid Levels during Ischemia Reperfusion Injury in Rats.Ser J Exp Clin Res 2016; 17 (2): 1-1.
- C. Τsompos, C. Panoulis, K. Τοutouzas, G. Ζografos, A. Papalois. The effect of erythropoietin on serum uric acid levels during renal ischemia reperfusion injury in rats. Turkish Journal of Urology 2014; 40 (2): 110-114.
- Palmiere C, Mangin P. Postmortem biochemical investigations in hypothermia fatalities. Int J Legal Med. 2013 Mar; 127(2):267-76.
- Chen YR, Yang Y, Wang SC, Chiu PF, Chou WY, Lin CY, Chang JM, Chen TW, Ferng SH, Lin CL. Effectiveness of multidisciplinary care for chronic kidney disease in Taiwan: a 3-year prospective cohort study. Nephrol Dial Transplant. 2013 Mar; 28(3):671-82.
- Lambers Heerspink HJ, de Zeeuw D. Novel drugs and intervention strategies for the treatment of chronic kidney disease. BrJClin Pharmacol. 2013 Oct;76(4):536-50.
- SulikowskaB, JohnsonRJ, Wiechecka-KorenkiewiczJ, Korenkiewicz J, MarszalekA, Odrowaz-SypniewskaG, ManitiusJ. Dopamine-Induced Changes in Serum Erythropoietin and Creatinine Clearance Reflect Risk Factors for Progression of IgA Nephropathy. J Investig Med. 2015 Aug; 63(6):811-5.
- Kmoch S, Živná M, Bleyer AJ. Autosomal Dominant Tubulointerstitial Kidney Disease, REN-Related. Gene Reviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2018.
- Balaguer C, Peralta A, Ríos Á, Iglesias A, Valera JL, Noguera A, Soriano JB, Agustí À, Sala-Llinas E. Effects of simvastatin in chronic obstructive pulmonary disease: Results of a pilot, randomized, placebo-controlled clinical trial. ContempClin Trials Commun. 2016 Jan 14; 2:91-96.
- Fleming WE, Ferouz-Colborn A, Samoszuk MK, Azad A, Lu J, Riley JS, Cruz AB, Podolak S, Clark DJ, Bray KR, Southwick PC. Blood biomarkers of endocrine, immune, inflammatory, and metabolic systems in obstructive sleep apnea. ClinBiochem. 2016 Aug; 49(12):854-61.
- Schaalan MF, Mohamed WA. Determinants of hepcidin levels in sepsis-associated acute kidney injury: Impact on pAKT/PTEN pathways?J Immunotoxicol. 2016 Sep; 13(5): 751-7. 11. D'Arrigo G, Baggetta R, Tripepi G, Galli F, Bolignano D. Effects of Vitamin E-Coated versus Conventional Membranes in Chronic Hemodialysis Patients: A Systematic Review and Meta-Analysis. Blood Purif. 2017; 43(1-3):101-122.
- Georgatzakou HT, Tzounakas VL, Kriebardis AG, Velentzas AD, Papageorgiou EG, Voulgaridou AI, Kokkalis AC, Antonelou MH, Papassideri IS. Pathophysiological aspects of red blood cells in end-stage renal disease patients resistant to recombinant human erythropoietin therapy. Eur J Haematol. 2017 Jun; 98(6):590-600. [
- Gounden V, Jialal I. Renal Function Tests. Stat Pearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018-.2018 May 25.
- Fleming WE, Holty JC, Bogan RK, Hwang D, Ferouz-Colborn AS, Budhiraja R, Redline S, Mensah-Osman E, Osman NI, Li Q, Azad A, Podolak S, Samoszuk MK, Cruz AB, Bai Y, Lu J, Riley JS, Southwick PC. Use of blood biomarkers to screen for obstructive sleep apnea. Nat Sci Sleep. 2018 Jun 14; 10:159-167.
- Τsompos C, Panoulis C, Τοutouzas K, Triantafyllou A, Ζografos C, Tsarea K, Karamperi M, Papalois A. Comparison of the Acute Hypervolemic Capacities of Erythropoietin and U-74389G Concerning Mean Corpuscular Volume Levels. Innovations Tissue Eng Regen Med. 1(1). ITERM. 000503. 2018.
- Τsompos C, Panoulis C, Τοutouzas K, Triantafyllou A, Ζografos C, Tsarea K, Karamperi M, Papalois A. The Opposite Metabolic Effects of Erythropoietin and U74389Gon Serum Alanine Amino Transferase Levels. Journal of Genetics and Genetic Engineering Volume 2, Issue 2, 2018, PP 17-23.