Information
Journal Policies
Urinary NGAL and L-FABP as Valuable Biomarkers for Early Detection of Acute Kidney Injury in Intensive Care Unit Patients
Eman Rafaat Youness1*, Sahar Mohamed Ismail2, Abeer AbdElfatah Ali2, Aml Mokhtar Ahmed2, Samah Mohamed Oquab2
2.Department of Internal Medicine, Faculty of Medicine (for girls), AlAzhar University, Cairo, Egypt.
Copyright : © 2018 . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Background: Acute kidney injury (AKI) is one of the most frequent problems occurring in critical patients of the intensive care unit and strongly associated with increase morbidity and mortality in these patients. AKI is diagnosed by serum creatinine, however creatinine has limitation. Therefore, more sensitive and specific biomarkers are needed to detect acute kidney injury at an early stage.
Objective: To assess the role of urinary neutrophil gelatinase associated lipocalin and urinary liver fatty acid binding protein in early detection of AKI in ICU patients.
Methods: Eighty patients were recruited from inpatient of ICU of Alzahraa university hospital; these patients were recently admitted to ICU (within 6hours) with normal serum creatinine on admission. Then they were classified after 48 hours according to KIDGO Criteria into AKI group which included 38 patients (47.5%) and non AKI group which included 42(52.5%). According to this criteria AKI group was further subdivided into three stages (1, 2, 3) respectively.
Results: There was a highly significant increase in the mean of u-NGAL and u-L-FABP among AKI group when compared to non AKI group. Urinary NGAL and L-FABP were not only correlated with AKI, but also correlated with the degree of renal injury in conjunction with the KIDGO criteria.
Conclusion: AKI in ICU have been associated significantly with increase morbidity and mortality even in mildest degree of AKI so the need for early diagnosis is mandatory. Urinary NGAL and L-FABP can be used as early biomarker for diagnosis of AKI in ICU patients.
Acute kidney injury, Urinary neutrophil gelatinase (u-NGAL) associated lipocalins, urinary liver fatty acid binding protein ,Nephrology
1. Introduction
AKI is one of the most frequent problems occurring in the critical ill patients of the intensive care unit (ICU) and is strongly associated with increased morbidity and mortality in these patients.[1], AKI is characterized by an abrupt decline in renal function, resulting in an inability to secrete wastes and maintain electrolyte and water balance.[2] Acute kidney injury is aserious and common condition which affect 3-18% of all hospitalized patients[3] it affects around 34% of critical ill adult, and carries hospital mortality as high as 62%[4].
Identifying risk factor for developing AKI(like diabetes mellitus, hypertension, dehydration, advance age or pervious AKI) has become apriority so that preventative treatment can occur.[5]AKI occurs either due to prerenal injury ,intrinsic kidney or obstructive uropathies and the prognosis of AKI is highly dependent on the underlying cause of injury. Sepsis is the leading cause of AKI in ICU and 45-70% of all AKI cases are associated with sepsis which carries high mortality[2].
Although serum creatinine is a commonly used marker for renal function, it fails as a marker for renal injury due to the following reasons:-1-serum creatinine level increases after changes in glomerular filtration, and hence is thought to be a delayed marker for decreased renal function - 2- serum creatinine increase from 4 hours to elevated after 24 to72 hours if glomerular filtration rate decrease -3-serum creatinine is affected by non-renal factors such as age, sex, body weight, muscle mass, total body volume, and protein intake ,so it is not reliable marker for early detection of AKI[6] . Therefore, more sensitive and specific biomarkers are needed to detect AKI at an early stage.
Neutrophil gelatinase associated lipocalin (NGAL) is a small molecule of 178 amino acids that belongs to the super family of lipocalins, which are proteins specialized in binding and transporting small hydrophobic molecules. In healthy kidneys it is barely detectable in either plasma or urine. However in the setting of acute tubular injury, NGAL undergoes rapid and profound upregulation with large increases in both urine and plasma[7].
liver fatty acid binding protein (L-FABP) is a 15 KDa protein that belongs to the family of fatty acid binding proteins (FABA) this small protein is involved in cellular long chain fatty acid metabolism and is abundantly expressed in tissues with an active fatty acid metabolism like heart and liver, Following cell damage, FABA is rapidly released into the interstitium and plasma. Urinary L-FABP is undetectable in the urine of healthy subjects. Many studies have explored the potential utility of urinary L-FABP as a biomarker for early diagnosis of AKI[8].
Our aim was to assess the role of urinary neutrophil gelatinase associated lipocalin and urinary liver fatty acid binding protein in early detection of acute kidney injury in intensive care unit patients.
2. Patients And Methods
The comparative study don on eighty patients were recruited from inpatient of ICU of Alzahraa hospital during the period from September 2015 to September 2016, from those 80 patients 44(55%) were males and 36(45%) were females and their mean age was (47.36±10.50) years old. An informed consent was taken from each patient after explaining the purpose and implication of the study which was reviewed and approved by the ethical committee of the Faculty of Medicine for Girls, Al Azhar University.
These patients were recently admitted to ICU (within 6hours) with normal serum creatinine on admission. Then they were classified after 48 hours according to KIDGO Criteria (2012)9 KDIGO criteria, AKI is staged as follows: Stage 1- 1.5-1.9 times baseline OR ≥0.3 mg/dl (≥26.5 micromol/l) increase in the serum creatinine, OR urine output < 0.5 ml/kg per hour for 6 to 12 hours. Stage 2 -2.0-2.9 times baseline increase in the serum creatinine OR urine output < 0.5 ml/kg per hour for ≥12 hours. Stage 3 - 3.0 times baseline increase in the serum creatinine OR increase in serum creatinine to ≥4.0 mg/dl (≥353.6 micromol/l) OR urine output of < 0.3 ml/kg per hour for ≥24 hours, OR anuria for ≥12 hours OR the initiation of renal replacement therapy OR, in patients < 18 years, decrease in estimated GFR to < 35 ml/min.
AKI group which included 38 patients (47.5%) and non AKI group which included 42(52.5%). According to this criteria AKI group was further subdivided into three stages (1, 2, 3) respectively.
1. Stage (1): which include 13 patients (16.3%)
2. Stage (2): which include 8 patients (10%)
3. Stage (3): which include 17 patients (21.3%)
2.1.1. Exclusion Criteria
Readmitted patients who received renal replacement therapy (RRT) during pervious admission, end stage renal disease (ESRD) or patients on chronic dialysis. Post renal transplantation surgery or patients with past history of nephrectomy. Chronic kidney disease as known case of polycystic kidney, lupus nephritis, diabetic nephropathy, diabetic patients with albumin creatinine ratio more than 2.5mg/mmol for male or more than 3.5 mg/mmol for female, IGA nephropathy or any past history of renal disease also patient with severe urinary tract infection, kidney malignancy were excluded.
All patients included in this study were subjected to the following:
1. Full medical history and complete clinical examination including calculation of BMI and calculation of APACH II scores for grading of illness severity. The APACHE II scoring system consists of: Acute Physiology score (APS), Age points, and Chronic Health points. The total APACHE II score ranges between zero and 71 points. Points of 25 or less denote less than 50% mortality while points of 35 or more denote more than 80% mortality.
2. 24 hours measurement of urine output till discharge from ICU.
3. Routine laboratory investigations: serum creatinine (on admission then follow up daily during ICU stay and estimation of GFR by using MDRD formula), 1 cm of blood sample was collected into sterile test tube from each patients at time of admission and daily during ICU stay and allowed to be clot then centrifuged and serum was aliquoted then analyzed by colorimetric technique. Complete blood count (CBC), lipid profiles, fasting blood sugar, liver function tests, Erythrocyte sedimentation rate (ESR), Creactive protein (CRP), urine analysis, arterial blood gases.
4. U-NGAL and urinary L-FABP were measured on admission. Urine sample were collected by sterile methods in sterile urinary cup. Patients who were catheterized, the urinary catheter were separated at the connection between catheter and catheter tubing containers, the stored urine dripped then catheter were clamped by non-crushed artery clamp for minutes to allow urine to collected in the bladder then clamp was opened, urine sample were collected in sterile cups. u- NGAL and urinary L FABP were measured by enzyme linked immunosorbant assay (ELISA) technique using sandwich ELISA method.
5. Pelviabdominal U/S, ECG, ECHO cardiography was done.
6. Follow up to patients during ICU stay including urine output hourly, initiation of RRT, TCU stay, mortality and need for mechanical ventilation.
Data were analyzed using statistical program for social science (SPSS) version 23. Quantitative variables were expressed as mean± stander deviation (SD) for normally distributed data. Qualitative variables were expressed as frequency and percentage. A one way analysis of variance (ANOVA) was use when comparing between more than two means. Chi-square(X2) test was used in order to compare proportions between qualitative parameters, p value higher than 0.05 was considered insignificant while p value less than 0.05 was considered significant and less than o.o1 was considered as highly significant. Receiver operator characteristic (ROC) analysis was used to explore the ability of urinary NGAL and urinary L-FABP to predict AKI within 48 hours when they were measured on admission, ROC curves are presented and the area under the curve (AUC) had been calculated. Sensitivity and specificity were reported for the best cutoffs. Pearson’s correlation coefficient (r) test was used to assess the strength of association between different values and NGAL.
3. Results
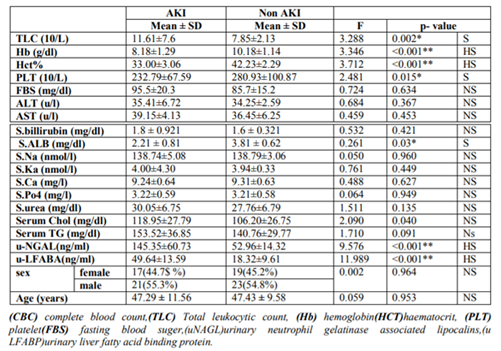
There was highly significant increase in mean u-NGAL (145.35±60.35)ng/ml in AKI group compared to u-NGAL (52.96±14.32) ng/ml in non AKI group. Also there is was highly significant increase in mean u-LFABP (49.64±13.59) ng/ml in AKI group in compared to mean u.-LFAB (18.32±9.61)ng/ml in non AKI patients (p< 0.001) (Table1). There was significant increase in mean TLC(11.61±7.6) x103 in AKI compared to mean TLC (7.85±2.13)x103 in non- AKI group.(p< 0.05).Table (1)
There was significant decrease in mean PLT (232.79±67.59)10/L in AKI group compared to mean PLT (280.93±100.87)10/L in non AKI group and highly significant decrease in mean Hb(8.18±1.29)g/dl and mean HCT (33.00±3.06) % in AKI compared to mean Hb (10.18±1.14) g/dl and mean HCT (42.23±2.29)% in non AKI group. Also there was significant decrease in mean serum albumin (2.21 ± 0.81) mg/dl in AKI compared to mean serum albumin (3.81 ± 0.62)mg/dl in non AKI group. while as regard FBS, CHO, TG, ALT, AST, bilirubin and electrolytes there was no statistically significant difference between AKI and non- AKI group. Table (1)
As regarding the causes of AKI there was 14 patients (36.8%) developed AKI due to sepsis, nine patients (23.7%) due to Hypoperfusion, five patient (13.2%) due to hepatorenal syndrome, three patient (7.9%) due to contrast exposure, 3 patient (7.9%) due to pre eclampsia, one patients (2.6%) due to Cardiorenal syndrome, one patient (2.6%)due to drug induced interstitial nephritis, one patient (2.6%) due to vasculitis and one patients (2.6%) due to Rhabdomyolysis.
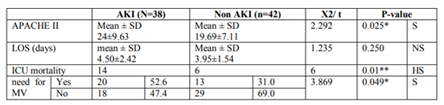
Table (2) showed there was significant increase in mean APACHE 11 score (24±9.63) in AKI compared to mean APACHE11 score (19.69±7.11) in non AKI (P< 0.05). While there was insignificant results in mean LOS (4.50±2.42) in AKI compared to mean LOS (3.95±1.54) in non AKI (p>0.05).Table 2 also showed highly significant difference between both group regarding incidence of ICU mortality (p< 0.01) and significant difference regarding need for mechanical ventilation (p< 0.05).
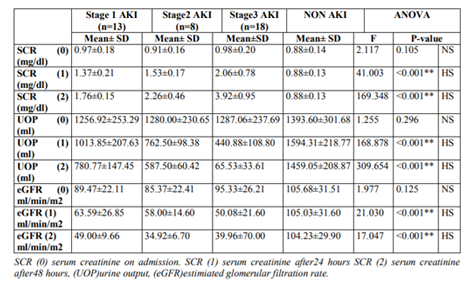
Table (3) showed that there was highly significant difference between non AKI-group and different stages of AKI regarding to serumcreatinine, UOP and GER. patients without AKI show the lowest mean serum creatinine in day 1,2 (0.88±0.13) ( 0.88±0.13) mg/dl, respectively followed by stage 1 AKI (1.37±0.21) ( (1.76±0.15)mg/dl ,followed by stage2(1.53±0.17) (2.26±0.46) mg/dl while the stage 3 show the highest serum creatinine in day 1,2(2.06±0.78)(3.92±0.95)mg/dl respectively (p< 0.001). As regarding UOP inday1,2 ,the non AKI was highest mean UOP (1594.31±218.77) (1459.05±208.87) ml, followed by stage1AKI (1013.85±207.63) (780.77±147.45) ml followed by stage2 (762.50±98.38) (587.50±60.42) ml , and stage 3 show the lowest mean UOP (440.88±108.80) (65.53±33.61) ml respectively (p< 0.001).as regarding GFR in (day1&2) the non AKI was highest mean GFR (105.03±31.60) (104±29.90) ml/min/m2, followed by stage 1AKI (63.59±26.85) (49.00±9.66) ml/ min/m2 followed by stage 2(58.00±14.60) (34.92±6.70) ml/min/m2 ,the stage3 AKI show the lowest mean GFR (50.08±21.20) (39.96±70.00) ml/min/m2 respectively. (p< 0.001) while no statistically significant result between both group as regard serum creatinine, UOP and eGFR on admission (p>0.05).
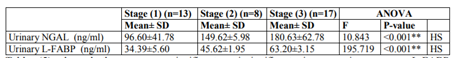
Table (4) showed that there was a highly significant increase between patients with different stages in AKI group regarding u-NGAL. Patients with Stage (1) showed the lowest urinary NGAL level (96.60±41.78) ng/ml, followed by Stage (2) (149.62±5.98) ng/ml while Stage (3) showed the highest urinary NGAL level (180.63±62.78) ng/ml (P< 0.001). Also there was highly significant difference between patients with different stages in AKI group regarding urinary L-FABP. Patients with Stage (1) showed the lowest urinary L-FABP level (34.39±5.60) ng/ml, followed by Stage (2) (45.62±1.95) ng/ml while Stage (3) showed the highest L-FABP level (63.20±3.15) ng/ml (p< 0.001).
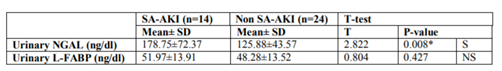
Table (5) showed there was a significant increase in mean u-NGAL(178.75±72.37) ng/ml in sepsis associated AKI patient compared to mean u-NGAL(125.88±43.57) ng/ml in non sepsis associated AKI (< 0.05). While there was insignificant increase in mean u-L-FABP (51.97±13.91) ng/ml in sepsis associated AKI compared to mean u L-FABP (48.28±13.52) ng/ml in non sepsis associated AKI (p> 0.05).
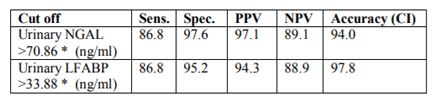
Table (6) showed that the area under curve at ROC analysis was 0.94 confidence interval (CI). The sensitivity of u-NGAL for diagnosis of AKI at cut off value 70.86ng/ml was 86.8%and specificity was 97.8%. Also the area under curve at ROC analysis was 0.97 CI. The sensitivity of urinary L-FABP for diagnosis of AKI at cut off value 33.88 ng/ml was 86.8%and specificity was 95.2%.
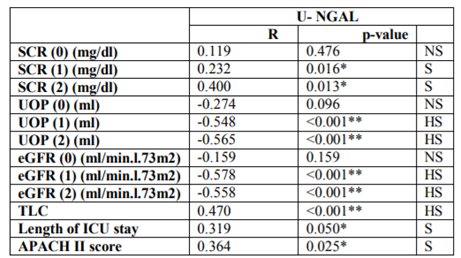
Table (7) showed there was significant positive correlation between urinary NGAL and both creatinine day (1),day (2), APACHE II and Length ICU stay, it shows also a highly significant negative correlation between urinary NGAL and both urine output and eGFR in day (1) and day (2).
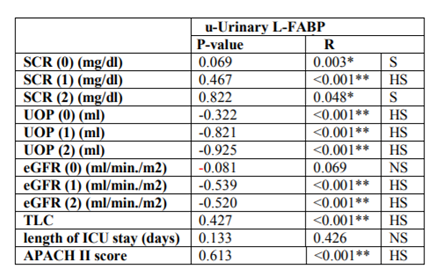
Table (8): showed there was significant positive Correlation between urinary L-FABP with serum creatinine day (0) and day (2) and highly significant positive Correlation with serum creatinine in day (1), TLC and APACHE II score. It shows also highly significant negative correlation between urinary L-FABP and eGFR in day (1) and day (2) and UOP in the three consecutive days, while non significant negative correlation between urinary L-FABP and eGFR in day (0) and non significant positive correlation between urinary L-FABP and length of ICU stay.
4. Discussion
The current study showed a highly significant increase in the mean of u-NGAL among AKI group when compared to non AKI group (p value< 0.001). u-NGAL was not only correlated with AKI, but also correlated with the degree of renal injury in conjunction with the (KIDGO criteria, 2012)[9].This result in consistent with Makris and his colleagues (2009)[10] who showed that highly significant increase in u-NGAL between AKI and non AKI in post-traumatic patients who were admitted to ICU and these higher levels persisted over the following 2 days. De Geus and his colleague.,(2011)[11]who assessed the ability of u-NGAL to predict severe AKI prospectively in a cohort of 632 critically ill patients through serial u-NGAL sampling (4,8,24,36,72 hours) and found that there was a significant association between patients u-NGAL levels on ICU admission and the final RIFLE class. Although serial u-NGAL measurements did not provide additional information for thepredictionof RIFLE.
Watanabe and his collegue (2014)[12]who assessed 83 patients admitted to the intensive care unit for clinical reasons and divided them into AKI and non AKI groups. U-NGAL was high in AKI group (p< 0.001) within the first 24 hours after admission and preceded the increase of serum creatinine in acute kidney injury patients.
NGAL is barely detectable in either plasma or urine in healthy kidney. However, in the setting of acute tubular injury, NGAL undergoes rapid and profound up regulation with large increases in both urine and plasma [13].
Our study showed that there was highly significant increase in the mean of L-FABP among AKI group when compared to non AKI group (p value< 0.001). Urinary L-FABP was not only correlated with AKI, but also it correlated with the degree of renal injury in conjunction with the (KIDGO criteria, 2012)[9].This result agreed with Doiand his collaegue (2011)[14] who measured 5 different urinary biomarkers (L-FABP, NGAL, cystatin C, IL-18 and albumin) in 339 critically ill adult patients on admission to a medical-surgical ICU of whom 131 developed AKI. They concluded that the best urinary biomarker to detect AKI was u.L-FABP. Cho and his colleague (2013)15, in their prospective observational study conducted over 145 patients (54 AKI and 91 non AKI), urinary L-FABP and NGAL measured at time of admission .They concluded that urinary L-FABP could be an adjunctive and independent biomarker for both the detection of AKI as well as the prediction of prognosis in heterogeneous ICU patients.
L-FABP is a newly emerging biomarker that has antioxidant properties. Enhanced expression of L-FABP in proximal tubular cells and subsequent urinary excretion are known to reflect the presence of tubular injury[15].
As regard serum creatinine, the current study showed a highly significant increase between different stages of AKI and non AKI-group in day 1 and 2 (after 24 and 48 hours respectively) but no significant difference in mean creatinine measured at time of ICU admission day (0).
These results compatible with Boghdady and his colleague (2013)[16]who reported that no statistically significant result between AKI and non AKI group at 0,12hours while a highly significant result after 48 hours of admission. But Ren and his colleague (2014) [17]found a highly significant difference between AKI and non AKI group as regard basal creatinine (pvalue < 0.01).
Our study showed that sepsis associated AKI patients had a significant rise in urinary NGAL levels than non septic patients while no significant difference between them as regard urinary L-FABP .
This result coincided with Martensson and his colleague (2010)[18]found that urine NGAL level was increased only in sepsis with AKI but was not increase in sepsis without AKI therefore, u-NGAL may be an index to evaluate whether sepsis will developed AKI.
Dai and his colleague (2015)[19]whoreported the usefulness of urine NGAL to predict septic AKI with area under curve (AUC) of 0.84 (95 % confidence interval (CI): 0.72 − 0.91) and 0.88 (95 % CI: 0.79–0.95), respectively. However, Vanmassenhove and his colleague (2015)[20] found that patients in sepsis without AKI, kidney tissue can also increase NGAL urinary excretion rate. The increased levels of u-NGAL can also be due to overspill from the systemic circulation, which render the discriminative value of NGAL as a biomarker for AKI in patients with sepsis to become blurred.
Our study showed that there is a significant increase of total lekocytic count in AKI when comparing to non AKI group (pvalue < 0.05) and this is in agreement with chang and his colleague (2014)4who studied 543 critically ill patients who admitted to ICU (187 AKI and 356 non- AKI) they proved that highly significant difference between mean total leukocytic count in AKI patients when comparing to non -AKI group (pvalue< 0.01).Which may be due to increase prevalence of sepsis in ICU patients.
Our study showed there was a significant decrease in hemoglobin between AKI and non-AKI group, this result agreed with Han and his collegue (2015)[21], in their retrospective analysis done over 2,145 ICU patients. They found that the risk of AKI was higher in the anemia group than the non-anemia group.
Anemia directly reduces oxygen delivery to the kidney. Because AKI frequently develops in the ischemic conditions, anemia can be one of reasons for the high incidence of AKI in hospital-admitted patients [21].
The current study showed significant decrease in serum albumin between AKI and non AKI group and this result was in agreement with Yu and his colleague (2017)[22]in his retrospective study which included 19.472 patients. Found that the incidence of AKI was 10.7% (340/3179) in the hypoalbuminmia group and 4.1% (662/16293) in the normoal buminemia group (P value= 0.005).
The current study showed that AKI patients has a higher mortality rate than non AKI patients as regard APACHE II mortality score (p value =0.025) also mortality increase with increase severity of AKI (p value < 0.001between different AKI stages) and so, AKI is considered a significant predictor for mortality .This result was agreed with. Samimagham and his colleague (2011)[23],Renand his colleague (2015)24 and Hashemian and his colleague (2016)25 who studied APACH II scores between AKI and non AKI with a highly significant mortality score and mortality rate in AKI than non AKI group (p=0.000). Mortality rate in patients with AKI was 13 times higher than those who did not develop AKI.
As regard length of stay in ICU (LOS), our study showed that no statistically significant result either between AKI and non AKI patients or between different stages of AKI .This result agreed with Reddy and his colleague (2014)[26] who studied 250 ICU patients and found non-significant difference in the mean of ICU LOS in patient with AKI when compared with non AKI patients (p-value 0.10).But our result disagreed with. Samimagham and his colleague (2011)23,Boghdadya and his colleague (2013)16 and, Hashemian and his colleague (2016)25 where there was a highly significant increase in the mean ICU stay of AKI patients than non AKI patients and longer ICU stay occur in AKI patients (p= 0.001) The variability in length of ICU stay in different studies is affected by various factors and associated comorbidities[27].
The current study showed a significant increase in need for mechanical ventilation between AKI and non-AKI group. Dos Santos and da Silva Magro201528 concluded that: the use of invasive mechanical ventilator support with positive end-expiratory pressure in critically ill patients in intensive care units can impair renal function.
According to receiver operating characteristic (ROC) analysis of sensitivity and specificity of urinary NGAL, the current study showed that the area under curve at ROC analysis was 0.94 CI. The sensitivity of u-NGAL for diagnosis of AKI at the time of ICU admission was 86.8% and specificity was97.6 % at cut off value of > 70.86 ng/ml.
According to receiver operating characteristic (ROC) analysis of sensitivity and specificity of urinary L-FABP, the current study showed that the area under curve at ROC analysis was 97.0CI. The sensitivity of urinary L-FABP for diagnosis of AKI at the time of ICU admission was 86.8% and specificity was95.2 % at cut off value of > 33.88 ng/ml. Various authors have reported different cut off values for urinary NGAL and L-FABP to early diagnose acute kidney injury.
Tecsonand his colleague (2017)[29]who reported that best cut-off value for U. NGAL for predictive diagnosis of AKI was 78.0/ml with AUC0.73%, sensitivity 78.8% and specifity 73%. Cho and his collegue (2013)15who reported that best cut-off value for L-FABP for predictive diagnosis of AKI was 28.45 ng/ml with AUC 0.780 (0.702-0.857), sensitivity 71.7% and specificity (75.8%).
The current study found significant positive correlation between u-NGAL and serum creatinine in day (1&2) and significant negative correlation between u-NGAL and UOP in day (1 & 2) and these results partially agreed with Watanabe and his colleague (2014)12 who studied 38 patients admitted to ICU and divided them to non-AKI (patient who did not developed AKI during stay in ICU),AKI (patient developed AKI during stay in ICU) and severe AKI (patient had AKI upon admission to ICU). He found that, in group AKI u-NGAL was negatively correlated with UOP at24 hours in severe AKI, u-NGAL was negatively correlated with UOP and positively correlated with serum creatinine at 24, 48 hours. He also agreed with our study in that no different in UOP between AKI (AKI & severe AKI) and non-AKI in the first 24 hours of ICU admission.
5. Conclusion
AKI in ICU have been associated significantly with increase morbidity and mortality even in mildest degree of AKI so the need for early diagnosis is mandatory. Urinary NGAL and L-FABP can be used as early biomarker for diagnosis of AKI in ICU patients.
Recommendation
Another multicenter studies covering large number of ICU patients to confirm our results. Repeat this study on a various cause of AKI separately. Follow up of patient who discharged from ICU over long period to detect development of CKD.
References
- Kokkoris S, Pipli C, Grapsa E et al. Novel biomarkers of acute kidney injuryin general adult ICU. Renal failure. 2013; 35: 4p579-91
- Shah SR,Tunio SA,Arshad MHet al. acute kidney injury recognition and management: areview of liitreture and clinical evidence. Global jornal of health science2016; 8(5)9736-9744
- Wonnacott A, Meran Sand Amphlett Betal. Epidemiology and outcomes in community-acquired versus hospital-acquired AKI. Clin J Am SocNephro2014;l9: 1007–1014
- Chang CH, Fan PC, Chang MY, et al. Acute Kidney injury Enhances Outcome predictability Ability of Sequential Organ Failure Assessment Score in Critically ill patients. PLoS One.2014; 9(10): e109649.
- ChuvaT,Maximino J, Barbosa J, et al. Haematological malignancies and acute kidney injury requiring nephrology consultation: challenging the worst of the worst Clin Kidney J. 2016 Jun; 9(3): 418–423.
- Lopes JA and Jorge S. The RIFLE and AKIN classification for Acute Kidney injury: a critical and Comprehensive review. Clin Kidney J. 2013; 6 (1): 8-14.
- Sanjeevani S, Pruthi S, Kalra S, et al. Role of neutrophil gelatinase-associated lipocalin for early detection of acute kidney injury. Int J CritIllnInjSci 2014; 4: 223-22.
- Matsui K, Kamijo-Ikemori A, Sugaya T, et al. Usefulness of Urinary Biomarkers in Early Detection of Acute Kidney Injury After Cardiac Surgery in Adults. Circ J. 2012; 76: 213–220.
- KDIGO Clinical Practice Guideline on Acute Kidney Injury. Kidney Int Suppl. 2012; 2: 6–138.
- Makris K, Markou N, Evodia E, et al. A. Urinary neutrophil gelatinase-associated lipocalin (NGAL) as an early marker of acute kidney injury in critically ill multiple trauma patients. ClinChem Lab Med 2009; 47: 79-82.
- De Geus HR, Bakker J, Lesaff re EM, et al. Neutrophil gelatinase associated lipocalin at ICU admission predicts for acute kidney injury in adult patients. Am J RespirCrit Care Med 2011, 183: 907-914.
- Watanabe M, Fulan e Silva G, Dezoti da Fonseca,etal. Urinary NGAL in patients with and without acute kidney injury in a cardiology intensive care unit. Rev Bras TerIntensiva. 2014 Oct-Dec; 26(4): 347–354.
- Malyszko J: Biomarkers of acute kidney injury in different clinical settings: a time to change the paradigm. Kidney Blood Press Res 2010; 33: 368-382.
- Doi K, Negishi K, Ishizu T, et al. Evaluation of new acute kidney injury biomarkers in a mixedintensive care unit. Crit Care Med 2011, 39: 2464-2469.
- Cho E, Yang H, Jo S, et al., The Role of Urinary Liver-Type Fatty Acid-Binding Protein in Critically Ill Patients J Korean Med Sci. 2013; 28(1): 100– 105.
- Boghdady IM, EL Naggar MM, Emara MM, et al. Kidney injury molecule-1 as an early marker for acute kidney injury in critically ill patients. Menufia medical journal. 2013; (26): 2. 98-104
- RenH, Zhou X,DaiDet al. Assessment of urinary kidney injury molecule-1 and interleukin-18 in the early post-burn period to predict acute kidney injury for various degrees of burn injury. BMC Nephrology; 2014: 16: 142.
- Martensson J, Bell M, Oldner A, et al. Neutrophil gelatinase-associated lipocalin in adult septic patients with and without acute kidney injury. Intensive Care Med 2010; 36: 1333-1340.
- Dai X, Zeng Z, Fu C, et al..Diagnostic value of neutrophil gelatinase-associated lipocalin, cystatin C, and soluble triggering receptor expressed on myeloid cells-1 in critically ill patients with sepsis-associated acute kidney injury. Crit Care. 2015; 19: 223.
- Vanmassenhove J, Glorieux G, Lameire N et al., Influence of severity of illness on neutrophil gelatinase-associated lipocalin performance as a marker of acute kidney injury: A prospective cohort study of patients with sepsis. BMC Nephrol 2015; 16: 18.
- Han SS, BaekSH , AhnSY,et al. anemia is arisk factor for acute kidney injury and long term mortality I critically ill patients. Tohoku journal of expirmentalmedicine ; 2015: (237). 4 p287-295.
- Yu M, Lee S, Baek s et al. Hypoalbuminemia at admission predicts the development of acute kidney injury in hospitalized patients: A retrospective cohort study. PLoS ONE. 2017; 12(7): e0180750.
- Samimagham HR, Kheirkhah S, Haghighi A et al. Acute kidney injury in intensive care unit: incidence, risk factors and mortality rate. Saudi J Kidney Dis Transpl 2011; 22: 464-70.
- Ren H, Zhou X,DaiDet al. Assessment of urinary kidney injury molecule-1 and interleukin-18 in the early post-burn period to predict acute kidney injury for various degrees of burn injury. BMC Nephrology; 2015: 16: 142.
- Hashemian SM, Jamaati H, Bidgoli FB, et al.Outcome of Acute Kidney Injury in Critical Care Unit, Based on AKI Network. Tanaffos. 2016; 15(2): 89-95.
- Reddy NK, Ravi K. P., Dhanalakshmi P et al. Epidemiology, outcomes and validation of RIFLE and AKIN criteria in acute kidney injury (AKI) in critically ill patients: Indian perspective, Renal Failure, ; 2014: 36: 6, 831-837.
- Gruenberg DA, Wayne Shelton, Susannah L. Rose, MSSW; Ann E. Rutter, MS; Sophia Socaris, Glenn McGee, Factors influencing length of stay in the intensive care unit. Am J Crit Care. 2006; 15(5):502-509.
- Dos Santos LL and da Silva Magro M. Mechanical ventilation and acute kidney injury in patients in the intensive care unit: Universidade de Brasília, Brasília, DF, Brazi Actapaul. Enferm; 2015: vol. 28 no. 2
- Tecson KM, Erhardtsen E, Eriksen PM et al. Optimal cut points of plasma and urine neutrophil gelatinase-associated lipocalin for the prediction of acute kidney injury among critically ill adults: retrospective determination and clinical validation of a prospective multicentre study, BMJ. 2017; (7): 7