Information
Journal Policies
Extreme Hydronephrosis or Multicystic Dysplastic Kidney: Still Diagnostic Dilemma
Stanislaw Warchol1*,Grazyna Krzemien2,Agnieszka Szmigielska2,Przemyslaw Bombinski3,Krzysztof Toth4,Teresa Dudek - Warchol1
2.Department of Pediatrics and Nephrology, Medical University of Warsaw, 02-091 Warsaw, Zwirki&Wigury street 63a, Poland.
3.Department of Pediatric Radiology, Medical University of Warsaw, 02-091 Warsaw, Zwirki&Wigury street 63a, Poland.
4.Nuclear Medicine Laboratory Nukleomed, Warsaw 04-736, Zeganska street 46 a, Poland.
Copyright : © 2017 . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Multicystic dysplastic kidney (MCDK) is estimated as anomaly easy to diagnose, because of its characteristic ultrasound picture. Usually advocated imaging studies to establish the diagnosis of MCDK suspected prenatally, include postnatal ultrasound examination as well as radionuclide scan to show the lack of kidney function, however, the need for confirmatory scintigraphy still is discussed. Ultrasonographically large hydronephrosis in the newborn with extremely dilated renal collecting system and very narrowed, almost invisible renal parenchyma is very similar to the picture of multicystic kidney. In such cases it is very difficult to differentiate between MCDK and giant hydronephrosis only with the ultrasound alone. We report 2 cases of infants with extreme hydronephrosis initially diagnosed as MCDK and present completely different clinical course. Early operative treatment of obstructed, extreme hydronephrosis helps to salvage the kidney and achieve acceptable clinical outcome. It seems that radionuclide renogram still is valuable imaging study in a child with ultrasound picture of multicystic dysplastic kidney to complete diagnosis.
neonatal hydronephrosis, multicystic dysplastic kidney, radionuclide renography, pyeloplasty, Nephrology
1. Introduction
A multicystic dysplastic kidney (MCDK), a form of renal dysplasia, represents non-functioning organ due to abnormal kidney development. The incidence of prenatal diagnosis of MCDK is still rising, confirmed within the newborn period by postnatal ultrasound examination [1-4]. Imaging work-up usually employed in cases of MCDK include ultrasound examination (US) and confirmatory nuclear medicine scan. The advisability and usefulness of radionuclide study to show the absence of renal function in MCDK as well the time to perform such study, still is discussed and somewhat controversial [4-9]. The aim of the present study was to present 2 cases of infants with extreme hydronephrosis diagnosed initially as multicystic dysplastic kidney to discuss diagnostic dilemma, completely different clinical course and results of treatment.
2. Material And Methods
During the last 5 years two infants were treated because of large hydronephrosis due to congenital ureteropelvic junction obstruction, initially diagnosed as MCDK.
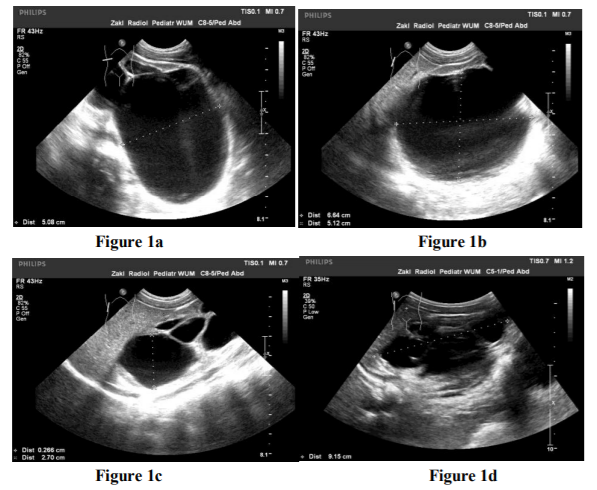
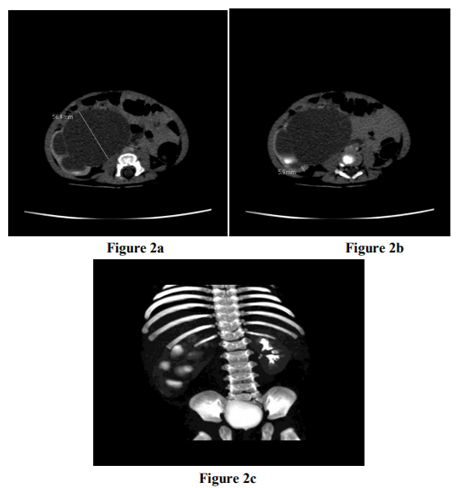
3-months old male with prenatally diagnosed right MCDK confirmed postnatally ultra sonographically was referred for urologic evaluation, because control ultrasound performed at the age of 3-months to evaluate the regression of the size of cysts, was described as large hydronephrosis (Figure 1a, b, c, d). Computed tomography urography (Figure 2a, b, c) confirmed the diagnosis of extreme hydronephrosis due to ureteropelvic junction obstruction.
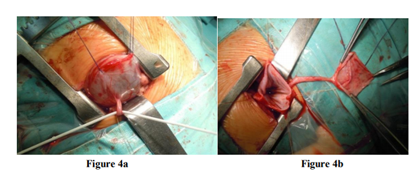
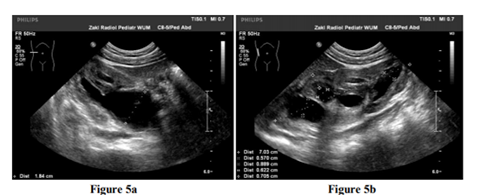
Dynamic scintigraphy (Figure 3 a,b,c) showed giant right hydronephrosis with almost completely obstructed ureteropelvic junction and grossly diminished renal function (21% of differential renal function). An infant was operated on emergency basis – intraoperatively long distance ureteropelvic junction obstruction was found and dismembered Hynes- Anderson pyeloplasty was done (Figure 4 a, b). During 5 year follow-up gradually decrease of dilatation degree of the right collecting system was noted on US (Figure 5 a,b) while dynamic scintigraphy (Figure 6 a,b,c) showed permanent improvement of drainage together with better right renal function (up to 31%).
6-months old female with diagnosed prenatally left MCDK underwent imaging studies because of urinary tract infection at the age of 5 months. Only one confirmatory ultrasound study was done immediately after the birth and the next one was advised by neonatologist after one year of life. Ultrasound revealed large left hydronephrosis, voiding cystourethrography right reflux grade IV and also reflux to the left ureter, radionuclide study practically no function of the left kidney (5%). As the first step of treatment left nephroureterectomy was done and later at the age of 2 years persisting right reflux grade III was successfully corrected endoscopically.
3. Discussion
Usually advocated imaging studies to establish the diagnosis of multicystic dysplastic kidney suspected prenatally, include postnatal ultrasound examination as well as radionuclide scan to show the lack of the kidney function. The value of scintigraphy, however, is still debated, because MCDK with its characteristic ultrasound picture is estimated as anomaly easy to detect and diagnose [4-8]. Typical ultrasound features of MCDK include: cysts of variable size and shape, an absent reniform appearance and the absence of centrally located cyst [5-7]. Large hydronephrosis in the newborn with extremely dilated pelvis and calyces together with very narrowed, almost invisible renal parenchyma, however, is very similar to the picture of multicystic kidney. In such instances it is very difficult to differentiate between MCDK and giant hydronephrosis only with the ultrasound alone [8,10-14].
As those two diagnoses: MCDK and large hydronephrosis vary greatly in the treatment recommendations – surgical intervention for large, obstructed hydronephrosis versus observation for MCDK – making the correct diagnosis is of utmost importance [2,4,8,12,13,15].
Conservative, non-surgical management is the preferred and recommended approach to MCDK. Children with MCDKs very rarely require operative intervention [8,16,17] and routinely are followed with repeated renal ultrasound to confirm progressive involution of cysts, however, involution before adulthood is unpredictable [2,3,15,18-20].
On the other hand, in the majority of newborns and infants with congenital hydronephrosis due to ureteropelvic junction obstruction, diagnosed prenatally and confirmed postnatally, operative treatment is not usually necessary immediately after diagnosis, with one exception. Obstructive, large hydronephrosis with preserved renal function (as estimated by radionuclide study) require prompt surgical correction on emergency basis to salvage the kidney [11-14].
Our observation showed clearly that ultrasound imaging alone is not sufficient to differentiate between MCDK and large hydronephrosis with extremely dilated calyces and renal pelvis, even when ultrasound examination is performed by experienced radiologist. The clinical course of reported 2 infants with prenatally diagnosed multicystic dysplastic kidney, confirmed postnatally and delayed final diagnosis of large hydronephrosis, clearly confirm the value of nuclear scan to rule out potential obstructive hydronephrosis with preserved renal function amenable for surgical correction.
4. Conclusion
Ultrasound picture of multicystic dysplastic kidney may be very similar to that of extreme hydronephrosis, and sometimes can pose diagnostic dilemma. Early operative treatment of obstructed, extreme hydronephrosis helps to salvage of the kidney and achieve acceptable clinical outcome. It seems that radio nuclide renogram still is valuable imaging study in a child with ultrasound picture of multicystic dysplastic kidney to complete diagnosis.
References
- Schreuder MF, Westland R, van Wijk JAE. Unilateral multicystic dysplastic kidney: a meta-analysis of observational studies on the incidence, associated urinary tract malformations and the contralateral kidney. Nephrol Dial Transplant. 2009; 24:1810-1818.
- Aslam M, Watson AR, on behalf of the Trent&Anglia MCDK Study Group. Unilateral multicystic dysplastic kidney: long term outcomes. Arch Did Child 2006; 91:820-823.
- Eickmeyer AB, Casanova NF, He C, Smith EA, Wan J, Bloom DA, Dilmann JR. The natural history of the multicystic dysplastic kidney – is limited follow-up warranted? J Pediatr Urol. 2014:10:655-661.
- Hains DS, Bates CM, Ingraham S, Schwaderer AL. Management and etiology of the unilateral multicystic dysplastic kidney: a review. Pediatr Nephrol. 2009; 24:233-241.
- Whittam BM, Calaway A, Szymanski KM, Carroll AE, Misseri R, Kaefer M, Rink RC, Karmazyn B, Cain MP. Ultrasound diagnosis of multicystic dysplastic kidney: is a confirmatory nuclear medicine scan necessary? J Pediatr Urol. 2014; 10:1059-1062.
- Hollowell JG, Kogan BA.How much imaging is necessary in patients with multicystic dysplastic kidneys? J Urol. 2011;186:785-786
- Sarahan OM, Alghanbar M, Alsulaihim A, Alharbi B, Alotay A, Nakshabandi Z. Multicystic dysplastic kidney: impact of imaging modality selection on the initial management and prognosis. J Pediatr Urol. 2014; 10:645-649.
- Psooy K, in collaboration with the Pediatric Urologists of Canada (PUC). Multicystic dysplastic kidney (MCDK) in the neonate: the role of the urologist. Can Urol Assoc J. 2016; 10:18-24.
- Carazo-Palacios ME, Couselo-Jerez M, Serrano-Durba A, Pemartin-Comella B, Sanguesa- Nebot C, Estornell- Moragues F, Dominguez-Hinarejos C. Multicystic dysplastic kidney: assessment of the need for renal scintigraphy and the safety of conservative treatment. [Article in English, Spanish]. Actas Urol Esp. 2016; doi: 10.1016 /j.acuro. 2016. 05. 004.
- Debnath J, Roy S, Sahoo SK, Pandit A. Congenital giant hydronephrosis: a rare cause for upper abdominal mass in the newborn. J ClinNeonatol 2013; 2:33-35
- Ismaili K, Piepsz A. The antenatally detected pelvi-ureteric junction stenosis: advances in renography and strategy of management. Pediatr Radiol. 2013; 43:428-435.
- Vemulakonda V, Yirr J, Wilcox DT. Prenatal hydronephrosis: postnatal evaluation and management. Curr Urol Rep. 2014; 15:430-436.
- Shimada K, Matsumoto F, Kawagoe M, Matsui F. Urological emergency in neonates with congenital hydronephrosis. Int J Urol. 2007; 14: 388-392.
- Piepsz A. Antenatally detected hydronephrosis. Semi Nucl Med. 2001; 37:249-260
- Cambio AJ, Evans ChP, Kurzrock EA. Non-surgical management of multicystic dysplastic kidney. BJU International. 2008; 101 :804-808.
- Kumar M, Gathwala G, Rattan KN, Lather S, Poonam D. Congenital giant dysplastic kidney presenting as respiratory distress: a case report. J Neonat Surg. 2017; 6:15
- Yadav P, Sureka KS, Ansari MS, Soni R, Lal H. Large multicystic dysplastic kidney mimicking a large cystic renal neoplasm. J Clin Diag Res. 2017; 11:PD03-PD04, doi: 10.7860 /JCDR / 2017/24226.9887
- Weinstein A, Goodman TR, Iragorri S.Simple multicystic dysplastic kidney disease: end points for subspeciality follow-up. Pediatr Nephrol. 2008; 23:111-116.
- Hayes WN, Watson AR, Trent&Anglia MCDK Study Group. Unilateral multicystic dysplastic kidney: does initial size matter? Pediatr Nephrol. 2012; 27:1335-1340.
- Tiryaki S, Alkac AY, Serdaroglu E, Bak M, Avanoglu A, Ulman I.Involution of multicystic dysplastic kidney: is it predictable? J Pediatr Urol. 2013; 9:344-347.