Information
Journal Policies
Revisiting Acute Kidney Injury in Minimal Change Disease a Case Report and Review of Literature
Dr.Tena Abraham1,Dr.Shobhana Nayak-Rao2,Dr.Pradeep Shenoy M3
2.Associate Prof and Head, Dept of Nephrology, K.S. Hegde Medical Academy, Medical Sciences Complex, Derlakatte Mangalore, Karnataka, INDIA.
3Assistant Prof, Dept of Nephrology. K.S. Hegde Medical Academy, Medical Sciences Complex, Derlakatte Mangalore, Karnataka, INDIA.
Copyright : © 2017 . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
The occurrence of renal failure has been believed to be a common complication of nephrotic syndrome associated with minimal change disease in children. In adults though, it has been relatively more infrequently documented than in children. Acute kidney injury (AKI) has been described in nephrotic syndrome in literature and has been associated with older age, systolic hypertension, vascular disease and increasing severity of nephrotic syndrome. The underlying pathophysiology responsible for the reduction of glomerular filtration rate (GFR) has been a matter of debate. We present a case of an elderly patient who presented with worsening renal failure and review the available literature on this entity of AKI in adult minimal change nephrotic syndrome.
Minimal change disease, nephrotic syndrome, adult, renal failure,Nephrology
1. Introduction
The occurrence of renal failure has been believed to be a common complication of nephrotic syndrome associated with minimal change disease in children. In adults though, it has been relatively more infrequently documented than in children. Acute kidney injury (AKI) has been described in nephrotic syndrome in literature since 1966 with more than 85 cases reported so far[1,2]. It has been associated with older age, systolic hypertension, vascular disease and increasing severity of nephrotic syndrome [3,4]. The underlying pathophysiology responsible for the reduction of glomerular filtration rate (GFR) has been proposed by Lowenstein et al [5] to be due to interstitial oedema of kidney also termed as nephrosarca causing vascular or tubular occlusion and a subsequent filtration failure. However this has been debated in some reports and other mechanisms have been proposed [6]. We present a case of an elderly patient who presented with worsening renal failure and review the available literature on this entity of AKI in adult minimal change nephrotic syndrome including the known pathogenetic mechanisms that lead to renal failure in these patients and also look at the outcome of patients who develop AKI during the course of the illness.
A 75 year old male without any significant past medical history presented to us with one week history of progressive swelling of hands and feet and weight gain of > 10 kgs in the previous two weeks prior to admission. He had also noted slightly decreased urinary frequency and quantity of urine during this period. He did not report any preceeding h/o sore throat, arthralgia, myalgia, skin rashes, hematuria, dysuria or h/o any ingestion of any NSAID’s or any other alternative medication use. The patient did not smoke or consume alcohol. Physical examination revealed an elderly male weighing 67 kgs (previous recorded weight 55 kgs ) , blood pressure of 150/90mm of Hg, pulse rate of 82/min, respiratory rate 18/min. There were 3+ pitting edema till upper thighs and sacral edema. There were no skin rashes or lymphadenopathy and all pulses were equally felt. Other than decreased breath sounds at both lung bases, the remainder of the physical examination was unremarkable. On admission, his blood urea 67mg/dl, with a serum creatinine of 1.6mg/dl with normal serum electrolytes. Urine analysis at presentation had 4+ proteins, 5-10 WBC/HPF, no RBC and no casts. Hematology investigations revealed hemoglobin of 1.3gm/dl, total WBC count of 11,000/cmm, normal differential and platelet counts. An ultrasound abdomen did not reveal any organomegaly, normal kidney size (RK10.2X3.2cms, LK 11.0X3.cms) with normal cortical echogenicity and no hydronephrosis. Total serum protein was reduced at 4.5gm/dl with serum albumin 2.1gm/dl. A 24 hr urinary protein revealed 4.2 gms of protein with estimated creatinine clearance of 2.7ml/min. A complete serological work-up including serum complement C3,C4 ,antinuclear antibody, anticytoplasmic antibody , anti HIV,HCV and hepatitis B antibody were negative.
A percutaneous renal biopsy was performed one day after admission and this included a total of 15 glomeruli with no sclerosed glomeruli. The glomeruli were normal in size and appearance on light microscopy with no focal or segmental sclerosis and mild vascular intimal hyperplasia. The interstitial space revealed mild focal tubular injury, no tubular fibrosis or atrophy was noted. Immuno flouresence of the specimen revealed 11 viable glomeruli and was negative for IgG, IgA, IgM, C3, C1q, kappa and lambda chains.
A diagnosis of minimal change disease with mild acute tubular injury was made and treatment was started with prednisolone 1mg/kg daily basis. Over the next two weeks after admission and treatment initiation, the PCV progressed to 9.09mg/dl with drop in estimated GFR to 5.7ml/min. Volume overload persisted despite albumin infusions, salt and water restriction and use of loop diuretics. Hemodialysis was initiated on day 10 of hospitalization. At this time, the patients’s weight had climbed up to 75 kgs and he was mildly dysnoeic. He required a total of 15 litres of ultra filtration before he was deemed to have achieved dry weight. Hemodialysis was continued for 4 weeks. The proteinuria and renal functions slowly improved after 5-6 weeks of prednisone therapy and at the time of hemo - dialysis discontinuation, the endogenous Cr Cl was 15.7ml/min. The patient continues to be on steroid therapy at last follow-up at 3 months with serum creatinine of 3.0 mg/dl and he is off dialysis. The last estimated 24 hr protein is >1gm/day. A summary of relevant clinical data is presented in Table 1.
2. Discussion
The phenomenon of acute renal failure in nephrotic syndrome with normal or near normal structure was first described in detail by Chamberlain et al way back in 1966[7]. This initial report described nine cases of oliguric renal failure occurring unexpectedly in the course of nephrotic syndrome though renal pathology revealed a range of glomerular diseases. Since then several case reports and case series have reported reversible acute renal failure in patients presenting with nephrotic syndrome with minimal change disease on renal histology[1,4,5,20,21]. It is however relatively uncommon when compared to the classic presentation of nephrotic syndrome with preserved glomerular filtration rate (GFR). Information on the pathophysiology that underlies acute renal failure has been varied and distinct.
Since the first report by Chamberlain et al, many investigators have suggested that a reduction in effective intravascular volume induced by a lower plasma oncotic pressure and interstitial fluid space seeping leads to a fall in GFR leading to renal dysfunction. However this pathophysiologic mechanism has not been accepted by other investigators who have proposed different mechanisms. We review the current thinking on this entity. The major factors that regulate GFR are: circulating blood volume, renal blood flow and the intrinsic determinants of single nephron GFR.
Blood Volume in nephrotic syndrome: The traditional view of the pathogenesis of oedema formation in the nephrotic syndrome was that low plasma oncotic pressure resulting from hypoalbuminaemia would activate Starlings’ forces favouring transudation of plasma fluid into the interstitial space. The resulting decrease in effective intravascular circulating volume would then trigger volume-regulatorysensors to cause sodium and water retention by the kidneys. This view was however challenged by Eisenberg in 1968 who demonstrated that blood volume was normal in edematous nephrotic syndrome patients [8]. Other subsequent studies have also supported Eisenberg’s hypothesis that with certain exceptions, no demonstrable difference existed between circulating blood /plasma volume in nephrotic and normal individuals [9,10]. However observations of normal volumes should not be taken as proof that minor degrees of hypovolemia do not exist. There is little doubt however that in the majority of patients, blood volume is normal or even slightly expanded during full-blown relapse when oedema formation is maximal. Other mechanisms that increase total effective circulating blood volume results from enhanced proximal tubular reabsorption of sodium , non-osmotic secretion of AVP and activation of the symphathetic nervous system (SNS) and the renin angiotensin aldosterone system [11,12].
Renal blood blood flow is minimal change nephrotic syndrome has been estimated from para –aminohippurate (PAH) clearance technique. In most nephrotic patients, renal blood flow appears to be normal or only slightly reduced. Because plasma flow is normal and GFR often moderately reduced, the filtration faction (FF) is characteristically low. This observation of low FF in nephrotic syndrome is surprising and argues against the traditional hypothesis of hypovolemia in nephrotic syndrome. In other conditions of reduction in absolute or effective blood volume such as hemorrhage, congestive cardiac failure etc. the GFR is better preserved than renal blood flow resulting in an increase in FF. The low FF then in nephrotic syndrome must indicate a primary renal defect in the regulation of GFR.
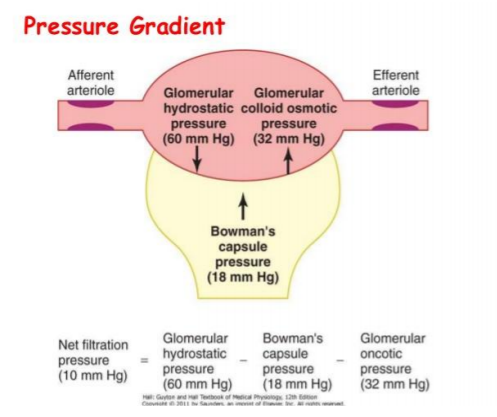
As shown in Figure 1, other factors may affect single nephron GFR in patients with nephrotic syndrome. This could be a decrease in Δ P (transcapillary hydraulic pressure) due to an increase in Pf (tubular hydrostatic pressure), primary reduction in Kf (ultrafiltration co-efficient), either by a reduction in the glomerular surface available for filtration or by an change in glomerular water permeability or both.
Renal interstitial edema/ nephrosarca - Lowenstein and co-workers proposed that intense extravasation of fluid into the renal interstitium actually caused renal failure [5]. Numerous pathological reports have also commented on renal interstitial oedema [3,5] or nephrosarca as a cause of increased interstitial pressure altering the glomerular hemodynamics and causing a reduction in single nephron GFR. The accumulation of high protein fluid into the interstitium along with a primary problem in renal lymphatic drainage results in severe interstitial oedema. However not all patients have evidence of interstitial oedema on biopsy [2,4,6]. Cameron et al [6] have made the case that improvement in GFR is not however related to loss of fluid but rather with the resolution of proteinuria and argue against the nephrosarca hypothesis.
The majority of renal biopsies in patients with minimal change disease and acute renal failure show changes of ischemic tubular damage [4]. Dilatation of tubules with flattening of the tubular epithelium and loss of brush border may be seen. Features of acute tubular necrosis (ATN) such as significant epithelial cell necrosis and tubular obstruction by proteinaceous casts are rare but possibly more common in children. The use of diuretics has been implicated in causing impaired perfusion and precipitating ATN [2,14]. Different studies have found varying prevalence of AKI in patients with adults minimal change disease. Haas et al found in retrospective analysis of elderly patients (>60ys) who had renal biopsies done for AKI, 7.5% had nephrotic syndrome with ATN as a diagnosis [15]. Waldman et al [16] also in a review of 95 adults with minimal change disease found that 24(25.2%) has acute renal failure .In 17 patients it was concurrent with the initial presentation of proteinuria while in 7 patients, it occurred at relapse. The study also found that male, older, hypertensive patients were more likely to develop AKI. Incidence of AKI also increased with greater proteinuria and lower serum albumin. Mean time to recovery of renal function was 6.4±2.0 wks. Elderly patients may be at more risk of renal dysfunction given the nephron loos and loss of cortical volume with aging [17]. Chen et al [18] also found the corroborated the same risk factors in their study. Keskar et al [19] also found that 22.9% of adolescents and adults with minimal-change disease in their study presented with AKI and all but 2/61 patients failed to recover. In another recent study by Maas et al [20] , AKI was observed in 40% of patients with minimal change disease. Response of nephrotic syndrome to first line therapy with steroids and achievement of complete remission can be longer in AKI patients than in patients without AKI [21]. In a single center study by Komukai et al, 27 (37.7%) out of 53 patients with biopsy proven first onset MCNS were evaluated. The median time to complete remission (CR) was significantly longer in patients with AKI at presentation.
However , renal failure in most if not cases recovers completely and progression to end stage renal disease occurs in only those few patients whose initial biopsies show changes of focal segmental glomerulosclerosis. The long term renal prognosis of childhood onset MCD has therefore been excellent and most patients have long disease free periods [21]. Progression to ESRD is rare and is more often in those with FSGS on initial or subsequent biopsies. The long term outlook for adult patients especially the elderly with pre-existing medical conditions presenting with AKI while generally good is difficult to define and further long term follow-up studies specifically addressing this issue are necessary. It is also not known that this stage if different treatment regimens correlate with better recovery of renal function and are yet to be defined.
References
- Smith JD, Hayslett JP. Reversible renal failure in the nephrotic syndrome. Is J Kidney Dis 1992; 19: 201-213.
- Furuya R, Kumagai H, Ikegaya N et al. Reversible acute renal failure in idiopathic nephrotic syndrome. Intern Med 1993; 32: 31-35.
- Esparza AR, Kahn SI, Garella S, Abuelo JG. Spectrum of acute renal failure in nephrotic syndrome with minimal (or minor) glomerular lesions. Lab Invest 1981; 45: 510-521.
- Jennett JC, Falk RJ. Adult minimal change glomerulopathy with acute renal failure. Am J Kidney Dis 1990; 16: 432-437.
- Lowenstein J, Schacht RG, Baldwin DS. Renal failure in minimal change nephrotic syndrome. Is J Med 1981; 70: 227-233.
- Cameron MA, Peri U, Rogers TE, Moe OW. Minimal change disease with acute renal failure: a case against the nephrosarca hypothesis. Neph Dial Transplant 2004; 19: 2642-46.
- Chamberlain MJ, Pringle A, Wrong QM. Oliguric renal failure in the nephrotic syndrome. Q J Med 1966; 138: 215-235.
- Eisenberg S. Blood volume in persons with the nephrotic syndrome. Am J Med Sci 1968; 255: 320-26
- Geers AB, Koomans HA, Ross JC et al. Functional relationships in the nephrotic syndrome. Kidney Int 1984; 26: 324-330.
- Fadnes HO, Pape HF, Sundsfjord JA. A study in oedema mechanism in nephrotic syndrome. Scan J Clin Lab Invest 1986; 46: 533-538.
- Usberti M, Federico S, Meccariello S et al. Role of plasma vasopressin in the impairment of water excretion in nephrotic syndrome. Kidney Int 1984; 25: 422-429.
- Brown EA, Markandu ND, Roulston JE. Is the renin angiotensin –aldosterone system involved in the sodium retention in the nephrotic syndrome Nephron 1982; 32: 102-107.
- Koomans HA, Boer WH, Dorhout Mees AJ. Renal function during recovery from minimal lesions nephrotic syndrome. Nephron 1987; 47: 173-78.
- Loghman-Adham M, Siegler RL, Pyscher TJ. Acute renal failure in idiopathic nephrotic syndrome. Clin Nephrol 1997; 47: 76-80.
- Haas M, Spargo BH, Wit E-JC, Meehan SM. Etiologies and outcome of acute renal insufficiency in older adults: A renal biopsy study of 259 cases. Am J Kidney Dis 2000; 35: 443-447.
- Waldman M, Crew JR, Valeri A et al. Adult minimal change disease: Clinical characeristics,Treatment and outcome. Clin J Am Soc Nephrol 2007; 2: 445-453.
- Denic A, Lieske JC, Chakkera PA. The substantial loss of nephrons in Healthy Human Kidneys with Aging. J Am Soc Nephrol ; 2017; 28(1): 313-20.
- Chen T, Lv Y, Lin F, Zhu J. Acute kidney injury in adult idiopathic nephrotic syndrome. Ren Fail 2011; 33(2): 144-9.
- Keskar V, Jamale TK, Kulkarni MJ, Jagadish PK, Fernades G, Hase N. Minimal –change disease in adolescents and adults: epidemiology and therapeutic resposne. Clin Kidney J 2013;6: 469-72.
- Maas RJ, Deegens JK, Beukhof JR et al. The clinical course of minimal change nephrotic syndrome with onset in Adulthood or late Adolescence: A case series. Am J Kidney Dis 2017; 69(5):637-646.
- Komukai D, Hasegawa T, Kaneshima N et al. Influence of acute kidney injury on the time to complete remission in adult minimal change nephrotic syndrome: a single-centre study. Nephrology (Carlton) 2016; 21(10): 887-92.