Information
Journal Policies
ARC Journal of Nephrology
Volume-1 Issue-1, 2016, Page No: 11-15
Fever In ESRD; Does It Worth A Second Look?
Dr. Ahmed Yehia 1, Dr. Omar Ballut 1, Alaa Sabry 2
Sur Hospital, South Sharqiya Region Sultanate of Oman.
Professor, Mansoura University, Egypt.
Professor, Mansoura University, Egypt.
Citation : Yehia A, Ballut O, Sabry A. Fever In ESRD; Does It Worth A Second Look? ARC Journal of Nephrology. 2016;1(1):11–15.
Copyright : © 2016 Yehia A. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
End Stage Renal Disease (ESRD) patients are liable for infections due to both their low immunity in comparison to general population and specific causes (i.e. recurrent central venous access needed for dialysis). So, it is logic to think about infection if a hemodialysis patient is presenting with fever. Here, we present five cases presented with fever and in spite of that, all their septic screens were negative, finally all of them turned out to have hematoma of different sizes and locations. Fever was persistent in spite of broad spectrum antibiotics given and resolved only after resolution of the hematoma.
CASE 1
A Sixty Seven years old Saudi male known to have End Stage Renal Disease (ESRD) secondaryto Diabetes Mellitus (DM) and Hypertension on regular hemodialysis (HD) for few months, he had thrombosis of his Arterio-venous Fistula (AVF) and malfunctioning temporary catheter. Permanent dialysis catheter was needed to minimize the rate of infection till creation of new AVF.
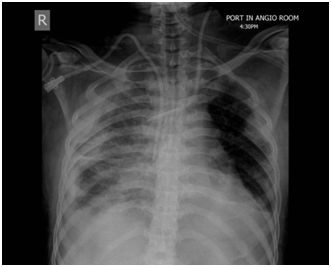
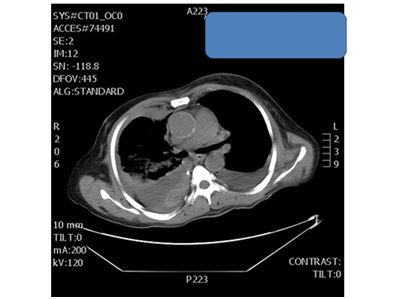
During insertion of the permanent catheter, suddenly the patient had severe chest pain and dyspnea. Chest x-ray (figure 1) and CT (figure 2) were done and the patient was shifted to ICU, chest tube was inserted and pure blood was drained.
Hemoglobin level dropped from 11.2 gm/dl to 7.8 gm/dl over 7 days. He received 5 units of Packed Red Blood Cells (PRBCs) together with Fresh Frozen Plasma (FFP). Femoral catheter was inserted for HD and permanent catheter was removed.
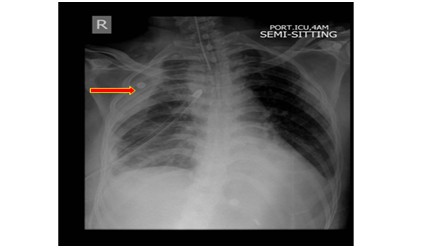
The amount of drained blood decreased with time till finally became minimal serous fluid, yet the patient still have extra pleural hematoma apparent on chest x-ray (figure 3).
Patient developed high grade fever (temperature higher than 38.5ᴼ C) that was investigated thoroughly but no clear cause was identified, and despite receiving empirical antibiotics and anti-tuberculosis medications (That was advised as therapeutic test for persistent and un resolving fever), patient remained febrile for more than one month till he went to a higher center and stayed there for several weeks where they stopped anti-tuberculosis drugs. Fever disappeared with time and, two months later, he returned to our hospital and he was afebrile without using antibiotics or tuberculosisdrugs, and chest x-ray showed resolution of the extra pleural hematoma.
CASE 2
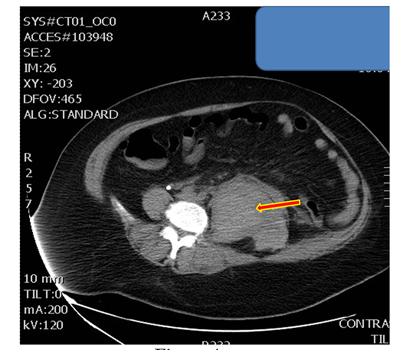
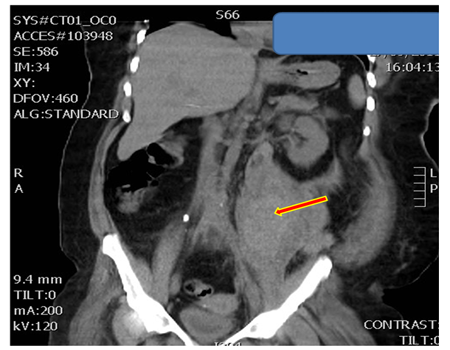
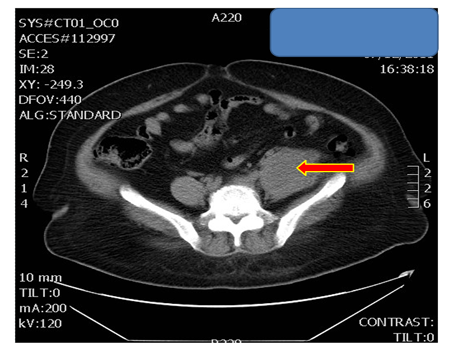
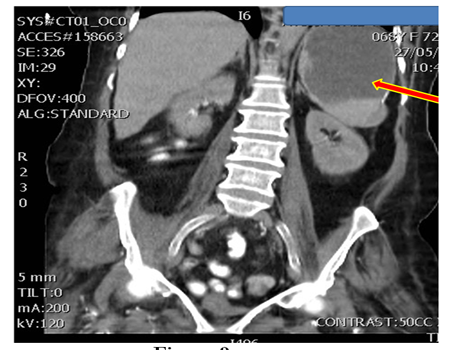
A forty eight years old Saudi woman on regular hemodialysis through right upper limb AVF, had suddenly, sneezed during dialysis then got severe lower abdominal pain. She was investigated thoroughly with no clear diagnosis. Few days later, she became highly febrile (temperature 39ᴼ C) with a drop at hemoglobin level of four grams over few days. CT abdomen was done and showed large Psoas muscle hematoma (figure 4-5). Patient remained febrile for one month until resolution of the hematoma (figure 6).
All septic screens were negative at that time and antibiotics were stopped for the patient.
3.CASE 3
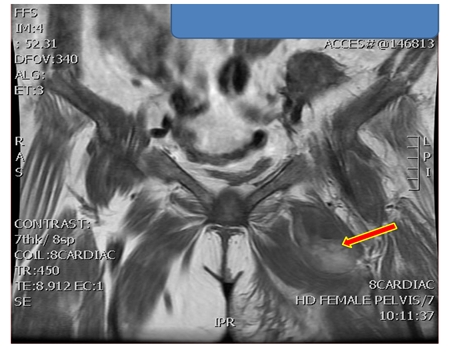
A Sixty eight years old Saudi female known case of ESRD and hepatitis C virus positive maintained on HD for six years, her dialysis access was right femoral permacath. She had severe Left thigh pain for few days with no history of trauma. She was examined by orthopedic surgeon, fracture neck of femur was suspected and MRI was done (figure 7).That showed a large hematoma. Also, her hemoglobin dropped from 10.9 gm/dl to 5.5 gm/dl over eight days. The Patient was admitted and received Packed Red Blood Cells (PRBCs) transfusion until hemoglobin level reached 11.2 gm/dl. She had fever for few days (temperature 38ᴼ C) and septic screen was negative with no reason for fever identified apart from the hematoma. No antibiotic was given and few days later, fever subsided and she was discharged home.
CASE 4
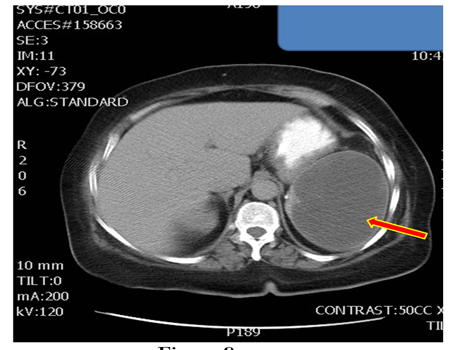
A Sixty Eight years old Saudi female known to have ESRD, DM and Hypertension, was admitted originally because of sepsis and received proper antibiotics, and follow up culture was negative. She was dialyzing through left AVF.
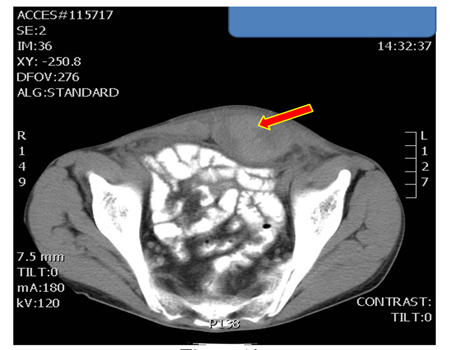
Few days later, she became highly febrile (temperature 39ᴼ C) with a drop of hemoglobin of 4 grams and as a lesson from the previous cases, CT abdomen and pelvis was done (figure 8-9) showing huge splenic hematoma.
Patient remained febrile for the whole period of stay in our hospital after the hematoma. She was transferred to a higher center for a second opinion and she stayed there for two weeks with no additional treatment given until she died there.
CASE 5
A twentyone years old Saudi male known to have ESRD (due to Alport’s syndrome) on regular HD through left AVF, hepatitis C positive and dilated cardiomyopathy, had persistent cough then he developed severe lower abdominal pain. On examination, he had severe tenderness over the lower abdomen with a palpable mass (tender and poorly localized). Again, his hemoglobin dropped from 10.5 gm/dl to 8.2 gm/dl over few days and he had mild fever (temperature 38ᴼ C).
CT abdomen and pelvis was requested and showed rectus muscle hematoma (figure 10).
The patient remained febrile for a few days then the fever disappeared completely without any antibiotic therapy.
Discussion
Fever, an elevation in core body temperature above the daily range for an individual, is a characteristic feature of most infections but is also found in a number of non-infectious diseases such as autoimmune diseases [1].
Compared with the population with normal kidney function, patients with chronic kidney disease (CKD) and end stage renal disease (ESRD) are at higher risk of acquiring bacterial infections, particularly urinary tract infections, pneumonia, and sepsis [2,3].
Bacterial infection is a major cause of mortality and morbidity in the hemodialysis (HD) population and vascular access is the main route for bacteraemia [4]. The immunological system is deficient in patients with uremia [5], which may impair their pyrogenic response to infection. As one study showed, 13of 21 asymptomatic controls were discovered to have purulent material in their clotted grafts [6].
As a result to the above mentioned data, the diagnosis of Gram positive bacteraemia should be suspected in the presence of fever >38°C, chills, hypotension, tachycardia and/or hyperventilation [5]. In this case series, we are drawing attention to another cause that is not well covered by contemporary literature dealing with dialysis population.
Two well recognized vascular causes of fever of unknown origin (FUO) are pulmonary emboli and hematomas in enclosed spaces [7]. The incidence of hematoma induced fever may be higher in hemodialysis patients than general population due to the use of anticoagulant during hemodialysis sessions together with frequent need for invasive vascular access insertion.
In agreement with Herman et al., hematoma as an isolated cause of temperature elevation in an adult patient is rarely reported [8]. Under recognition or misdiagnosis by physicians may contribute to unnecessary and prolonged use of antibiotics with the risk of emergence of resistant strains and the risk of their adverse effects on the patients, not to mention missing serious internal organs bleeding or hematoma.
Considering that this is the first paper trying to document hematoma as a possible cause of high grade fever in ESRD, further research is needed to document the prevalence and exact mechanism of such association.
We should consider hematoma of various organs if we faced unexplained high fever in End Stage Renal Disease patient. Empirical antibiotics - that werestarted till culture results are available- should be stopped once the possibility of infection is ruled out, especially if there is no clinical effect on the fever.
5.References
- Reuven Porat and Charles A Dinarello. Pathophysiology and treatment of fever in adults. Uptodate 21.2 (2013), Topic 2734 Version 8.0.
- Naqvi SB, Collins AJ. Infectious complications in chronic kidney disease. Adv Chronic Kidney Dis 2006; 13:199.
- Dalrymple LS, Katz R, Kestenbaum B, et al. The risk of infection-related hospitalization with decreased kidney function. Am J Kidney Dis 2012; 59:356.
- Kessler M, Hoen B, Mayeux D et al. Bacteremia in patients on chronic haemodialysis. Nephron 1993; 64: 95–100.
- Claudio Ponticelli. New recommendations in the treatment of Gram-positive bacteraemia in dialysis patients. Nephrol Dial Transplant 2008; 23: 27–32.
- David Sheikh-Hamad and J.CarlosAyus. The patient with a clotted PTEF graft developing fever. Nephrol. Dial. Transplant. 1998; 2392-2393
- J. V. Hirschmann. Fever of Unknown Origin in Adults. Clinical Infectious Diseases 1997; 24:291-302.
- Chmel H, Palmer JA, Eikman EA. Soft tissue hematoma as a cause of fever in the adult. DiagnMicrobiol Infect Dis. 1988 Dec; 11(4):215-9.