Information
Journal Policies
Effect of Maintenance Hemodialysis on Red Cell Indices and Erythrocyte Sedimentation Rate in Northeast Nigeria
Emmanuel Asuquo Etim
Copyright : © 2018 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Background: The process of maintenance hemodialysis which is an artificial kidney by principle can result in alteration in hematological parameters. This study aims to investigate the effects of maintenance hemodialysis on erythrocyte sedimentation rate and red cell indices.
Materials and methods: A total of 78ESRD subjects receiving hemodialysis, (comprising 35 men and 43 women), with mean age of 53 ± 21years participated in this study. There were 58% subjects above 50years old while 42% of subjects were below 50years. A total of Three milliliters of blood were collected from subjects before and immediately after hemodialysis session. Full Blood Count was determined in the blood using Sysmex XP 300 automated hematological analyzer while ESR was measured using the modified Westergren method.
Results: For subjects below 50years of age, the mean ESR value changes from 21.59 ± 0.41 mm/hr in pre hemodialysis blood to 70 ± 1.13mm/hr in post hemodialysis blood P< 0.05 while the mean ESR value of subjects above 50years old increases from 78 ± 2.19mm/hr in pre hemodialysis blood to 115 ± 1.83mm/hr in post hemodialysis blood. The value of red cell indices increases after hemodialysis session at P < 0.05. But, MCH, and RDW showed no significant difference in pre and post hemodialysis blood P< 0.05.
Conclusion: ESR Significantly increases in post hemodialysis blood than in pre hemodialysis blood. RDW and MCH value did not show statistical significant differences in pre and post hemodialysis blood.
Hemodialysis, Erythrocyte Sedimentation Rate, Red Cell Indices,Hematology
1. Introduction
Maintenance hemodialysis has been the most common method used to treat advanced and permanent kidney failure since in1960s. [1] Hemodialysis (HD) is one of the methods of renal replacement therapy [2] readily available in Nigeria.[3] HD is a type of dialysis technique in which substances move from the blood through a semi permeable membrane into an hemodialysis solution (hemodialysate) using concentration gradient principle. Some hemodialysate contains glucose concentration of 1.5%, 2.5% or 4.25% [4] and the electrolyte composition is usually similar to that of human plasma [5] and in some cases, Dialysate sodium bicarbonate concentration of 35–40 mmol/l are used to provide a gradient for bicarbonate to diffuse into the patient’s blood. [6]An average normal hemodialysis session usually last between 3– 4 hours. Ultimately, both the hemodialysis machine and hemodialysate can result in changes in the value of Erythrocyte Sedimentation Rate (ESR) and red cell indices. Hemodialysis by itself do contributes to decrease in RBC survival because of mechanical damage induced by the dialysis membrane and extracellular circulation. [7] In addition, hemodialysis also leads to changes in the erythrocyte cytoskeleton structure and the presence of glucose in dialysis fluid activates the pentose phosphate pathway which contributes to the intensification of oxidative stress in the blood[2] and also, thrombocytopenia do occur as a side effect of hemodialysis.[8] Dialyzer hyper sensitivity symptoms are infrequently associated with a fall in platelet count and it has been reported that most recent cases of dialysis associated thrombocytopenia is seen with polysulfone membrane sterilized by electron beam. [9]
Red cell indices are part of routine automated full blood count test which measures our general health. Red cell indices examine red cell conditions and measures the size, shape, and physical characteristics of red blood cell. Red cell indices consider in this study are: RDW (Red Cell Distribution Width), MCV (Mean Cell Volume), MCH (Mean Cell Hemoglobin), MCHC (Mean Cell Hemoglobin Concentration).
Chronic hemodialysis patients have chronic anemia due to lack of adequate erythrocyte production as a result of impaired erythropoietin production occasion by prolong renal problem. Patients with ESRD are susceptible to metabolic and physiologic degradation due to the interplay between kidney function, biochemical and hematological disturbances that occur in kidney failure.[10] The protocols of maintenance hemodialysis (an artificial kidney for people whose kidney can no longer sustain life) can also cause changes in ESR.
ESR is the rate in millimeters per hour at which red cell forms rouleaux and settles through the plasma in a vertical column. ESR is a common hematological test which is a non-specific measure of inflammation.[11] Various factors usually affects ESR value, such as the size and shape of red cell, plasma volume, fibrinogen, and globulin levels as well as mechanical and technical factors of hemodialysis. The red cells normally have a net negative charge and repel each other, but many plasma proteins are positively charge and neutralize the surface negative charge of erythrocytes thereby reducing the repulsive forces that exist between red cells hence promoting aggregation (rouleaux formation) [12] which in turn increases rate of red cell sedimentation and it turn out that, the higher the plasma protein concentration, the higher will be the rate of sedimentation. Alteration in the sedimentation rate of red cell has been also attributed to both plasma and red cell factors[13].
Reports in medical literature indicates that patients with extremely elevated ESR (>100mm/hr) had renal diseases of varying etiologies [14] but only few studies have addressed changes in ESR in patients with ESRD on maintenance hemodialysis.[15] In Nigeria however, the effects of hemodialysis on ESR and red cell indices have not yet been fully examined. This study therefore aims to investigate the effects of maintenance hemodialysis on erythrocyte sedimentation rate and red cell indices in other to elucidate the pathophysiology of hematological changes in patients on routine maintenance hemodialysis.
2. Materials And Methods
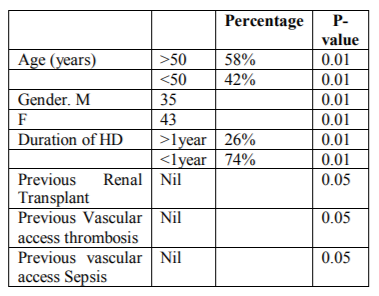
This prospective study was carried out at the Federal Medical Center of Yola, in Adamawa State, Northeast Nigeria. A total of 78 ESRD subjects receiving hemodialysis took part in the study, comprising 35 men and 43 women, with an average age of 53 ± 21years. There were 58% of subjects above 50years of age while 42% of subjects were below 50years and 26% of the subjects have had dialysis for more than one year while 74% have been on maintenance hemodialysis for less than a year. None of the subjects either had previous renal transplant, previous vascular access thrombosis, or previous vascular access sepsis (table 1).
Three milliliters of blood were aseptically collected from all subjects before and immediately after hemodialysis session. The blood was put in EDTA vacutainers that were further labeled with the patient number, sex, and age. Full blood count was determined in the pre and post hemodialysis blood sample within one hour of collection using Sysmex XP 300 automated hematological analyzer and ESR was measured in the pre and post hemodialysis blood using modified westergren method. All tests were carried out according to the standard operating procedure. The hemolysate (acid and sodium bicarbonate) used was automatically prepared by the hemodialysis machine (dialog+B/Braun).
Patients with chronic kidney disease stage 5 (i.e. ESRD) receiving routine maintenance hemodialysis were included. ESRD patients that were not receiving routine maintenance hemodialysis and those above 83years old were excluded from this study.
3. Sample Analysis
Using the sysmex XP300 hematology analyzer, the procedure for full blood count determination was performed as follows: EDTA samples were placed in a blood mixer for five minutes and the blood cells were automatically counted through a probe fitted in the sysmex machine. After one minute, the result of the blood cell count was displayed on the colored LCD screen of the machine.
Blood was transferred to a standard westergren tube and drawn to 200mm mark in capped pipette containing 0.5ml of 3.8%trisodium citrate. The tube was placed in a rack in strictly vertical position and allowed to stand for 1 hour at room temperature of 270c. The distance from the lowest points of the surface meniscus of stacked red cell to the upper limit of the plasma was measured after one hour and the reading taken as the ESR value was expressed in millimeters per hour.
4. Statistical Analysis
Statistical analysis was performed using the SPSS (Statistical Package for Social Science) 20.0 software (Chicago IL). Descriptive value was given as mean standard error of mean. Categorical variation was expressed as the number of cases and the percentage value. The student’s t-test was used to compare the mean difference between pre and post hemodialysis blood.
5. Results
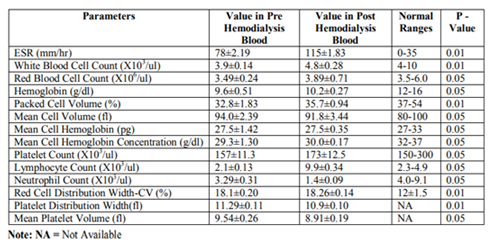
ESR and most red cell indices values was increased in post hemodialysis blood of all the age group when compared to the value in pre hemodialysis blood and the normal range at P< 0.05 as shown in table 2. However, the mean value of mean cell hemoglobin (MCV), mean platelet volume (MPV) and neutrophil count were low in post hemodialysis blood compare to the values in pre hemodialysis blood of subjects above age of 50years (table 2).
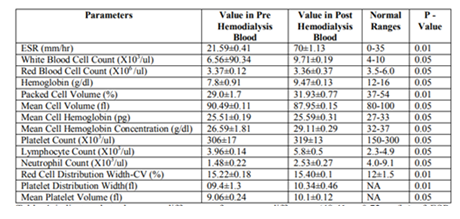
The ESR value in pre hemodialysis blood was higher than the reference value for subjects above 50years of age when compared to that of subjects below 50years of age. Table 3 indicated that the value of ESR in the post dialysis blood was higher than that of the pre dialysis blood of the subjects above 50 years of age at P< 0.05. For the subjects above 50years of age it was observed that, Packed Cell volume (PCV) increases from 32.8 ± 1.83% in the pre dialysis blood to 35.7 ± 0.94% in the post dialysis blood (table 2). While for the subjects above 50years of age the mean PCV value increases from 29.0 ± 1.7% to 31.93 ± 0.77%. Additionally, table 3 shows that the mean value of ESR of pre hemodialysis blood was 21.59 ± 0.41mm/hr (within the normal range) for subjects below age 50years while the post hemodialysis ESR was 70 ± 1,13mm/hr at P< 0.05, but the mean ESR value in the pre hemodialysis blood of subjects above 50 years of age was 78±2.19mm/hr (higher than the reference range) while the post hemodialysis ESR was 115±1.83mm/hr. In the blood of subjects above 50years of age also, there was no significant difference in the value of red cell count and mean cell hemoglobin in pre and post hemodialysis blood.
Although most of the red cell indices values increases after hemodialysis session as shown in table 2 and table 3, the MCH and RDW did not show significant differences in pre and post hemodialysis blood of subjects. In addition, while MCHC values increases in post hemodialysis blood, MCV value was observed to be reduced in post hemodialysis blood at P< 0.05 for subjects above 50years of age while the reverse was true for subjects below 50years old (table 2 and table 3). When comparing the mean platelet volume (MPV) of pre and post dialysis blood it was observed that, MPV was reduced in post hemodialysis blood compare to that of the pre hemodialysis blood of subjects above 50years (P< 0.05) while it was increased in the post hemodialysis blood of subjects below 50years of age. Age was a factor contributing to changes in the values of red cell indices and red cell sedimentation rate in pre and post hemodialysis blood (table 3).
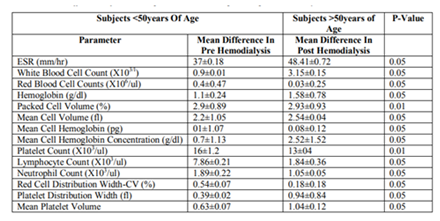
Table 4 indicates that, the mean difference of ESR value between pre and post hemodialysis blood (37±0.18mm/hr) for subjects below 50years old was significantly lower than the mean difference (48.41 ± 0.72mm/hr) of ESR value between pre and post hemodialysis blood for subjects above the age of 50years at P< 0.05.
6. Discussion
In this present study, it was observed that, Erythrocyte Sedimentation Rate (ESR) values in post hemodialysis blood was significantly higher than that of the pre hemodialysis blood of all subjects at p< 0.05. This may be due to increase rate of rouleaux formation in post hemodialysis blood because sedimentation of red cells is greatly influenced by the extent to which the red cells forms rouleaux and the faster the formation of rouleaux, the higher will be the rate of erythrocyte sedimentation and rouleaux formation is in turn influenced by the concentration of plasma protein like fibrinogen, globulin and other acute phase proteins[16] whose concentration may increase in post hemodialysis blood as a result of changes in plasma volume due to hemodialysis mechanisms. Also, the higher ESR value observed in post hemodialysis blood is an indication of inflammatory process which may be triggered by hemodialysis procedures since inflammatory process do increase fibrinogen in peripheral blood [17] and high proportion of fibrinogen in the blood do make red blood cells to stick to each other causing red cells to settle faster and thereby increases the rate of it sedimentation. However, the impact of different factors affecting ESR in End Stage Renal Disease (ESRD) patients on hemodialysis has been conflicting in different studies. Nevertheless, elevated values of ESR in post hemodialysis blood compared to pre hemodialysis blood of all subjects observed in this study conforms with the report of Mohammed Ibrahim et al.,[15] but differs from the report of Bathon J et al.,[18]
Packed Cell Volume (PCV) of pre hemodialysis blood was lower than the normal range because hemodialysis patients have chronic anemia due to impaired erythropoietin production as a result of prolong renal problem.
Increase in red cell indices observed in this study in post hemodialysis blood compare to the value in pre hemodialysis blood is believed to be due to changes in plasma volume as a result of hemodialysis mechanism since most red cell indices value is related and/or dependent on plasma volume. [19,20] Although the value of most red cell indices increases in post hemodialysis blood compare to it value in pre hemodialysis blood but, the mean value of RDW and MCH remains unchanged in pre and post hemodialysis blood. This observation shows that hemodialysis with dialog+B/Braun machine using acid and sodium bicarbonate dialysate do not have significant effect on red cell structure since red cell distribution width (RDW) is a red cell index whose value reflects the degree of variation in red cell structure.
7. Conclusion
When comparing the mean value of red cell indices and ESR in pre and post hemodialysis blood, differences in mean values was observed. The change was more significant in erythrocyte sedimentation rate. The rate of sedimentation of red cell was significantly increased in post hemodialysis blood compare to the value in pre hemodialysis blood. Most red cell indices had higher value in post hemodialysis blood than in pre hemodialysis blood but, Red Cell Distribution Width (RDW) and Mean Cell Hemoglobin (MCH) values did not show significant difference in pre and post hemodialysis blood. Age was observed to be a factor contributing to changes in the measured parameterin pre and post hemodialysis blood. Information obtained in this study will improve the understanding of the pathophysiology of hematological changes in patients on maintenance hemodialysis in Northeastern Nigeria.
References
- Kultigin T, Faith M, Fatih O, Adalet O, Emin M, Aysu O. Platelet-to-lymphocyte ratio better predicts inflammation than neutrophil-to-lymphocyte ratio in end-stage renal disease patients.J hemodialysis Intl;2013;17(3)391-396.
- Maria Olszewsk, Joanna Bober, Jerzy Wiatrow, Joanna Stepniewsk, Barbara Dolegowk, DariuszChlubek. The impact of hemodialysis on erythrocyte membrane cytoskeleton proteins. PostepyHig Med Dosw (0nline), 2015; 69:165-175.
- Okaka EI, Unuigbe EI. Eight-year review of hemodialysis: Treated patients in a tertiary center in Southern Nigeria. Ann Afr Med 2014; 13:221-225.
- Omer Mehina. Effect of hemodialysis on blood glucose level. Intl J Anatomy and Research. Elixir Physio. & Anatomy. 2015(87):35771-35772.
- Yasir AH, Hakim AA, Abbas I, Adil Khalil, Hameeda Ibrahim, Ahmed Mustafa. The effect of hemdialysis on hemoglobin concentration, platelet count and white blood cells count in End Stage Renal Failure. Int J Med Res & Health Sc.2016; 5(5):22-35.
- Barry Kirschbaum. The effect of hemodialysis on electrolyte and acid-base parameters. ClinicaChimicaActa. 2003; 336:109-113.
- Frederiek E. Vos, John B. Schollum, Carolyn V. Coulter, Terrence C.A. Doyle, Stephen B. Duffull, Robert J. Walker. Red blood cell Survival in Long-term Dialysis patients. Am J Kidney Dis. 2011; 58(4):591-598.
- Katz I. Kidney and kidney related chronic disease in South Africa and chronic disease intervention program experiences. Adv Chronic Kidney Dis.2005; 12:14-21.
- John T. Daugirdas, Angelito A. Bernardo. Hemodialysis effect on platelet count and function and hemodialysis-associated thrombopenia. Kidney Intl.2012; 82:147-157.
- Degrassi F, Quaia E, Martingano P, Carvallaro M, and Cova MA. Imaging of hemodialysis renal and extrarenal findings. Insights Imaging.2015; 6(3):309-321.
- Zacharski LR, Kyle RA. Significance of extreme elevation of erythrocyte sedimentation. JAMA. 1967; 220:264-266.
- Rovel A, H’Huillier JF, Vigneron C. Mechanism of erythrocyte sedimentation. Biomedicine J.1978; 28:248-255.
- Shusterman N, Kimmel PL, Kiechle FL. Factor’s influencing erythrocyte sedimentation in patients with chronic renal failure. Arch Intl Med. 1985; 145:1796-1799.
- Wyler DJ. Diagnostic implication of markedly elevated erythrocyte sedimentation rate: A revaluation. South Med J. 1977; 70:1428-1430.
- Mohammed IbraheemAlsomalli, Muhammad Yousuf, Fayez Hejailli, waleedAlmotain, Abdulla A. Al-sayyari. Erythrocyte sedimentation rate in stable patients on chronic hemodialysis. Saudi J Kidney Dis transpl.2015; 26(6):1149-1153.
- Al-Homrany M. The significant of extreme elevation of the erythrocyte sedimentation rate in hemodialysis pateints. Saudi J Kidney Dis Transpl.2002; 13:141-145.
- Emelike OF, Akpan JE, Obigwe BU, Jeremiah ZA. Comparative study of erythrocyte sedimentation rate (ESR) using Trisodium Citrate, Normal Saline and Whole Blood in Ethylene Diamine Tetra Acetic Acid (EDTA). J ApplSc Environ Manage.2010; 14(1)23-27.
- Bathon J, Graves J, Jens P, Hamrick R, Mayes M. The erythrocyte sedimentation rate ion end-stage renal failure. Am J Kidney Dis.1987; 10:34-40.
- Mohammad H. Sadeghian, Hossein Ayatollahi, Hossein Azarian, MaliheNajibzade, HamideFarzam, EnsiehKhajehim. Correlation between Hyperlipemia and erythrocyte indexes. Intl J Hematol and Oncol.2008; 3(18):150-152.
- Bisallah Chindo Ibrahim, Muhammad AbubakarAmali, Umar Isah A, Soje Michael O, ABubakar Mohammad Ramadan. Demographic characteristics and causes of chronic kidney disease in patients receiving hemodialysis at IBB specialist hospital Minna, Niger State, Nigeria. J med and Medical res.2015; 3(4):21-26.