Information
Journal Policies
Invasive Mole Complicating a Spontaneous Abortion
Hary Fanambinantsoa Rabarikoto1*, Nomeharisoa Rodrigue Emile Hasiniatsy2, Herilalao Elisabeth Razafindrafara3, Domoina Malala Aurelia Randriambololona4
2.Department of Oncology, Soavinandriana Hospital Center Antananarivo, Madagascar.
3.Department of Pathology, Soavinandriana Hospital Center Antananarivo, Madagascar.
4.Department of Obstetrics and Gynecology, University hospital center Tanambao I Antsiranana, Madagascar.
Copyright : © 2018 . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Invasive mole is a rare gestational trophoblastic neoplasia occurring exceptionally after a miscarriage. It is a chemosensitive and curable disease. We aimed to report a case of invasive mole occurring after a spontaneous abortion. A 32-year-old patient, multiparous, presented persistant vaginal bleeding 12 weeks after expulsion. The pregnancy test was positive, the ultrasound didn’t find any abnormalities and the biopsy of the endometrium was not contributive. The patient returned two months after with a cardiovascular collapse and presented an acute abdominal pain with haemoperitoneum at the ultrasonography. A laparotomy was performed in emergency which discovered an important bleeding from the fundus of the uterus which has been perforated, leading up to realize an emergency hemostasis hysterectomy. The histological examination of the operative specimen found an invasive mole. The patient was put on methotrexate. A favorable evolution was observed.
Abbreviations: GTN: gestational trophoblastic neoplasia, HCG: choriogonadotrophin, MTX: methotrexate.
Chemotherapy, invasive mole, miscarriage, surgery, uterine perforation,Gynecology, Obstetrics
1. Introduction
Invasive mole is a rare gestational trophoblastic neoplasia (GTN) characterized by the penetration of molar tissue into the uterine myometrium or into the uterine vascularization [1]. In rare cases, these villi cross the entire uterine wall resulting in acute haemoperitoneum [2]. It usually follows a molar pregnancy but can occur after any pregnancy whatever its outcome [2,3]. We aimed to report a case of invasive mole developing after spontaneous abortion, and revealed by a haemoperitoneum with uterine perforation.
2. Observation
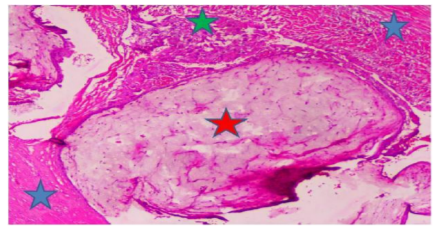
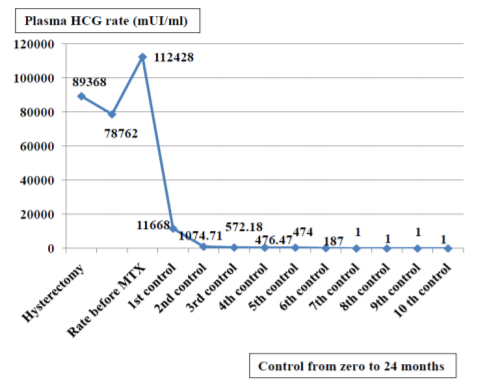
This is a 32-year-old patient, G6P4A2, who was seen in consultation for persisting vaginal bleeding three months after spontaneous miscarriage. The last abortion occurred at seven weeks of gestation, the expulsion happened at home, without any intrauterine proceeding. She didn’t take any contraception. During the examination, the abdomen was not painful, the bleeding came from the endocervix. The urinary choriogonadotrophin (HCG) was positive, the ultrasound has found an empty uterus without particular intrauterine image, nor image of suspicious latero-uterine mass. The dosage of plasma HCG was prescribed but not honored by the patient. A biopsy of the endometrium with the pipelle of Cornier was not contributive, finding no trophoblastic material or sign of malignancy. The patient was long lost after. Two months after this period, she returned for acute abdominal pain associated with heavy vaginal bleeding. Clinical examination found a cardiovascular collapse with peritoneal flowing at the ultrasonography. A laparotomy in emergency was realized, revealing an important bleeding from the fundus of the uterus. It was irregular, presenting a perforated lesion with 2.5 cm of diameter which had an appearance of placenta percreta, but without fetus, thus leading up to suspect a gestational trophoblastic neoplasia. An hemostasis hysterectomy was decided in emergency. The plasma rate of HCG the day of the intervention was 89 368 mIU / ml and it dropped more than 10% the next day (78762mUI / ml). The histological examination of the operative specimen found an invasive mole within a gestational trophoblastic neoplasia, confirmed by a review of a referral team (Figure 1).
The HCG was up to 112 428 mIU / ml after 15 days. The extension assessment was negative. The prognostic classification of the International Federation of Gynecology and Obstetrics was less than 6, the patient was treated by methotrexate (MTX). The decrease of the level of plasma HCG was rapid under chemotherapy and its negativation was obtained after two months (Figure 2). At 24 months of follow-up, the patient was completely asymptomatic.
3. Discussion
The invasive mole is a histological subgroup of GTN. There are three other types, including choriocarcinoma, placenta-site trophoblastic tumor and epithelioid trophoblastic tumor [3,4]. Its prevalence is not much known, but all GTN constitute less than 1% of all gynecological tumors [5]. It usually follows a molar pregnancy [1] but can occur after any pregnancy whatever its outcome [2,3]. An histological examination of all abortions’ products is advised to avoid a delay of the diagnosis. In our case, the invasive mole happened after a spontaneous abortion which seemed following a normal pregnancy. These complications have to be sought in case of persistence of vaginal bleeding after a miscarriage. Indeed, any persistent unexplained bleeding at more than six weeks after a pregnancy should have a GTN searched [3]. Pelvic ultrasound and HCG dosage serum total allow to have the diagnosis [3,6] However, the definitive diagnosis of invasive mole is made on histology [7].
For our patient, the diagnosis of invasive mole was made late, only after the histological examination of the operative specimen.
Concerning the treatment, hysterectomy is indicated to control complications and stabilize patients in cases of abdominal urgency by uterine bleeding, severe bleeding, sepsis, and the patient who had completed her parental project [2,8-10]. In Madagascar, in the first case described by Rajaonera in 1965, it was the main treatment of the invasive mole [11]. It does not prevent yet the occurrence of metastases [2].
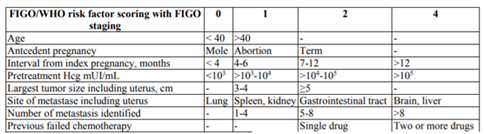
Currently, chemotherapy is the main treatment of invasive mole and is effective in almost 100% of cases [12,13]. It will be based on the category of prognosis classification of the International Federation of Gynecologists and Obstetricians (FIGO) both the World Health Organization (Table 1) [6].
The score value for the risk factor are 1, 2 and 4 and score of 6 or less is classified “low-risk disease” [3,6]. Patient at a low-risk like the case we report could put on monochemotherapy with MTX [13,14].
The monitoring of plasma HCG allows to evaluate the efficiency of chemotherapy of an invasive mole [3]. In our practice, plasmatic HCG is dosed before chemotherapy to have a starting point. Then it is monitored weekly until two weeks after negativation, monthly during three months and quarterly until 24 months after diagnosis. The chemotherapy is effective if the plasma HCG level is negative.
4. Conclusion
Invasive mole is a rare gestational trophoblastic neoplasia that can be life-threatening. Any persistent vaginal bleeding after any pregnancy should lead up to suspect it. Early diagnosis allows the initiation of chemotherapy which permit to avoid complications and to preserve the obstetric prognosis. Hysterectomy can be considered when the vital prognosis is threatened.
References
- Tse KY, Chan KK, Tam KF, Ngan HY, An update on gestational trophoblastic disease, Obstet Gynaecol Reprod Med. 22(1), 7-15 (2012).
- Aminimoghaddam S, Maghsoudnia A, Unusual Presentation of Invasive Mole: A Case Report, J Reprod Infertil. 18(1), 205-209 (2017).
- Institut National du Cancer – Haute Autorité de Santé, Recommandations de bonne pratique, Maladies trophoblastiques gestationnelles (môles hydatiformes et tumeurs tropho blastiques gestationnelles) : diagnostic et prise en charge. (2010). http://www.e-cancer.fr/content/download/58368/532120/file/10-06-11 MTG_Recommandations_LabelINCa-HAS.Pdf (accessed in 28th December, 2017).
- Lurain JR , Gestational trophoblastic disease: epidemiology, pathology, clinical presentation and diagnosis of gestational trophoblastic disease, and management of hydatiform mole, Am J Obstet Gynecol. 203(6), 531-9 (2010).
- Nair K, Al-Khawari H, Invasive mole of the uterus- a rare case diagnosed by ultrasound: a case report, Med Ultrason.16(2), 175-8 (2014).
- Ngan HY, Kohorn EI, Cole LA, Kurman RJ, Kim SJ, Lurain JR et al, Trophoblastic disease, Int J Gynaecol Obstet. 119 (2), S130-6 (2012).
- Wells M, The pathology of gestational trophoblastic disease: recent advances, Pathology. 39(1), 88- 96 (2007).
- Sahaja Kittur, Venktesh, Ramlingappa A, A rare case of invasive mole with silent uterine perforation, Int J Reprod Contracept Obstet Gynecol. 2(1), 109-110 (2013).
- Fang J, Wang S, Han X, An R, Wang W, Xue Y, Role of adjuvant hysterectomy in management of high-risk gestational trophoblastic neoplasia, Int J Gynecol Cancer. 22(3), 509–14 (2012).
- Doll KM, Soper JT, The role of surgery in the management of gestational trophoblastic neoplasia, Obstet Gynecol Surv. 68(7), 533-42 (2013).
- Rajaonera R, Franco R, Le problème de la dégénérescence post-molaire : à propos d’un diagnostic de chorioadenoma destruens, Ann de l’Univ de Mad (Medicine). 3(2), 25-8 (1965).
- Seckl M J, Sebire N J, Berkowitz R S, Gestational trophoblastic disease, Lancet. 376, 717–29 (2010).
- Niemann I, Vejerslev LO, Frøding L, Blaakær J, Maroun LL, Hansen ES, and al, Gestational trophoblastic diseases - clinical guidelines for diagnosis, treatment, follow-up, and counselling, Dan Med J. 62(11), (2015).
- Froeling F E, Seckl M J, Gestational trophoblastic tumours, Curr Oncol Rep.16, 408 (2014)