Information
Journal Policies
Taxpayer Burden Related to Family Planning and Birth Control. An Analytic Review
Kurt Kraetschmer MD, PhD*
Copyright : © 2018 . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Background: Various aspects of contraception and family planning continue to be topics of scholarly articles and public health media. Hitherto, the information provided in these publications has never been the object of a critical analysis. Such an analysis reveals implications in the area of socio-economics, including burdens for the taxpayer.
Aim: The paper aims at rectifying error-prone information disseminated by various agencies and organisations and stipulates that accurate information can lead to increased use of contraceptive measures and thus engender economic advantages for the health care system including the individual taxpayer.
Conclusion and Implications: The conclusion drawn from the analysis performed is evidence of inaccurate and incomplete information presently available for women in the U.S., especially for those planning to engage in family planning by means of contraception. The ensuing implications suggest rectification of flaw-ridden data. Such rectification will lead to improved possibilities of self-decision for women embarking on family planning and contribute to alleviating taxpayer burden regarding contributions to the health care system.
family planning, contraception, socio-economics, public health, government agencies,
Gynecology, Obstetrics
1. Material
The material used comprises scholarly articles published in journals with the highest impact factors and information in the form of websites or reports provided by the most frequently consulted government agencies. This material has been selected based on the scholarly impact of authors and on the authority and reputation of the institution or government agency in question. Only authors with highest impact factors and agencies or institutions with highest authority have been included in the review.
2. Method
Data were retrieved from scholarly journals and books as well as information disseminated via internet. The collection of data was guided by principles of evidence-based medicine which ascertain that only verifiable sources were taken in to account. These data were systematically organized according to their place of origin, namely government agencies, research institutes, and academic institutions. This method of organizing material collected was determined by the global impact of information selected, ie, the recognition by international scholarship.
3. Results
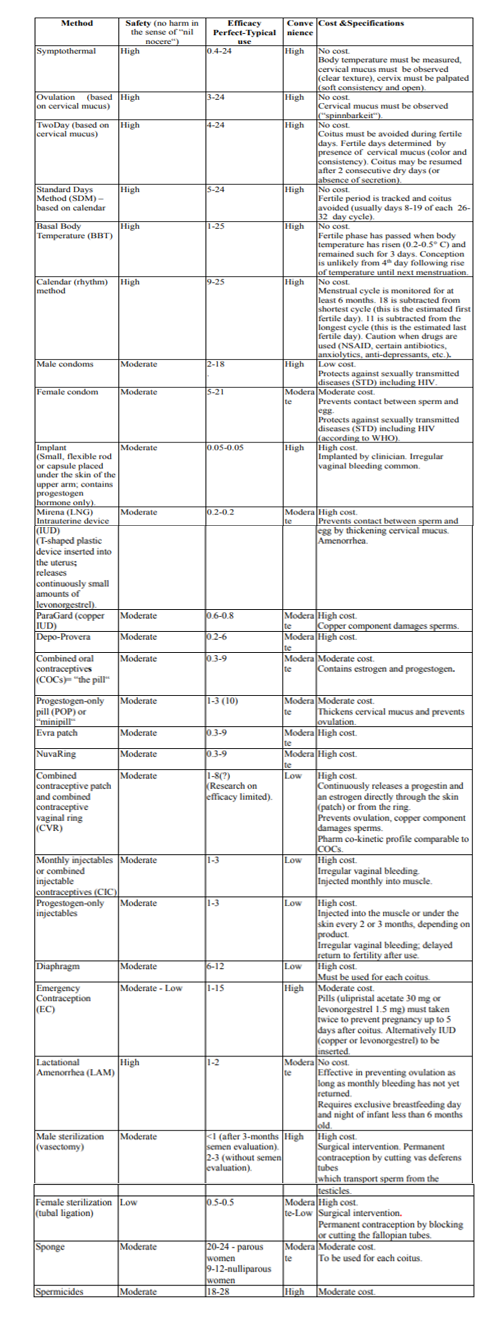
The results of data retrieval are summarized in a table based on the information emanating from the most influential scholarly publications as well as from the most authoritative agencies and organisations, namely Contraceptive Technology (2011), World Health Organisation (2018), Food and Drug Administration (2013), and American Congress of Obstetricians and Gynecologists (2017). Table 1 displays the rectified data in a synoptic fashion by focusing on the most salient parameters of contraception, namely safety, efficacy, convenience, and cost.
In contrast to other tables hitherto presented in the literature, this table ranks methods not primarily according to efficacy but according to safety, ie, absence of harm in the sense of the principle “nil nocere.” This method of ranking is based on the clinical experience that a great number of women places highest priority on safety and considers efficacy as secondary. Equally in contrast to other tables is the inclusion of the parameter convenience, which takes into account women's interest in easy practicability. Finally, fitting for the topic of this investigation, the factor cost is also considered.
4. Discussion
World-wide contraception continues to be a topical issue both in medical sciences and public health. Medical scholarship has been investigating for many years the salient features[1] and specificities of contraceptive methods;[2] in public health, topics such as teenage pregnancy related to provision of no-cost, long-acting contraceptive devices,[3] teen sexual health, [4] and contraception as a primary care service have been discussed[5,6].
The fundamental concerns in numerous investigations are socio-economic considerations, including the burden for the taxpayer. Thus, studies in the area of family planning led to the conclusion that in the U.S. “every $1 spent on public funding for family planning saves taxpayers $3.74 in pregnancy-related costs.”[7] Given the pivotal role of taxpayer money, it is regrettable that in the U.S.
communication between consumer and government agencies regarding contraception is being hampered by fundamental flaw, namely inaccurate, incomplete, and misleading information. In fact, the amount of taxpayer money saved with respect to family planning could be more substantial if such information were accurate, complete, unprejudiced, and thus conducive to averting pregnancy-related costs.
Given that about 62% of women of reproductive age are currently using contraception,[8] it can be estimated that this percentage would be considerably higher if women were informed more accurately about contraceptive methods including those that are not invasive, have no side effects or interactions with other medications, and bear none of the risks associated with so-called “standard” methods[9]. If such information were provided, women with intolerance to pills and devices and women devoted to a natural non-hormonal life-style would be prepared also to engage in contraceptive pursuits and thus contribute to the reduction of pregnancy-related costs.
So far, studies on health care have not sufficiently investigated the possibilities of motivating women to engage in family planning through improved education, including appropriate information on contraception. In an attempt to fill this gap of knowledge this investigation examines how presently available information could be altered to promote self-decision according to the principle of informed consent. Although it is based on the most influential agencies and most authoritative experts it is limited by a lack of verifiability. In many instances the investigation must rely on data presented in the literature without having the possibility of verifying these data.
From an international perspective it appears that in the U.S. accurate and comprehensive information on family planning is not communicated to the consumer as efficiently as in other societies. This deficit becomes patent in an analysis of the most frequently consulted sources of information, ie, publications emanating from government agencies, public health organisations, and research institutes. The following analysis examines information disseminated through these channels and draws attention to inaccuracies that stand in contrast to findings by international scholarship.
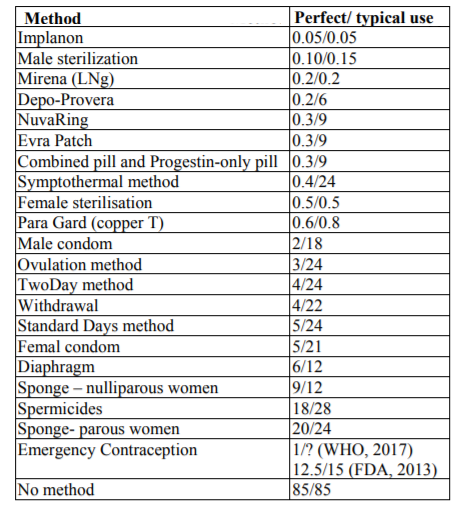
The U.S. Department of Health and Human Services (Office on Women's Health)[10] allegedly adapted WHO data to provide information on family planning and attributed collectively 24% (“number out of every 100 women who experienced an unintended pregnancy within the first year of typical use”) to the so-called “fertility-awareness based methods. “These methods are described as the least effective, barely superior to the “spermicide method” (28%). Such an assessment, alas, does not take into account that the nomenclature “fertility-awareness” comprises at least four different methods. Each one of these methods has a failure rate of its own, ranging from 0.4 perfect use (symptothermal) to 5 (Standard Days, based on the calendar), as can be seen from the most reliable estimates, namely those propounded by Contraceptive Technology[11]. These estimates are summarized in a table which provides ratings only, but can be adapted to a ranking according to perfect use estimates. In such an adaptation, the efficacy of each method can be identified conveniently and expeditiously, as can be seen from Table 2. (Cf. Table 2 Ranking based on Contraceptive Technology CT Failure Table, 2011).
The precision of the CT Failure Table, especially the distinction between perfect and typical use stands in sharp contrast to other ratings, as for example the website which emanates from the Office of Population Affairs (OPA)[12]. Here again, a common failure rate of 25% is indicated for the four methods, as if all of them were equally effective. What is correct, at least, is the characterization of the “sympto-thermal”/sic!/ method as a combination of basal body temperature and cervical mucus method. What is not mentioned by the OPA is the importance of observing several symptoms, such as mastalgia, irritation, and fleeting lower abdominal pain (“mittelschmerz”)[13]. However, on a positive note, the OPA underscores the importance of fertility awareness for achieving pregnancy. In fact, some of the fundamental therapeutic options implemented for the treatment of infertility are based on the principles of the “Billings' ovulation method,”ie, meticulous observation of changes in cervical mucus around the time of ovulation.
The lack of precision and completeness evidenced in information disseminated by U.S. government agencies stands in contrast to European public health communication media. These media provide precise and comprehensive information in both, scholarly reports and freely available popularizing print media[14]. Some widely distributed free magazines and pamphlets contain data on all available contraceptive methods, including those which in the U.S. are either neglected or misrepresented, ie, calendar, temperature, cervical mucus, and symptothermal. In addition, attention is drawn to various parameters, such as age and social status, to optimize the decision-making process of each individual woman. The accuracy of information communicated to the public is obviously a result of long-standing scientific research on contraception which stringently distinguishes the various methods from one another. As a result of focusing on individual methods[15], comprehensive information and reliable data have been circulated in Europe since the second half of the last century. Moreover, research has furnished data also on natural family planning or periodic abstinence methods[16], which in numerous U.S. publications are not even mentioned. The shortcomings of this research, alas, are lack of verifiability of the Pearl Indices utilized for rankings of contraceptive methods. This lack has been compensated partially by Contraceptive Technology,[11] and this compensation has been incorporated into the above mentioned Safety – Efficacy – Convenience – Cost Ranking (SECCR).
An in-depth analysis of publications emanating from the most influential U.S. agencies and organisations irritates the international scholar for reasons of incompleteness and unreliability. Thus, the U.S. Food and Drug Administration provides a consumer-friendly survey of FDA-approved contraceptive methods but makes no mention of such methods as calendar, cervical mucus, temperature or symptothermal[17]. It is true, the FDA's domain is food and drugs; but a survey of contraceptive methods that aims at completeness has to list all internationally recognized methods, even if they are not approved by the FDA. The arbitrary omission of certain methods leads the consumer into believing that such methods do not exist and represents a violation of the bio-ethical principle of “informed consent.”[18] This principle requires comprehensive and complete information so as to enable the patient to make an intelligent choice. Unlike European consumers who are in a position to consent to a specific method after having been adequately informed about the entire range of options, U.S. consumers lack vital information and are left with the impression that there are no other methods available than those approved and listed by the FDA. The weakness of the FDA survey is further exacerbated by paradoxical estimates for Emergency Contraception, where perfect use estimates (85%) are inferior to typical use estimates (87.5%). In view of such manifestations of inaptitude the taxpayer rightly asks why her/his money is invested in the production and dissemination of flawed and error-prone surveys, which are more suited to mislead the consumer than to enlighten her.
Similarly inaccurate is the information provided by other government-funded agencies. In a “Womens health” publication,[19] natural family planning is erroneously identified as the “rhythm method“ and attributed a failure rate of 25. This identification obscures the fact that “natural family planning” is not a method per se but just a taxonomic nomenclature. Moreover, the figure quoted might be correct for typical use estimates but not for perfect use, especially not for the symptothermal method, whose estimate for perfect use is 0.4, as can be seen from the above mentioned Safety – Efficacy – Convenience – Cost Ranking (SECCR) as well as from research by Contraceptive Technology[11].
What must be kept in mind in reviewing the inaccuracies and incompleteness of information emanating from U.S. government agencies is the economic aspect. This aspect includes not only the amount of money spent to produce and disseminate flawed or misleading information, but also the consequences of such misinformation in the area of public health. Millions of women remain ignorant of the possibilities of using low-cost or even no-cost methods of birth control and feel obliged to engage in rather costly procedures such as implants or intrauterine devices.
Moreover, from the viewpoint of socio-economics it is not only the cost for the production and dissemination of error-prone information that must be calculated but also the costs incurred for salaries and wages. After all, it is incompetent work force that has been involved and still is involved in the gathering, production and dissemination of flaw instead of providing the consumer with reliable and trustworthy information. Elimination of unqualified members of the work force from the pay-roll of government agencies would be tantamount to saving also considerable amounts of taxpayer money.
Improving the qualifications of government employed work force could contribute to reversing the trend towards unreliability and inaccuracy, which has been dominating the U.S. public health media during the last decade concerning questions related to family planning and contraception. Such efforts are presently a concern of one of the most authoritative organisations, ie, the American Congress of Obstetricians and Gynecologists (ACOG). While these experts on gynecological issues claimed in the past -- until recently as 2015 -- that natural family planning “is not as effective as other methods of birth control,”[20] they are presently acknowledging the advantages of fertility awareness methods. Particularly with respect to efficacy, cost, and absence of adverse events the virtues of these methods are recognized: “They cost very little. Many women like the fact that fertility awareness is a form of birth control that does not involve the use of medications or devices"[21].
In a similar fashion, the Centers for Disease Control (CDC) acknowledge the feasibility of fertility awareness methods for contraceptive pursuits. Although these centers cite the same inaccurate data as the agencies discussed above, namely 24, they draw attention to the advantages of the “newest” methods of fertility awareness by specifying: “Newest methods (Standard Days Method and Two Day Method) may be the easiest to use and consequently more effective.[22]”
The efforts towards rectification of flawed data, as exemplified by the ACOG, are rarely noticeable in publications emanating from institutions of higher education. In a publication with the heading “temporary contraception options” provided by “UWHeatlh,”[23] only the ovulation, the symptothermal, and the rhythm method are mentioned. In describing their characteristics, the symptothermal method is apparently erroneously identified as the temperature method and assigned the same estimate as the ovulation method (“90-95 percent effectiveness rate”). In addition, it is discredited as involving “a lot of details,” without taking into account that the symptothermal method involves nowadays only few details, especially in conjunction with easily available smart phone applications. Originally, it is true, a “cycle sheet” had been developed where body temperature and changes in cervical mucus had to be recorded, including position, opening and consistency of the cervix. Regarding the cumbersome task of closely observing symptoms it should not be overlooked that for some women attention to physiological processes is a welcome opportunity to get better acquainted with their own body. In addition, painstaking observation of these processes is nowadays a stringent requirement for the efficacy of infertility treatments.
Although some publications furnished by institutions of higher education provide correct descriptions of the symptothermal method, they fail to indicate conclusive failure rates[24] or add unverified comments recommending fertility awareness methods only for those “whose strong religious beliefs prohibit standard contraceptive methods.”[25] It is certainly true that in some societies a religious motive might encourage women to use one of the natural methods. Yet, in many instances the driving force is intolerance to hormones, aversion to pills and invasive procedures, as well as fear of complications.
What is perplexing for the international scholar is the fact that even U.S. scholarly publications do attempt to improve the quality of information disseminated. The widely-known National Health Statistics Report8 speaks in an unspecific manner of “fertility awareness” and indicates the probability of pregnancy as 25.3 (“probability of a contraceptive failure within the first 12 months of typical use of a contraceptive method”). As this report provides no specification of the methods belonging to fertility awareness, this figure leads to the assumption that all the methods that can be considered as fertility awareness have the same probability of a contraceptive failure. Such an assumption denies the statistically significant difference in efficacy among the methods of fertility awareness. It also contradicts widely acknowledged authorities in the statistics of failure rates, who attribute 0.4 to the most efficient of the fertility awareness, ie, natural family planning methods[26].
Idiosyncratic failure rates appear also in one of the leading medical reference-books, the MSD Manual[27]. Although this manual with a long history explains correctly that the symptothermal method is the most reliable among the “periodic abstinence methods” in determining the days where abstinence is mandatory, it attributes to this method a failure rate of 10%. This failure rate does not reflect the efficacy in case of perfect use, considered to be between 0.3 and 5.0 by international research[28].
Unorthodox figures for failure rates without attention to the specificity of each individual method are presented also in publications by specialists in reproductive health. In studies emanating from a widely-known international institute, fertility awareness-based methods are not distinguished from one another but indiscriminately assigned a failure rate of 0.4 -5 for perfect use and 24 for typical use[29]. It seems unlikely that the calendar method can reach a failure rate as desirable as 0.4; on the other hand, the symptothermal method with a perfect use failure rate of 0.4 must be implemented with utmost carelessness to worsen to a typical use failure rate as unfavorable as 24.
Another unresolved issue that plagues publications on reproductive health is the interpretation of data collected. In one of the most recent studies on contraceptive failure rates in the developing world the “calendar-rhythm” method is listed as a “traditional” method and attributed the highest failure rate, together with withdrawal[30].It seems obvious that in regions where illiteracy goes rampant and calendars (or cycle beads) are a luxury, the proper use of the calendar or basal body temperature method is a greater challenge for women than coitus interruptus or lactational amenorrhea. Above all, there is no proof in this and in numerous other studies that women using the “calendar-rhythm” method received adequate instruction to be capable of observing all the details which are a precondition for the successful use of the method. The same holds true for an objective assessment of the other periodic abstinence methods requiring observation of cervical mucus and rise of temperature, as described in the above mentioned Safety – Efficacy – Convenience – Cost Ranking (SECCR). Without an intensified communication between care provider and patient these methods are a priori doomed to failure. Past research has rarely addressed this precondition for the periodic abstinence methods and attributed a low efficacy without assessing the competence of the women using it. A sound competence, however, is a prerequisite for successful utilization of the method. In evaluating the efficacy of these methods it has been neglected in past investigations that they require a great deal more in-depth instruction than other methods, as for example oral hormonal contraception or intrauterine devices.
5. Conclusion
The possibility of saving taxpayer money through family planning has been convincingly ascertained through the calculations of pregnancy-related costs. What remains to be investigated is the possibility of saving taxpayer money also through the elimination of presently disseminated flawed information and replacing it by accurate, complete, and reliable information. Such a replacement will open new avenues for improved sex education and motivate an additional number of women to venture into birth control, especially those who prefer – for whatever reasons – natural family planning, ie, absence of hormones and devices as well as avoidance of adverse events and risks[31]. As in other societies,[32] a considerable segment of the U.S. population is dedicated to a “natural“ way of life and this segment might be motivated to embrace natural contraceptive methods so that the percentage of U.S. women who are presently not using contraception (38%) could be reduced significantly. There is good reason to conjecture that the ensuing increase in the use of contraceptive options will lead to a decrease of pregnancy-related costs and thus alleviate taxpayer burden.
6. Implications
In efforts to disseminate unadulterated information on contraception, each method should be assigned its proper failure rate figure without being subsumed under a general taxonomy. Concerning terminology, semantics established in scholarly research over the years should be employed, ie, calendar (after Knaus-Ogino), basal temperature (after van de Velde), cervical mucus (after Billings), and symptothermal (after Rötzer)[33]. Such a unified nomenclature will facilitate international scientific co operations, particularly in the face of additional methods derived from the original ones, eg, Two Day and Standard Days. Information on all available methods should be provided in accordance with the principle of informed consent so that each woman is enabled to make her well-reflected choice according to her own needs and convictions, as has been claimed as early as 2003[34]. Such a choice can be directed towards those methods that require a minimum of financial investment and thus allow also the individual consumer to benefit from reduced expenses for public health care.
References
- Vessey M, Lawless M, Yeates D, et al. Efficacy of different contraceptive methods. Lancet 1982; 1:841.
- Amy JJ, Tripathi V. Contraception for women: an evidence-based review. BMJ 2009, 330: b2895. Doi:10.1136/bmj.b2895.
- Secura GM, Madden T, McNicholas C, et al. Provision of no-cost, long-acting contraception and teenage pregnancy. N Engl J Med 2014; 371:1316-1323.
- Jacob JA. Health campaign focuses on teen sexual health. JAMA 2016; 315(4):336.
- Gossett DR, Kiley JW, Hammond C. Contraception is a fundamental primary care service. JAMA 2013; 309 (19): 1997-1998.
- Carolyn M. Controversy over contraception coverage. JAMA 2013; 310 (12):1287-1288.
- Cleland K, Peipert J, Westhoff C, Spear S, Trussell J. Family planning as a cost-saving preventive health service. N Engl J Med 2011; 364 (18).e37. Doi: 10.10561 NEJM p.1104373.
- Jones J, Mosher W, Daniel K. Current contraceptive use in the United States, 2006-2010, and changes in patterns of use since 1995. National health statistics reports; no 60. Hyattsville, MD: National Center for Health Statistics. 2012.
- New York Times. Accessed June 21, 2016, at: http://www.nytimes.com/health/guides/specialt opic/birth-control-and-family planning/print.html
- U.S. Department of Health. Accessed June 29, 2016,at:http://www.cdc.gov/reproductivehealth/ unintendedpregnancey/contraception.htm.
- Trussell J. Contraceptive efficacy. Table 3-2. In: Hatcher RA, Trussell J, Nelson AL, Cates W, Kowal D, Policar M. Contraceptive Technology: Twentieth Revised Edition. New York, NY: Ardent Media, 2011.
- Office of Population Affairs. Accessed June 21, 2016, at: http://www.hhs.gov/.../natural-family-planning-fact-sheet.
- Family doctor. Accessed June 21, 2016, at: http://www.familydoctor.org/familydoctor/en/p revention-wellness/sex-birth-control/natural-family-planning.
- Gesund und Leben in Niederösterreich. 2013; 06+07/13: 22.
- Frank-Herrmann P, Heil J, GnothC, et al. The effectiveness of a fertility awareness based method to avoid pregnancy in relation to a couple's sexual behaviour during the fertile time: a prospective longitudinal study. Human Reproduction 2007; 22(5): 1310-1319.
- Gröger S, Grüne B. Kontrazeption. In: Diedrich K, ed. Gynäkologie und Geburtshilfe. Berlin: Springer, 2000: 60-87.
- Food and Drug Administration. Accessed June 21, 2016, at: http://www.fad.gov/ForConsume rs/ByAudience/ForWomen/FreePublications/uc m313215.htm.
- Code of Medical Ethics. Current Opinions. American Medical Association. Chicago, Illinois: 1992, p.38.
- Womens-Health. Accessed July 2, 2016, at: http://www.Womenshealth.gov/publications/ou r-publications/fact-sheet/birth-control-methods.html.
- American Congress of Obstetricians and Gynecologists. Accessed June 21, 2016, at: http://www.acog.org/Womens-Health/Birth-Control-Contraception.
- American Congress of Obstetricians and Gynecologists (ACOG). Accessed Febr 14, 2017.at:www.acog.org/Patients/FAQs/Fertility- Awareness-Based-Methods-of-Family-Planning.
- Centers for Disease Control and Prevention. U.S. Medical Eligibility Criteria for Contraceptive Use, 2016. Accessed March 26, 2017,at:https://www.cdc.gov/mmwr/volumes/6 5/rr/rr650301.htm.
- University of Wisconsin. Accessed June 21, 2016,at:http://www.uwhealth.org/obgyn/tempor ary-contraception-options/13222.
- University of Maryland. Accessed June 21, 2016,at:http://www.umm.edu/health/medical/re ports/articles/birth-control-options-for-women.
- Milton S. Hershey Medical Center. Accessed June 21, 2016, at: http://www. Pennstatehers hey.ada.com/content.aspx?productId=111&pid =10&gid=000091.
- Trussell J. Contraceptive failure in the United States. Contraception 2011; 83(5):397-404. Doi:10.1016/j.contraception.2011.01.021Epub2 011Mar12.
- Beers MH, Berkow R, eds. MSD Manual. 1999 (17th ed.). Merck & Co. Inc. Whitehouse Station, N.J. USA.
- Freundl G, Sivin I, Batár I. State-of-the-art of non-hormonal methods of contraception: IV. Natural family planning. The European Journal of Contraception and Reproductive Health Care 2010; 15 (2):113-23. Doi: 10.3109/1362 5180903545302.
- Guttmacher Institute. AccessedJuly 2, 2016, at: https://www.guttmacher.org/factsheet/contrace ptive-use-united-states.
- Guttmacher Institute. Accessed July 2, 2016, at: https://www.guttmacher.org/news-release/ 2016/new-study-estimates-contraceptive-failure- rate.
- United Kingdom Government. Accessed June 21, 2016, at: http://www.nhs.uk/news/ 2009/ 08 August/Pages/Pillchoices.
- La grande Santé-France. Accessed June 21, 2016, at: http://www.lagrandesante.com/articles /sante/la-methode-sympto-thermique-de-regula tion-des-naissances.
- Kraetschmer K. Are women denied the right of self-decision in matters of family planning and birth control? Saarbrücken. Scholar's Press: 2017.
- American College of Obstetricians and Gynecologists. Birth Control. A woman's choice. Washington, D.C.: 2003.