Information
Journal Policies
Frozen Analysis in Borderline Ovarian Tumors: Accuracy Rates and the Affecting Factors
Funda Atalay1*, Cemal Atalay2, Hanife Saglam1, Nermin Atar2
2.SBU Ankara Numune Training and Research Hospital, Gynecology Clinic,Turkey
Copyright : © 2018 . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Aim: The objective of the present study was to evaluate the accuracy of frozen-section in borderline ovarian tumors and to find out the factors affecting the diagnostic accuracy.
Methods: A retrospective review of all patients treated for borderline ovarian tumors at Ankara Oncology and Ankara Numune Training and Research Hospital between 2010 and 2017 was performed. Thirty-nine patients were identified. The frozen section results were compared to the paraffin section results. Accuracy, over and underdiagnosis rates were determined. The factors affecting the frozen section accuracy were also evaluated using univariate analysis.
Results: In this retrospective study, 39 patients were evaluated. Agreement between frozen and paraffin sections was observed in 20/37 (54,05 %) patients. Misdiagnosis occurred in 17/37 (45.94%). In univariate analysis of our retrospective study, CA 125 level was significantly associated with misdiagnosis (p=0,037).
Conclusion: Frozen section in borderline ovarian tumors has low accuracy. Misdiagnosis was frequent and CA 125 level was significantly associated with misdiagnosis.
borderline ovarian tumors, frozen section, CA 125,Gynecology, Obstetrics
1. Introduction
Borderline Ovarian Tumors (BOTs), which were included in the literature after Taylor identified them as ovarian tumors that were different from benign and malign epithelial ovarian tumors, are differentiated from invasive epithelial ovarian tumors with lacking stromal invasion; and yet, they have proliferation and atypia [1]. BOTs constitute 10-20% of all ovarian malignities. They differ from epithelial ovarian cancer (EOC) with several characteristics of theirs. Unlike invasive EOCs, a total of 75% of BOTs are seen as FIGO Stage I during the time of diagnosis. In addition, they are detected at earlier ages, and their prognosis is better than in the patients who have EOC. In Stage 1 BOT, the average 5-year survival rate is 95-97%; and 65-87% even in Stage II and II BOTs [1,2].
In the treatment of it, surgery is the gold standard. The surgery must be planned in line with the age, fertility desire, stage and histopathological characteristics of the patient. Depending on the young age of the patient and the prognosis being better, the surgery that is preferred is the conservative surgery to preserve the fertility of the patient. As conservative surgery is adequate for surgical cure, the importance of intraoperative accurate histopathological diagnosis is critical [3,4].
The symptoms being non-specific, the lack of proper diagnostic tools, and contribution of tumor markers being absent in the differential diagnosis all make preoperative diagnosis difficult [1]. Intraoperative frozen examination is often employed to perform sufficient surgery. However, the diagnostic value of the ıntraoperative frozen examination is low in BOT [5-9].
The purpose of the present study was to investigate the diagnostic accuracy of intraoperative frozen section in BOTs, and to examine the factors affecting the ıntraoperative frozen examination results.
2. Material And Method
A total of 39 patients who were treated with the diagnosis of BOT at Ankara Oncology Training and Research Hospital, and Ankara Numune Training and Research Hospital between 2010 and 2017 were assessed retrospectively. The medical and surgical data of the patients, their follow-up data, and the relapse and recurrence data of them were received from the electronic registry system of the hospitals and via telephone from the patients. The age of the patients at diagnosis, histological subtypes, tumor size, primary surgery and staging procedures, postoperative treatment, follow-up, recurrence findings, and the latest status of the patients were all recorded. The patients were staged according to the 2014 Ovarian Cancer Staging System of the International Gynecology and Obstetrics Federation (FIGO). The histological classification was carried out in line with the histological classification of ovarian neoplasms of the World Health Organization (WHO). The patients underwent conservative or radical surgical treatment and full-staging according to their ages and fertility demands through intraoperative frozen examination. The conservative surgery was defined as cystectomy or unilateral (USO); and the radical surgery was defined as total abdominal hysterectomy bilateral salpingo-oophorectomy (TAH+BSO). The cytological examination, omentectomy, multiple peritoneal biopsy, and appendectomy were implemented as full-staging procedure. Unlike the epithelial ovarian tumors, the lymph node dissection (LND) was not considered as the part of full-staging, and was not routinely implemented. However, it was implemented to the patients who were foreseen to have clinical or radiological involvement.
The statistical analyses were carried out by employing IBM SPSS 23.0 Windows Statistical Package Program. A p value < 0.05 was taken to be significant at statistical level. The univariate analysis was employed to assess the factors that influenced the frozen examination.
3. Results
A total of 39 patients were evaluated retrospectively. The average age during the diagnosis was 47.48±13.85 (25-78); and 33.33% of the patients were below the age of 40. Frozen examination was carried out in 37 (94.9%) patients. The histopathological distribution was found as 23 (58.97%) serous BOT, 15 (38.46%) mucinous BOT and 1 (2.56%) Brenner tumor. The average tumor size was 9.65 cm (3-20 cm) in serous BOT cases, 19.66 cm (5-35 cm) in mucinous BOT cases, and 13.79 cm (3-35 cm) when all cases were considered. While unilateral tumor was detected in 29 (74.35%) cases, bilateral BOT was detected in 10 (25.64%) cases; it was determined that all of the bilateral tumors were serous BOT. According to the FIGO staging system, 33 (84.61) cases were Stage 1, and 6 (15.38%) cases were Stage 2. It was observed that the preoperative CA 125 values were 224.62IU/ml (5-2617 IU/ml) in average, and while the CA 125 values were above 35 IU/ml in 45.94% (17/37) of the cases; these rates were 47.61% (10/21), 46.66% (7/15) in serous and mucinous BOT in sub-group analysis, respectively. While the high CA 125 (>35IU/ml) values were found to be at a rate of 45.16% (14/31) in stage 1 cases, this rate was found to be 50% (3/6) in other stages. Fertility sparing surgery (FSS) was performed to 12 cases (30.8%), and radical surgery was performed to 27 (53.3%) cases. Cystectomy was performed to a total of 3 cases who underwent FSS (25%), USO was performed to 8 (66.7%), and USO + biopsy to the counterpart ovary was performed to 1 (8.3%) patient.
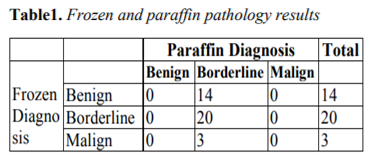
The intraoperative frozen examinations were reported as benign in 14 (35%) cases, borderline in 20 (51.3%) cases, and malign in 3 (7.7%) cases. It was observed that 37.83% (14/37) of the cases received underdiagnosis, 54.05% (20/37) received accurate diagnosis (20/37), and 8.10% (3/37) received overdiagnosis in the frozen examination (Table 1).
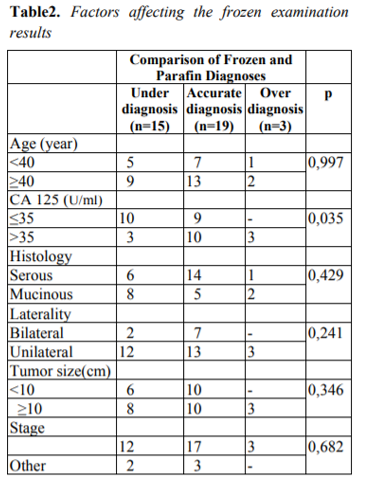
While the general accuracy rate of the frozen examination was 54.05% (20/37), this rate was 66.66% for serous BOT (14/21), and 33.33% (5/15) for mucinous BOT. The serum CA 125 levels were determined to be the factor affecting the frozen examination (p=0.035). The effect of age, tumor diameter, histologic type, stage and laterality on frozen examination results was not found to be significant in the statistical analyses (Table 2).
4. Discussion
It was observed in the present study that the age, histological type, FIGO stage, bilaterality and CA 125 results were similar to those reported in the literature.
The BOT being frequent in patients at reproductive age the prognosis being good, and cure rates being high even with conservative surgery have shown that fertility must be protected in these patients[3,4]. BOT is diagnosed histopathologically. The definitive diagnosis is carried out by examining the permanent sections after surgery. The frozen examination that is carried out during surgery is a method that is employed to avoid lacking or extra surgery in cases in whom malignant-benign differentiation cannot be made, and to manage the treatment in an accurate way. With this method, invasive ovarian cancers may be diagnosed accurately at a rate of over 90%. However, this rate is not as high as it is expected in BOT, and it may remain insufficient [10-13].
In BOT, the accuracy, sensitivity and specificity of frozen examination are 60-78%, 45-87% and 98%, respectively [5-12]. In the present study, it was observed that the frozen histopathological diagnosis was less than the actual one in 37.83% of the cases. While the general compliance rate of the frozen examination with the paraffin pathological examination was 54.05% (20/37), it was found as 66.66% (14/21) for serous BOT and 33.33% (5/15) for mucinous BOT. Although Basar et al. found the accuracy of the frozen examination in BOT as 62.7%, the sensitivity and positive predictive values were reported to be 71.2% and 84.1%, respectively [8].
Kolwijck et al. conducted a study and reported that there were high CA 125 (> 35 U/ml) levels at a rate of 53% in patients with BOT, and stated that the average CA 125 levels in serous BOT (59 U/ml) were higher compared to that in mucinous ones (25 U/ml) [13]. In the present study, it was found that the preoperative CA 125 values were 224.62 IU/ml in average were above 35 IU/ml in 45% of the cases, as in sub-group analyses for serous and mucinous BOT, they were 47.61% and 46.66% respectively. In the statistical study that was carried out, it was observed that the preoperative CA 125 values were the sole effect at statistically significant level on the frozen examination (p=0.035). The frozen examination results were reported as underdiagnosis in 42.85% of the patients who had CA 125 values < 35.
According to the results of the meta-analysis study that was conducted by Huang et al., it was demonstrated that there was a negative relation between the mucinous histology and frozen examination results; and this negative effect was associated with the mucinous tumors being larger than the serous tumors, and having benign, borderline and malignant components together [5]. Again, it was reported in a previous study that frozen examination accuracy rates were the lowest in the mucinous BOT [14]. In the study that was conducted by Kayıkcıoglu et al., again, the compliance between the frozen examination results and paraffin pathological diagnosis was 72%; and the inconsistency between the two pathological examinations was reported as 9% for serous types, and as 36.6% for mucinous types [10]. In the present study, it was shown that the histology had significant effect on the results of frozen examination, the compliance rates for frozen and paraffin examinations were found to be 66.66% for serous BOT; and 33.33% for mucinous BOT. In addition, the underdiagnosis rates were found as nearly two times higher in mucinous tumors when compared to the serous BOT (28.57% and 53.33%, respectively).
5. Results
In our study, it was demonstrated that the frozen examination accuracy rates were low in BOT. Although it was observed that the CA 125 values were the sole factor for the incompliance in frozen examination at a statistically significant level, and age, tumor size, laterality, and histological type had no significant effects on frozen examination results, it was also determined that the error margin increased especially in the presence of mucinous histology.
References
- Gökçü M, Güngördük K, Aşıcıoğlu O et al. Borderline ovarian tumors: clinical characteristics, management,and outcomes-a multicenter study. J Ovarian Res. 2016;9(66): 1-8
- Seong SJ, Kim da H, Kim MK, Song T.:"Controversies in borderline ovarian tumors". J Gynecol Oncol. 2015:26:343-9.
- Vasconcelos I, de Sousa Mendes M.:"Conservative surgery in ovarian borderline tumours: a meta-analysis with emphasis on recurrence risk". Eur J Cancer. 2015;51:620-31.
- Morice P.."Borderline tumors of the ovary and fertility". Eur J Cancer. 2006;42:149-
- Huang Z, Li L, Cheng CL et al. Diagnostic accuracy of frozen section analysis of borderline ovarian tumors: a meta-analysis with emphasia on misdiagnosis factors. J Cancer. 2018;9: 2817-24
- Gültekin E, Cingillioğlu B, Sayhan S et al. The value of frozen section evaluation in the management of borderline ovarian tumors. J Cancer Res Ther. 2017;7(4): 416-20.
- McCluggage WG.:"The pathology and controversial aspects of ovarian borderline tumors" . Curr Opin Oncol; 2010; 22(5):462-72
- Basaran D,Salman MC, Calis P, Ozek A, Ozgul N, Usubutun A, Yuce K.:"Diagnostic accuracy of intraoperative consultation (frozen section) in borderline ovarian tumours and factors associated with misdiagnosis". J Obstet and Gynecol. 2014;34: 429-34.
- Ilvan S, Ramazanoğlu R, Ulker –Akyıldız E, Calay Z, Beşe T, Oruc N.:"The accuracy of frozen section( intraoperative consultation) in the diagnosis of ovarian masses". Gynecol Oncol. 2005;97:395-9.
- Kayıkcıoglu F, Pata O, Cengiz S, Tulunay G, Boran N, Yalvac S, Kose F.:"Accuracy of frozen section diagnosis in borderline ovarian malignancy". Gynecol Obstet Invest. 2000.49:187-9
- Mederios LR, Rosa DD, Edelweiss MI, Stein AT, Bozzetti MC, Zelmanowicz A et al.: "Accuracy of frozen-section analysis in the diognosis of ovarian tumors: a systematic quantitative review". Int J Gynecol Oncol.2005; 15:192-02.
- Kim JH, Kim TJ, Park YG, Lee SH, Lee CW, Song MJ et al.:Clinical analysis of intra-operative frozen-section proven borderline tumors of the ovary". J Gynecol Oncol.2009;20,:176-80.
- Kolwijck E, Thomas CM, Bulten J et al. Preoperative CA 125 levels in 123 patients with borderline ovarian tumors. a retrospective analysis and review of the literature. Int j Gynecol Cancer.2009; 19:1335-8.
- Pongsuvareeyakul T, Kunamormpong S, Settakorn J, et al. Accuracy of frozen section diagnosis of ovarian mucinous tumors. Int J Gynecol Cancer. 2012;22(3): 400-6.