Information
Journal Policies
New Technologies and Reconstructive Surgery for Dysplasia and Cancer of the Vulva
Cherenkov V. G*
Copyright : © 2018 . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
With vulvar dysplasia, sclerotic deprive and suspected cancer under our observation there were 92 patients. The effectiveness of treatment of vulvar dystrophy (VIN I-II degree) by the method of photodynamic therapy (PDT) 45.8±4.7%. However, dysplasia II - III degree, sclerotic changes with the formation of pronounced horn scales prevents the full PDT and recurrence of the disease. Therefore, the treatment of choice is surgical treatment with a reconstructive plastic. The use of new reconstructive plastic surgery, including with the use of abdominal skin and fascial flap combined with vascularized lower segments of the rectus muscles (patent for invention No 2580665 from 11.11.14), have helped to reduce complications, improve cosmetic effect and reduce the duration of lymphorrhea in 2-3 days.
Comprehensive assessment and improvement of methods of diagnostics and treatment of vulvar dysplasias and early cancers.
vulvar cancer, PDT, cryoapplication, reconstructive plastic surgery of the abdominal skin and fascial and lower segments of the rectus muscles.
1. Introduction
Until recently, the main etiological factors of cancer of the vulva (RV) related disturbances in the neuroendocrine homeostasis. In the modern system of pathogenesis special attention is given papilloma infection (НРV). Latest play a leading role in the genesis of not only cervical cancer but also RVS that offers a new way to look at this problem [4,6]. Currently, PB is increasingly diagnosed in reproductive age, which in some way is connected with increasing frequency НРV of infection and incidence of vulvar intraepithelial neoplasia (VIN) among young women.
In 1993, the International society for the study of diseases of the vulva and vagina (ISSVD) and the International society of gynaecological pathology (ISGP), adopted a new classification of diseases of the vulva, which is based on pathological changes:
I. Benign Lesions of the Vulva
• Sclerotic zoster,
• Squamous cell hyperplasia
• Other dermatoses
II. Vulvar Intraepithelial Neoplasia (VIN)
1. Squamous vulvar intraepithelial neoplasia
• VIN 1 - corresponds to mild dysplasia of the vulva
• VIN 2 - corresponds to moderate dysplasia of vulva
• VIN 3 - corresponds to severe dysplasia of the vulva and Ca in situ.
2. Malosolenoj vulvar intraepithelial neoplasia
• Paget's Disease
• Melanoma in situ.
III. Invasive Cancer
Often one of the patients can observe the different pathological States that must be considered and classified.
Able to treat precancerous processes and prevent the development of cancer is difficult, but the real problem of modern gynecology [7, 8]. Some authors the solution to this problem is associated with the development of methods for cryosurgery, and PDT FDD [6]. Others believe that the organ-saving treatment of patients with neurodystrophic process, with a vulvar intraepithelial neoplasia and early cancer leads to relapse, and therefore in need of radical treatment [2, 3].
However, to date not solved the methodological aspects of detection and treatment of vulvar dysplasias and early cancers of the vulva. In works on RV [3, 7] indicate the importance of magnifying diagnosis and morphological methods. At the same time, stated that "the information content of the smears low" (up to 57% for summary data). "Often smears find only Horny scales and elements of inflammation, introducing the doctor astray".
2. Material and Methods
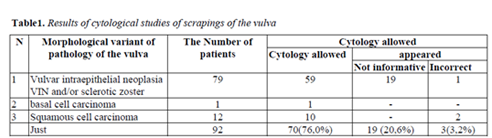
With vulvar dysplasia, sclerotic deprive and suspected cancer in regional oncologic dispensary from 2010 directed 92 of the patient. The examination we carried out with the use of colposcope (15 fold increase), allowing a high degree of confidence to select sites for target biopsy. Given the multicentric growth, as a rule, morphological study of vulvar dystrophies started with obtaining cytological material (smears and scrapings) from the suspicious areas (Figure1).
And only 20,6±1,5% were not informative. Have a 3.2±0.6% conclusion of catalogul was wrong. The sensitivity of Cytology in detecting different types of pathology NGOs amounted to 81.3±3.9 and ranged from 76% in vulvar intraepithelial neoplasia (VIN) to 97% at the pre - invasive forms of cancer.
In the literature available to us we have not found a description of the method of collection of material for cytological examination vulvar dysplasias as it is used for cytological screening of cervical cancer. Given that development of foci of RV occurs on the background of sclerotic zoster and increased keratinization of epithelial tissue, we used the technique of scraping with a scalpel consisting of two steps:
1) removing (scraping) keratinized scales of the epithelium of the 4-5 most suspicious areas; 2) scarification and receiving cells from deeper layers within the basal layer before the "dewdrops" of blood.
The results of cytological studies, we used incisional biopsy with a scalpel under local infiltration anesthesia (0.5% p-p of novocaine or lidocaine). And only when expressed scopinich and saucer-like forms of cancer a biopsy was performed by conchotomy. As can be seen from table 1, the cytological examination in 79 of the 92 patients with aimed vulvar dysplasia allowed at 76.0±3.4% of cases to establish a correct diagnosis, including 13 cases against this background, the cancer (stage 0-1), which is significantly higher than according to the literature - 57% [1, 2].
PDT we performed in 24 patients with diffuse vulvar dysplasia (VIN II-III) and PB to prepare the surrounding tissues, including 2 patients at relapse RV. As shown in Figure2, dysplasia and sclerotic zoster transferred to the skin of the thigh, which cannot be used for forming skin- fascial flap without PDT.
In their study, we used a second generation sensitizer – fotoditazin. Session of PDT was performed using 1.5-2 hours after intravenous drip infusion of the drug (LLC "Veta-Grand"), on average, 1.0 mg/kg of body weight in 100 ml of 0.9% solution of sodium chloride in terms of polystannanes of the room. Laser irradiation with a semiconductor device "Atcus-2" at the energy density of 80-250 j/cm2 of laser power output 1 W and the exposure time from 10 to 30 minutes depending on the area affected areas by scanning. Method involves generation of atomic (singlet) oxygen, leading to death of the atypical cells. After 1.5-3 months came healing and tissue repair without deformities in 9 women with barely visible scarring. Patients followed from 1 year to 3 years. Five women with repeated photodynamic therapy, however, complete cure has managed to achieve only two. Thus, the PDT allowed to cure vulvar dysplasia, only 11 of the 24 patients with I-II degree (45,8±4,7%). The renewal of the skin itch and residual lesions leukoplakia was observed in 13 women, due to the insufficient exposure of laser exposure on each zone, especially when there are significant Horny scales. Besides, PDT by moving the laser beam by hand does not allow to avoid subjectivity, and thus relapse. In such situations, in our opinion, requires an individual approach and combined treatment. As noted by the women themselves after PDT was only a temporary subjective effect, after which the itching resumed and they resorted to various folk remedies.
As noted by the women themselves after PDT was only a temporary subjective effect, after which the itching resumed and they resorted to various folk remedies For cancer of the vulva in order to avoid dispersion of tumor cells excision is always carried out radiowave scalpel and apparatus "Harmonics" In recent years, the excision of the tumor was preceded by her credibilitate to t - 185º using the apparatus ERBE, exposure 3-5 min (Figure3).
The results indicate the prospects of this approach, allowing a fixed tumor, it is more convenient to tighten and excise, to reduce blood loss.
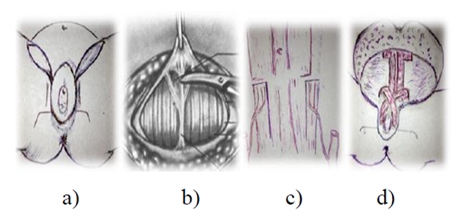
To improve quality, the formation of the amount of the external genitalia and reduce the lymphorrhea in recent times we have developed a method rekonstruktivnoi erasers (Patent No. 2580665 for invention dated 11.11.14) of the external genitalia through the mobilization of abdominal skin and fascial flap and the lower segments of the rectus muscles along with epigastrica inferior (Figure4, a), b), c) and d).
Closure of the wound was carried out at the beginning cross mobilized segments of direct muscles of a stomach on the vascular pedicle. Last create the missing volume of the labia majora and represent a unique plastic material for vascularization and lymph drainage. In the region of the decussation of the muscles and the ends of the segment performed the fixation to the muscles of the vagina with absorbable sutures so that they hung over the mouth of the urethra and did not close the symphysis of the pubic bones.
The next step was sutured fascia rectus muscles of the abdominal wall. Then put 6-7 stitches by Donati on the skin of the perineum and posterior vaginal wall tension in order to determine to what level will the skin defect to be filled abdominal skin and fascial flap with no tension.
Abdominal skin and fascial flap was laid on the wound surface, adapting it by cutting off the excess and sharp areas of the skin, stitches. Determining the projection of the abdominal flap, adjacent to the pubis, imposes two provisory internal anchor sutures to the periosteum, which is then stitched to the abdominal flap (without the skin), forming the genital fold.
Then through a separate puncture of the abdominal flap in the inguinal areas has introduced an active drainage in the inguinal- femoral area. Then every 0.7-0.8 cm for the tightness of stitches on the skin and the vaginal mucosa around the entire circumference and nodal skin sutures for Donati in inguinal- femoral area.
Surgery was performed in 12 women, mostly aged 45 to 55 years with abdominal obesity. The process is localized on the skin and mucosa of the anterior half of the vulva. In one case, focal leukoplakia was as an independent disease, in the other case was diagnosed with the initial cancer. Healing was by primary intention, with the exception of 1 woman (8,3±1,4%) with obesity and diabetes type II. An important aspect of reconstructive vulvectomy abdominal flap combined with segments of straight muscle on the vascular pedicle has been the reduction in the duration of lymphorrhea in 2-3 days, and the formation of the appearance of the organe.
3. Conclusions
1. The treatment of choice for vulvar dystrophy (VIN I-II degree) is PDT, which is in the diffuse forms the transition to the skin back of the thigh and with strong Horny scales should be used in combination with reconstructive plastic.
2. The use of reconstructive plastic surgery, including use of vascularized lower segment of the rectus abdomen is muscle is an individual method of choice in young women with cancer of the vulva and vulvar dystrophies (VIN II-III), a way of preventing the development of invasive forms of cancer, helps to reduce.
References
- Ashrafyan L. A., Kharchenko N. In.Kiselev V. I., etc. vulvar Cancer: etiopathogenic concept//Moscow,2006, 192 p.
- Gubaidulina T. N., Zharov V. A., Chernova L. F./Efficiency of surgical treatment of patients with background processes precancer and early cancer of the vulva with the use of reconstructive plastic surgery // Surgery. – 2008. - No. 2. – P. 48.
- Zharov A.V., Vazhenin, A.V., optimization of the treatment of patients with cancer of the vulva.- Chelyabinsk, 2005-131 with
- Buscema H. H. J. The Predomenance of human papillomavirus type 16 in vulvar neoplasia/J. Buscema, Z. Naghashfar,Sawada et al//Obstet. Gynecol. -1988.Vol.71, N4.- P. 601-606.
- Krikunova L. I., Kaplan M. A., Rykova E. V. the Role of photodynamic therapy in the treatment of vulvar cancer// 1 international conference. Obninsk , 1999.- p. 32-33.
- Urmancheyeva A. F. Epidemiology of cancer of the vulva. Risk factors and prognosis. Practical Oncology, vol. 7, No. 4, 189-196, 2006.
- Chulkova O. V., Novikova E. G., Sokolov V. V., Chulkov E. A.. Diagnosis and treatment of background and precancerous diseases of the vulva.//Practical Oncology "Tumor of the vulva and vagina", vol. 7, No. 4, 2006, 197-204.
- Knapstein P.G. Erweiterte Behand lungs mogli chkeiten das Vulvakarzinomas durch plastic reconstruktive Verfahren\ P.G. Knapstein, M. Mahlke, W.Poleska, W.Zeuner\\Zbl.Gynekol.- 1985.-Bd.107, N24.-p.1479-1487.