Information
Journal Policies
Impact of Adding a Sandwich Technique to a Stepwise Surgical Approach for the Conservative Management of Placenta Accreta Spectrum: (N & H Technique for Taming the Beast)
Hany F. Sallam*, Nahla W. Shady
Copyright : © 2018 . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Objective: To investigate the impact of adding a (Nahla&Hany) sandwich technique(N&H), (double transverse compression Suture at the lower uterine segment plus Intrauterine inflated Foley’s Catheter Balloon at the lower uterine segment) to stepwise surgical approach for the conservative management of placenta accretaspectrum (PAS) for decrease measured blood loss during and after a caesarian section.
Methods: A single center retrospective case–control clinical trial was carried out in a tertiary university hospital between March 2015 and March2018; 142 women were undergoing cesarean delivery for PAS were managed conservatively either with Stepwise surgical approach alone (71 patients in group I), or Stepwise surgical approach plus (H&N sandwich) technique (71 patients in group II) to control intra-operative blood loss and post-partum hemorrhage.
Results: There was a great reduction in intra operative blood loss in group II (913.8± 191.83) compared with Group I (1397.04± 305.53) (P=0.0001). Also, there was a great reduction in postoperative bleeding either vaginal bleeding or blood in the intra abdominal drain in group II than group I (p=0.0001 and 0.0001). Hence the total estimated blood loss in group II (1150.85± 243.39) showed highly reduction compared with group I (1726.06± 368.94) (P=0.0001).
Conclusion: Application of an Adjunctive sandwich technique for the conservative management of PAS (N&H technique) adding to Stepwise surgical approach is a novel approach, simple, safe and effective to decrease blood loss and may preserve the uterus as possible and decreases the need for the invasive internal iliac artery ligation(IIAL).
Abbreviations: PAS-placenta accreta spectrum, N&H-Nahla&Hany, CD-cesarean delivery, PPH- postpartum hemorrhage, IIAL-internal iliac artery ligation
Key message: The authors study the impact of adding N&H sandwich technique to a stepwise surgical approach to the conservative management of PAS which showed to be a novel approach, simple, safe, universally achievable and effective to decrease blood loss and may preserve the uterus and decreases the need for the invasive IIA ligation.
Placenta accreta spectrum, post-partum hemorrhage, Foley’s Catheter Balloon.
1. Introduction
PAS represents one of the most night mare's conditions in modern obstetrics, with high rates of hysterectomy, hemorrhage and intensive care unit admission [1]. The term PAS implies abnormal implantation and invasion of the placenta into the uterine wall. This term has been used to describe placenta accreta, increta, and percreta. Placenta accreta occurs when the placental villi adhere directly to the myometrium, with no normal intervening deciduabasalis layer. Cases with partial or complete invasion of trophoblast through the uterine wall are called increta and percreta, respectively, though all three categories are collectively identified as accreta in the epidemiologic literature [2].
PAS appears to be on the rise paralleling the rise in cesarean delivery (CD) rate as a major risk factor [3].
PAS is one of the most common reasons for cesarean hysterectomy [4] which associated with high rates of severe maternal morbidity (40%–50%) [4], with reported mortality rates up to 7%. And, might not be considered first-line treatment for women who have a strong desire for future fertility [5].
Conservative management of PAS defines all procedures that aim to avoid peripartum hysterectomy and its related morbidity and consequences.
The main types of conservative management which have been described in the literature: [8]. the extirpative technique (manual removal of the placenta); [7] leaving the placenta in situ or the expectant approach; [6] one-step conservative surgery and [9] the Triple-P procedure. These methods have been used alone or in combination and in many cases with additional procedures such as those proposed by interventional radiology.
Insertion of intrauterine balloon tamponade has been suggested in the management of massive postpartum hemorrhage (PPH). The Bakri balloon has a sausage-like spindle shape and a drainage lumen and is made of silicon. It has been used in cases of uterine atony and placenta previa with a success rate of 90% [10]. However, Bakriballoon is not available in all countries.
Till now there are debates about the optimal conservative management protocols of PAS, although primary goals in PAS is to prevent intraoperative and post-operative hemorrhage, the ideal treatment of MAPP should restore the uterine anatomy and ensure a new pregnancy with minimal risk of complications. The ideal treatment of PAS still elusive and debatable. With the rising incidence of abnormal placentation, it is important to define management strategies with a focus on reducing maternal morbidity and mortality mainly decrease PPH [11]. N&H technique was successfully used for control of blood loss during cesarean section for placenta previa [12].
So, the aims of our study to assess the effect of adding double Transverse Compression Suture at the lower uterine segment plus Intrauterine inflated Foley's Catheter Balloon(N&H technique) on measured blood loss during and after a caesarian section in patient undergone Stepwise surgical approach during cesarean section due to PAS, aiming for conservative management.
2. Materials And Methods
A retrospective study was conducted using data from 142CD recorded in the Department of Obstetrics and Gynecology, Aswan University Hospital in Aswan, Egypt. Which is a tertiary referral medical center for high-risk pregnancy, between March 1, 2015, and March 1, 2018? Aswan University Hospital conducts an average of 18322 deliveries per year. The study was approved by Institutional research board.
Study inclusion criteria were women undergoing elective cesarean delivery for PAS which not respond to simple hemostatic maneuvers like uterine artery ligation and placental bed hemostatic sutures. Diagnosis of PAS based on ultrasound in which one or more of ultra- sonographic features were present: 1- loss of the retro placental clear space. 2- Thinning of the myometrium overlying the placenta. 3-multiple irregular placental lacunae with a "moth-eaten" or "Swiss cheese" appearance of placenta. 4- turbulent blood flow through the lacunae on Doppler velocimetry. This ultra-sonographic feature confirmed at cesarean section by placental adherence requiring digital separation.
Women with any of the following criteria were excluded from the study: 1-Patients with cardiac, hepatic, renal or thromboembolic disease. 2-patients with placenta percreta (ultrasound features showed invasion of the placenta into the bladder or increased vascularity of the uterine serosa–bladder interface). 3-patient show to have placenta previa without signs of invasion (placenta previa without accreta). 4-women with inappropriate data.
As a routine in our hospital, all women diagnosed to have PAS were admitted in the third trimester of pregnancy and were subjected to full precise history taking, complete laboratory investigations, fetal surveillance by ultrasound scanning and cardiotocography, and antenatal administration of corticosteroids to enhance the fetal lung maturity. Maternal demographic and clinical characteristics and ultrasound findings were recorded in a database. The operative details and maternal and neonatal outcomes were collected into the same database.
All women were informed about the N&H technique, the technique of Stepwise surgical approach and the risk of Intraoperative hemorrhage and PPH, the need for blood products transfusion, and the possibility of cesarean hysterectomy if needed to control severe bleeding. A written informed consent was taken from each woman before performing any intervention. Moreover, a written permission was obtained from each woman to use her data for research purposes.
3. Intervention
Elective CS was planned at 37–38 weeks of gestation. An adequate amount of blood products was prepared to be available for transfusion. Delivery was performed by the same multidisciplinary team, including two expert obstetricians, an assistant, an expert anesthesiologist, and a pediatrician. All participants received general anesthesia. Two 16-gauge intravenous (IV) cannulas were inserted in 2 large forearm veins before induction of anesthesia, and one 16-gauge IV cannula was inserted in the external jugular vein after induction of anesthesia.
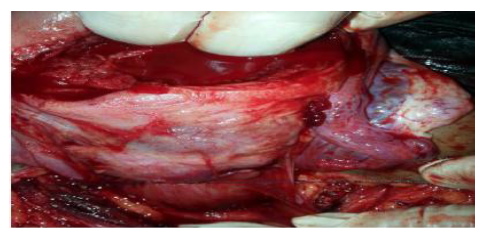
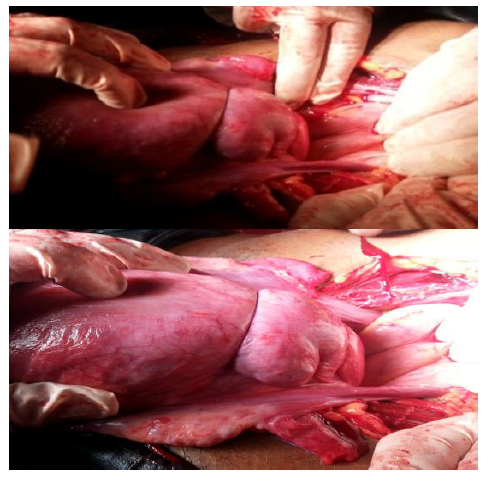
The abdomen was exposed through Pfannenstiel incision, after skin incision, the subcutaneous fat and abdominal fascia were opened crosswise, and the rectus muscle was opened on the midline, the parietal peritoneum was opened longitudinally, the visceral peritoneum was opened transversely and dissected downwards with the bladder and kept against symphysis pubis by a Doyen retractor, followed by transverse incision of the uterus with avoidance of transplacental incision which provokes severe bleeding. The fetus was delivered.
The uterus with the placenta inside was exteriorized quickly after extraction of the fetus while it was still not contracted to facilitate its exteriorization through the abdominal incision. The uterus (including placenta) is exteriorized and compressed against the symphysis pubis by assistant to minimize blood loss by direct pressure and kink of uterine vessels. The uterine artery was ligated bilaterally; then, the placenta was separated. Hemostatic sutures were applied in the uterine wall to control bleeding from the placental bed as much as possible.
internal iliac artery ligation (IIAL) was done if needed by Transabdominal/Trans peritoneal Approach.
Any observed bleeding should be dealt with in the usual way.
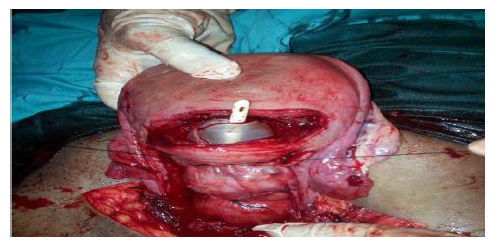
after acceptable control of bleeding from the placental bed, the internal os of the cervix was identified a double uterine compression suture at the lower uterine segment with inflated Foley's catheter balloon tamponade was performed as follow:
- 100-cm Vicryl no. 1 was thrown to form two nearly equal parts (each 50 cm) on a blunt semicircular 70-mm needle, the curve of the needle was straightened.
- The needle transfixed the right side of the uterine wall from anterior to posterior, about 5 cm below the hysterotomy incises posterior, then the needle transfixed the left side of the uterine wall from posterior to anterior, about 2 cm below the hysterotomy incision.
- another transverse compression suture undertook above the first one by 3 cm and below the hysterotomy incision by 2 cm.
- At the end of the suture application and before tying the knots, the internal os of the cervix was identified and a double-way 20 Fr Foley"s catheter with a 30-50-ml balloon (Amecath, Ameco Medical Industries, 10th of Ramadan City, Egypt) was inserted through the cervix to be handled by an assistant through the vagina and fixed to the patient‟s lower limb after inflation of the catheter balloon by 80 ml warm saline and pulling it against the lower uterine segment between the two transverse sutures . Only one catheter was used for tamponade.
- Lastly ties the sutures.
In both groups, all women received misoprostol 600 mcg (three tablets of MisotacR, Adwia Co, 6th October city, Egypt) rectal, as well as 20 IU of oxytocin (Syntocinon, Sanofi Aventais, Egypt) in 500-mL lactated Ringer‟s solution as an intravenous infusion.
Internal iliac artery ligation (IIAL) was done if needed by Transabdominal/Trans peritoneal Approach.
A wide pore drain was then inserted in the Douglas pouch, and the abdominal wall was repaired. The intrauterine inflated Foley's catheter balloon was left in place for 24 h after the operation and then removed.
Finally, the uterus was closed in three layers and pelvic drain was inserted in Douglas pouch in all patients followed by standard repair of abdominal wall.
Cesarean hysterectomy was performed if conservative approach failed to control bleeding during CD in both groups.
Blood loss was estimated by a combination of direct measurement and gravimetric method.
The primary outcome was estimation of intraoperative, postoperative, total blood loss (ml) and the incidence of invasive surgical procedures as cesarean hysterectomy or IIAL.
The secondary outcome measures included pulse rate, blood pressure and temperature which recorded continuously intraoperative, then every 30 minutes after operation therefor the mean were calculated. Also measures included the need for blood transfusion ≥ 4 units, operative time, period for hospitalization bladder injury and 24 hours postoperative hemoglobin concentration. After collecting all the data, the data were tabulated and analyzed.
4. Statistically Analysis
Data were entered and statistically analyzed using the Statistical Package for Social Sciences (SPSS) version 16. Qualitative data were described as numbers and percentages. Chi- square test was used for comparison between groups. Quantitative data were described as means (SD) after testing for normality by Kolmogorov-Smirnov test. Independent sample t-test was used for comparison between groups. Odds ratios and their 95% confidence interval were calculated. "p-value ≤ 0.05" was statistically significant.
5. Results
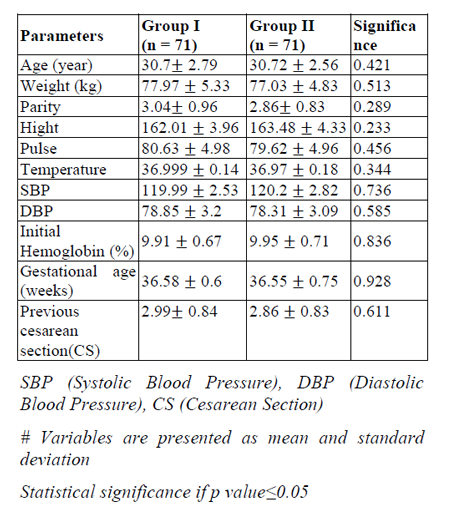
There was no significant difference between the two groups with respect to their age, weight, height, parity, gestational age, pre-operative pulse, systolic blood pressure (SBP), diastolic blood pressure (DBP), temperature, initial hemoglobin and number of previous cesarean sections (CS) (Table1).
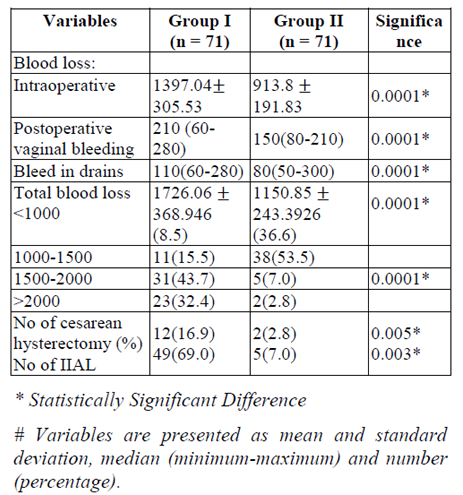
There was a great reduction in intraoperative blood loss in group II (913.8± 191.83) compared with Group I (1397.04± 305.53) (P=0.0001).
Also, there was a great reduction in post- operative bleeding either vaginal bleeding or blood in intraabdominal drain in group II than group I (p=0.0001 and 0.0001) Hence the total estimated blood loss in group II (1150.85± 295.46) showed highly reduction compared with group I (1726.06± 243.39) (P=0.0001).
The incidence of cesarean hysterectomy was decreased in group II (2.8%) than group I (16.9%), this reduction showed significant difference (p=0.005), also the incidence of IIAL was decreased in group II (7%) than group I (69%) (Table2).
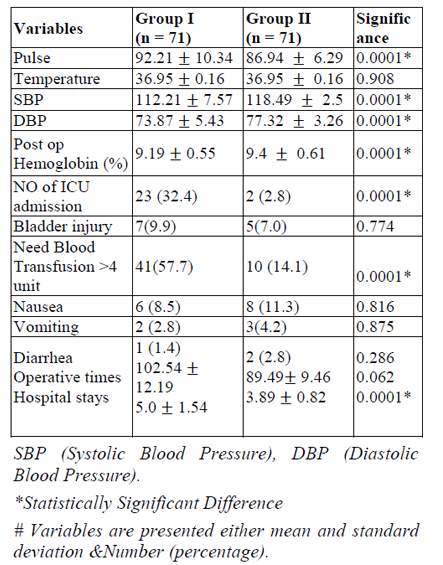
The number of patients need blood transfusion ≥ 4 bags was significant increase in group I; [41 patients (57.7%)] versus 10 patients in group II (14.1%). (P=0.0001). Also, the number of patients need admission to ICU were significant increase in group I [23 patients (32.4%)] versus 2 patients in group II (7%) (P= 0.0001). The mean post-operative hemoglobin in group I was (9.19±0.55) and in group II was (9.4±0.61) with statistically significant difference (p=0.0001).
There was significant increase in postoperative hospital stay in group I (5.0±1.54) compared with group II (3.89±0.82) (p=0.0001). There was a significant increase in post-operative pulse in group I (92.21± 10.34) compared with Group II (86.94± 6.92). (P= 0.0001). Also, there was significant decrease in both post-operative SBP (112.21± 7.57) and DBP (73.87± 5.43) in group I compared with SBP (118.51± 2.46) and DBP (77.04± 3.44) in group II (P=0.0001 and 0.0001).
There was no significant difference between both groups with respect to post-operative temperature, incidence of urinary bladder injury and operation time. (P=0.687, 0.774, and 0.062 respectively) (Table3).
6. Discussion
N&H sandwich techniques (double Transverse Compression Suture at the lower uterine segment plus Intrauterine inflated Foley‟s Catheter Balloon) adding to Stepwise surgical approach during CD due to PAS an alternative procedure to cesarean hysterectomy with the advantage of preserving future fertility in addition to less operative time, lesser cost, less chances of operative complications like bladder injury and post-operative adhesion formation.
Many "uterine sandwich" techniques have been described in the literature to achieved hemostasis for cesarean bleeding, [13,-15] with all using Hayman suture [15] or B-Lynch [13,14]. Many balloons have been used in the literature , such as simple condom, Sengstaken- Blakemore tube, and Foley, Rusch or Bakri catheters [30].In our study we use Foleys catheter balloon which is effect and cheap and available in our locality.
Preventive devascularization can be achieved by techniques used to treat PPH (embolization, bilateral uterine artery ligation, stepwise uterine devascularization, bilateral ligation of hypogastric arteries), although these uterine- sparing procedures may be less effective in cases of PAS[17,18].
We introduced an adjunctive novel (N&H technique), to achieve hemostasis from lower uterine segment at the placental bed during cesarean section in which we perform double transverse suture plus intrauterine inflated folly's balloon tamponade which compress the lower uterine segment and make an efficient tamponade to control bleeding from the placental bed. N&H technique makes anatomic and physiologic sense.PAS is one of the major causes of major bleeding during CD. In most cases of PAS, the potential for rapid blood loss during CD for PAS demands that obstetricians must prepare an emergent situation during CD of PAS. But there are few methods to manage intra-operative bleeding safely and immediately [31].
N&H technique could successfully control severe hemorrhage from a lower uterine segment of a patient with PAS. This technique is simple to use, scarcely invasive, and available at a low cost to all maternity wards and should be considered as one of the first management options to reduce the risk of undesirable hysterectomy.
In the current study, prophylactic use of adjunctive sandwich (N&H) technique for the conservative management of PAS is effectively reduced intra-operative, post-operative blood loss, blood transfusion needs more than 4 IU as well as lower the incidence of PPH due to PAS as compared with stepwise uterine devascularization alone. Also, associated with a decrease in cesarean hysterectomy for post- partum hemorrhage.
The greatest challenge in modern obstetrical care is the surgical management of PAS. With the recommended action in the management of PAS from the American College of Obstetrics and Gynecology being cesarean hysterectomy, [4] which associated with high rates of severe maternal morbidity (40%–50%) [4], with reported mortality rates up to 7%. And, might not be considered first-line treatment for women who have a strong desire for future fertility [5,31].
IN agreement with our work, Melekoglu Rauf et al (2017), investigate maternal outcomes of conservative management of post-partum hemorrhage due to PAS using IIAL and endo- uterine hemostatic suture to lower uterine segment. Patients, who were managed conservatively with IIAL and endo-uterine hemostatic suture to control post-partum hemorrhage secondary to PAS, suffer from lower hysterectomy rate compared with the other conservative methods reported in the literature [16].
Many complications have been described in association with IIAL to be 22.6%, including buttock claudication (12.2%), buttock necrosis (4.8%), spinal cord ischemia (4.0%), colonic ischemia (2.5%), and bladder necrosis (0.8%). Furthermore, IIAL is associated with serious intraoperative complications like internal iliac venous injury and ureteral damage. [19,[20,29].In our study, we did not encounter any serious intraoperative complications.
The overall success rate of N&H technique in our study was 97%, to preserve the uterus and control hemorrhage from the lower uterine segment which is comparable to previous studies with various conservative techniques [21-27].
The success rate of stepwise surgical approach for PPH has been reported as 42–75% in previous works[21-23]. Yildirim et al. [23] also stated it as high as 90% in their study. In our study, the success rate of stepwise surgical approach for PPH is in concordance with other studies and this may be due to early resort to stepwise surgical approach for patients with PAS. In our study stepwise surgical approach refrain hysterectomy in 83% of the patient, with adding N&H technique refrain hysterectomy in97% of the patients, and this agreed with the literature [25-27].
Palacios-Jaraquemada et al. described outcomes of one-step conservative surgery on 68 women presenting with PAS. Uterine preservation was achieved in 95.7% (44/46) and 27.3% (6/22) of cases, respectively. (28)
The main limitation of our study was probably related to the lack of blinding and randomization. Additionally, the small sample size of the included women may limit the generalizability of the results. Finally, limitations of our study include those inherent to retrospective nature. Future studies designed prospectively with a large sample size need to be performed to further clarify the place of N&H technique in the conservative management of PAS.
7. Conclusion
The results of this study highlight that: Application of an Adjunctive sandwich technique (N&H technique) for the conservative management of PAS adding to Stepwise surgical approach is a novel approach, simple, safe and effective to decrease blood loss and may preserve the uterus as possible and decreases the need for the invasive IIA ligation. And may become an alternative valid option to planned cesarean-hysterectomy in well-selected cases who have a strong desire for future fertility.
8.Conflict of Interest
The authors declare that they have no conflict of interest.
References
- Grobman WA, Bailit JL, Rice MM et al. Frequency of and factors associated with severe maternalmorbidity.Obstet Gynecol. 2014 Apr;123(4):804–810. PubMed PMID: 24785608. PubmedCentralPMCID: 4116103.
- Silver RM. Abnormal placentation: Placenta previa, vasa previa, and placenta accreta. Obstet Gynecol.2015 Sep; 126(3):654–668. PubMed PMID: 26244528.
- Morlando M, Sarno L, Napolitano R Et al. Placenta accreta: Incidence and risk factors in an area with a particularly high rate of cesarean section. Acta ObstetGynecol Scand. 2013; 92(4):457–460. PubMed PMID: 23347183.
- Sentilhes L, Goffinet F, Kayem G. Management of placenta accreta. Acta ObstetGynecol Scand. 2013; 92:1125–1134
- Alchalabi H, Lataifeh I, Obeidat B, et al. Morbidly adherent placenta previa in current practice: prediction and maternal morbidity in a series of 23 women who underwent hysterectomy. J Matern Fetal Neonatal Med. 2014; 27(17):1734–7.
- Eller AG, Porter TF, Soisson P, Silver RM. Optimal management strategies for placenta accreta. BJOG.2009; 116:648–654.
- Sentilhes L, Ambroselli C, Kayem G, et al. Maternal outcome after conservative treatment of placenta accreta. Obstet Gynecol. 2010; 115:526–534.
- Kayem G, Davy C, Goffinet F, Thomas C, Clement D, Cabrol D. Conservative versus extirpative Management in cases of placenta accreta. Obstet Gynecol. 2004; 104:531–536.
- Teixidor Vinas M, Belli AM, Arulkumaran S, Chandraharan E. Prevention of postpartum hemorrhage and hysterectomy in patients with morbidly adherent placenta: A cohort study comparing outcomesbbefore and after introduction of the Triple-P procedure.Ultrasound Obstet Gynecol. 2015; 46:350–355
- Nagai S, Kobayashi H, Nagata T, et al. Clinical usefulness of Bakri balloon tamponade in the treatment of massive postpartum uterine hemorrhage. Kurume Med J. 2016;62(1–2):17– 21
- Kaya, Z. Damarer, K. Daglar, O. Unal, A. Soli man, O. GuralpIs there yet a role for internal iliac artery ligation in obstetric hemorrhage with the current gain in popularity of other uterus sparing techniques J Matern Fetal Neonatal Med, 30 (2017), pp. 1325-1332
- Hany F. Sallam&Nahla W. Shady :A sandwich technique (N&Hvariation technique) to reduce blood loss during cesarean delivery for complete placentaprevia: a randomized controlled trial, The Journal of Maternal-Fetal & Neonatal Medicine(2018):,DOI:10.1080/14767058.2018.1457643
- Danso D, Reginald P. Combined B-lynch suture with intrauterine balloon catheter triumphs over massive postpartum haemorrhage. BJOG 2002; 109: 963.
- Nelson WL, O'Brien JM. The uterine sandwich for persistent uterine atony: combining the B- Lynch compression suture and an intrauterine Bakri balloon. Am J ObstetGynecol 2007; 196: e9–e10.
- 3Yoong W, Ridout A, Memtsa M et al. Application of uterine compression suture in association with intrauterine balloon tamponade („uterine sandwich‟) for postpartum hemorrhage. Acta ObstetGynecolScand 2012; 91: 147–151.
- Rauf, M., Ebru, C., Sevil, E., and Selim, B. (2017) Conservative management of post- partum hemorrhage secondary to placenta previa–accreta with hypogastric artery ligation and endo-uterine hemostatic suture. J. Obstet. Gynaecol. Res., 43: 265–271. doi: 10.1111/jog.13215
- Sentilhes L, Trichot C, Resch B, et al. Fertility and pregnancy outcomes following uterine devascularization for severe postpartum haemorrhage. Hum Reprod. 2008; 23:1087– 1092.
- Sentilhes L, Gromez A, Clavier E, Resch B, Verspyck E, Marpeau L. Predictors of failed pelvic arterial embolization for severe postpartum hemorrhage. Obstet Gynecol. 2009; 113:992–999
- Joshi VM, Otiv SR, Majumder R, Nikam YA, Shrivastava M. Internal iliac artery ligation for arresting postpartum haemorrhage. BJOG 2007; 114: 356–361.
- Chitragari G, Schlosser FJ, Ochoa Chaar CI, Sumpio BE. Consequences of hypogastric artery ligation, embolization, or covera. J Vasc Surg. 2015; 62:1340–1347
- Clark SL, Phelan JP, Yeh SY, Bruce SR, Paul RH. Hypogastric artery ligation for obstetric hemorrhage. Obstet Gynecol1985; 66: 353– 356.
- Das BN, Biswas AK. Ligation of internal iliac arteries in pelvic hemorrhage. J ObstetGynaecol Res 1998; 24: 251–254.
- Papp Z, Tóth-Pál E, Papp C Et al. Hypogastric artery ligation for intractable pelvic hemorrhage. Int J Gynaecol Obstet2006; 92: 27–31.
- Yildirim Y, Gultekin E, Kocyigit A, Yilmaz C, Ertopcu K, Arioz DT. Color Doppler analysis of pelvic arteries following bilateral internal iliac artery ligation for severe postpartum hemorrhage. Int J GynaecolObstet 2009; 104:22–24.
- Simsek Y, Yilmaz E, Celik E, et al. Efficacy of internal iliac artery ligation on the management of postpartum hemorrhage and its impact on the ovarian reserve. J Turk Soc Obstet Gynecol. 2012;9(3):153–8
- Patil Y, Kathiriya D, Kshirsagar NS, et al. Role of Internal Iliac Artery Ligation in Control of Pelvic Haemorrhage. Int J Recent Trends Sci Technol. 2014;9(3):461–4
- Naithani V, Solanki J. Bilateral internal iliac artery ligation-a boon for severe post-partum hemorrhage. J Evol Med Dent Sci. 2013;2(9):4
- Palacios-Jaraquemada JM. Placental Adhesive Disorders. Berlin/Boston, MA: Walter de Gruyter; 2012.
- Simsek Y, Yilmaz E, Celik E, et al. Efficacy of internal iliacartery ligation on the management of postpartum hemorrhage and its impact on the ovarian reserve. J Turk Soc Obstet Gynecol. 2012; 9(3):153–8.
- Georgiou C. Balloon tamponade in the management of postpartum haemorrhage: a review. Br J Obstet Gynaecol.2009; 116:748– 57.
- A.C. Rossi, R. H. Lee, and R. H. Chmait, "Emergency postpartum hysterectomy for uncontrolled postpartum bleeding: a systematic review," Obstetrics and Gynecology, vol. 115, no. 3, pp. 637–644, 2010.