Information
Journal Policies
Uterine Arteriovenous Malformation with Failed Uterine Artery Embolization: A Case Report
Servet Gencdal1*, Nihan Kiziltug1, Emre Destegul2, Oznur Bilge1, Zafer Kolsuz1, Emre Ekmekci3
2.NigdeOmerHalisDemir University, Faculty of Medicine, Education and Research Hospital Department of Obstetrics and Gynaecology, Nigde, Turkey.
3.Sanlıurfa Education and Research Hospital, Department of Obstetrics and Gynaecology, Sanlıurfa, Turkey.
Copyright : © 2018 . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Uterine arteriovenous malformation (AVM) is a rare condition, with fewer than 100 cases reported in the literature. Despite it being rare, it is a potentially life -threatening condition. This case report describes a 34-year-old woman who presented with heavly hemorrhage. She was given a course of hormonal therapy and 4 units of blood and no conclusive diagnosis was attained. Transvaginal ultrasound (TVUS) of the pelvis showed increased vascularity with multidirectional flow of the uterus and a prominent vessel. A uterine artery angiogram confirmed an AVM in the fundal region with an early draining vein. Embolisation of the AVM was performed successfully. Unfortunately, it did not work . Patient's bleeding was still continuing. Hysterectomy was done as last option.
Arteriovenous Malformation, Doppler Ultrasonography, Embolisation, Hysterectomy.
1. Introduction
Arteriovenous malformation (AVM) can be found anywhere in the vascular system, including the uterus [1]. Uterine arteriovenous malformation (UAVM) is a rare condition, with fewer than 100 cases reported in the literature [2].It is a potentially life-threatening condition, as patients may present with profuse bleeding. It can be congenital or acquired. Congenital uterine AVM arises from an abnormality in the embryological development of primitive vascular structures. Acquired uterine AVM occur following surgical procedures such as dilatation and curettage, uterine surgery, or direct uterine trauma and are less commonly associatedwithvariousgynecological malignancies [3]. Colour Doppler ultrasound (US) provides a non invasive method for initially diagnosing this rare condition and confirmation can be made using diagnostic angiography. There are several treatment options for UAVM. In hemodynamic stable patients expactant management, medical therapy, uterine arter embolization (UAE). Even hysterectomy may be necessary for patients with severe bleeding [4]. This case report describes a previously undescribed manifestation of AVM which was successfully treated with hysterectomy.
2. Case Report
A 34-year-old woman was seen at our facility who presented with heavy vaginal bleeding. She presented prolonged and profuse vaginal bleeding for six months. The patient recounted a unremarkable medical history, specifically noting a gynecologic history of menorrhagia, with multiple hospital admissions for severe genital tract bleeding. She was given a course of hormonal therapy and 4 units of blood and no conclusive diagnosis was attained. The patient denied a family history of bleeding disorders. Her previous menstrual cycles had been regular and her last menstruation was one month previously. She had a history of two cesarean sections, three artificial dilation and curettage and one hysteroscopy for diagnosis. On observation of the uterine cavity at the time of diagnostic hysteroscopy, there were no abnor-mal findings. She was hemodynamically stable at admission. On pelvic examination, uterus was normal in size, shape, and was non tender. Her Hb was 9.3g/dl, HCT was 28.1% and human chorionic gonadotropin (hCG) level was less than 2 mIU/mL. Upon admission, there was no evidence of active vaginal bleeding. Transvaginal ultrasonography (US) revealed tubular inhomogeneous echoic mass in the uterus (Figure 1).
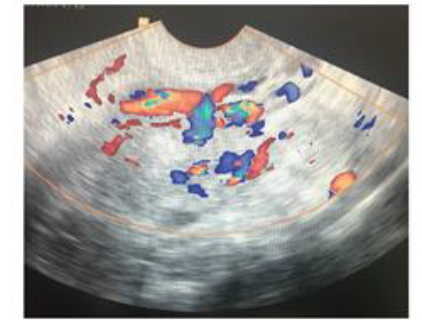
The lesion manifested numerous irregular, tubular, anechoic structures. These structures generated a multi-directional and turbulent flow on color Doppler US (Figure 2). A diagnosis of an AVM was considered and required an angiogram for confirmation. Angiography revealed enlarged left-sided uterine arteries with brisk drainage into the uterine veins, consistent with AVM. After informed consent was taken and mild sedation with fentanyl, antegrade puncture of right common femoral artery was done followed by placement of 6F vascular access sheath. Thereafter, left uterine artery was engaged with 5F C2 catheter and angiography was done which revealed a large tuft of serpiginous arteries arising from left uterine artery and draining into the dilated venous system Thereafter, the uterine artery was selectively injected with slow injection of PVA particles of 300-500 micron till sluggish flow was seen which was followed by injection of gel foam slurry till complete cessation of flow was seen. There was inadvertent dissection of short segment of uterine artery near origin during procedure, which resolved during later part of procedure. No complications were encountered.
The patient's vaginal bleeding did not decreased post-embolisation. Regular follow-up transvaginal US revealed that the lesion had not been gradually shrinking. Three months after undergoing UAE, hysterectomy was performed.
3. Discussion
The true incidence of uterine AVM is unknown. According to a literature review, uterine AVM are most frequently encountered in women of reproductive age (mean age, 30±9.1 years); in fact, 96% of patients are premenopausal women [5]. Thus, it is an important differential to be considered in women of reproductive age with unexplained vaginal bleeding and in post-menopausal women when anechoic structures are identified by US [6]. It can be either congenital or acquired (traumatic) lesions. In most cases, uterine AVM is acquired, and has been reported as a consequence of previous pelvic surgery, curettage, treatment by intra-uterine device, delivery, pathologic pregnancy-related events such as GTD, gynecologic malignancy, infection and maternal exposure to diethylstilbestrol [7]. Uterine AVM is a potentially life-threatening disorder in which patients present with vaginal bleeding that may be profuse and cause hemodynamic instability. The diagnosis of AVM can be critical, as endometrial curettage can catastrophically worsen bleeding from this vascular malformation. Our patient presented prolonged and profuse vaginal bleeding for six months and taking a course of hormonal therapy and several units of blood, also she had underwent one dilation and curettage procedure and one hysteroscopy for diagnosis, unfortunately no conclusive diagnosis was attained. Unlike vaginal bleeding was worsen.
Diagnosis of AVM is generally performed radio graphically. Grayscale ultrasound findings include a nonhomogenous mass with myometrial and endometrial cystic and tubular structures. Color Doppler interrogation commonly demonstrates multidirectional, high velocity flow, and color mosaic patterns[7]. In today’s practice, AVM is easily diagnosed using color Doppler ultrasonography [8]. But, in differential diagnosis, retained products of conception and gestational trophoblastic diseases should be kept in mind because these cases may also give a hypervascular appearance with turbulent flow. BHCG levels may be helpful in diagnosis. This patient did not have elevated hCG levels. Angiography is the gold standard in the diagnosis of AVM, depicting complex vascular connections supplied by hypertrophied feeding arteries, and early drainage through enlarged, tortuous and hypertrophic veins [9].
The treatment changes depending on the age, desire for future fertility, localization, and size of the lesion. The mainstay for management of uterine AVM has been hysterectomy or the embolization of uterine arteries. However, the uterine artery embolization (UAE) remains the first choice of treatment in women at reproductive age having expectation of future fertility [10]. Timmerman et al. presented 10 cases that demonstrated uterine AVM features by color Doppler US; of these, six cases spontaneously resolved [11]. Moreover, oral contraception as well as intramuscular and subsequent oral methylergonovine maleate have been shown to be associated with regression of lesions based on US (12). Our patient had hormonal therapy for three months, but it did not decrease her vaginal bleeding.Due to our patient had heavly bleeding, we preferred UAE, but it failed. Some cases may require repeat embolisation [12]. In our patient, she did not accept repeat embolization. Based on the literature search, there are no definitivetreatment guidelines for patients who fail initial embolization. Further, there have been no studies completed comparing the effectiveness of repeat embolization versus medical therapy versus hysterectomy for persistent bleeding after initial embolization.
4. Conclusion
Uterine AVM are rare and dangerous clinical entities; their management is complicated and necessitates a high level of suspicion. In women of childbearing age, angiografic embolization should be considered as the first treatment option and hysterectomy should be reserved for only life threatening conditions.
References
- Burro ws PE. Vascular malformations involving the female pelvis. Semin Intervent Rad iol 2008; 25(4):347-360.
- Hickey M and Fraser I. Clinical Imp licat ions of Disturbances of Uterine Vascular Morphology and Function. Baillieres Clin ObstetGynaecol. 2000; 14(6):937- 951.
- Ichikawa Y, Nakauchi T, Sato T, Oki A, Tsunoda H and Yoshikawa H. Ultrasound diagnosis of uterine arteriovenous fistula associated with placental site trophoblastic tumor. Ultrasound Obstet Gynecol 2003; 21:606-8.
- Yo ko mine D, YoshinagaM, Baba Y and et al. Successful management of uterine arteriovenous malformation by ligation of feeding artery after unsuccessful uterine artery embolization. J Obstet Gynaecol Res 2009;35(1):183-188
- Kelly SM, Belli AM and Campbell S. Arteriovenous malformat ion of the uterus associatedwithsecondarypostpartum hemorrhage. Ult rasound Obstet Gynecol 2003; 21:602-5.
- Polat P, Su ma S, Kantarcy M, Alper F and Levent A. Co lour Doppler Ultrasound in the Evaluation of Uterine Vascular Abnormalities. Radiographics. 2002; 22: 47-53.
- Kim TH and Lee HH: Presenting features of wo men with uterine arteriovenous malfo rmations. Fert il Steril 2010; 94: 2330.e7- e10.
- T. Gh i, S. Giunchi, C. Rossi and et al., “Three-dimensional power Doppler sonography in the diagnosis of arteriovenous malformation of the uterus,” Journal of Ultrasound inMedicine, vol. 24, no. 5, pp. 727-731, 2005.
- Hoffman M K, Meilstrup JW, Shackelford DP and Kaminski PF.Arteriovenous malformations of the uterus: An uncommon causeof vaginal bleeding. Obstet Gynecol Surv 1997; 52:736-40.
- S. Soeda, H. Kyozuka, S. Suzuki, S. Yasuda, Y. No mura and K. Fujimori, “Uterine artery embolization for uterine arteriovenous malfo rmation is associated with placental abnormalities in the subsequent pregnancy: two cases report,” FukushimaJournal of Medical Science, vol. 60, no. 1, pp. 86-90, 2014.
- Timmerman D, Bosch TVd and Peeraer K. Vascular Malfo rmations in the Uterus: Ultrasonographic Diagnosis and Conservative Management. Euro J Obstet Gynaecol Reprod Biol. 2000; 92:171-178.
- Grivell R, Reid K and Mellor A. Uterine Arteriovenous Malformations: A review of the Current Literature. Obstet Gynaecol Survey. 2005; 60(11):761-767.