Information
Journal Policies
Outlander of the Bladder: The Hidden Copper IUD
Ahuja M1, S Vikram2, Mehta A3, Jamal S4, Goel N3
2.Professor, Department of Surgery, School of Medical Sciences and Research, Greater Noida, India
3.Professor, Department of Obstetrics and Gynecology, School of Medical Sciences and Research, Greater Noida, India
4.Assistant Professor, Department of Obstetrics and Gynecology, School of Medical Sciences and Research,Greater Noida, India
Copyright : © 2018 . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Intrauterine contraceptive devices have been in use for many years. Although perforation of the uterus by an IUD is not uncommon (9.6 per 1000 insertions), intravesical migration with secondary stone formation is a rare condition.1, 2 We report a case of 46 year old late perimenopausal woman being treated for urinary complaints for a duration of six months which on USG turned out to be Copper T encrusted with secondary calculus formation managed successfully by cystoscopic retrieval.
IUD: Intra uterine Device, USG: Ultrasonography,Gynecology, Obstetrics
1. Introduction
Intrauterine device is a common form of LARC in use for many years owing to low cost and easy availability, especially in a developing country like India. However, IUD’s are sometimes plagued with morbid complications like perforation and migration in to the adjacent organs. Reports of intravesical migration and secondary calculi formation are few in number. Migrated intravesical IUD may presents with no symptoms to non-specific urinary complaints, lower abdominal pain and even sexual dysfunction has been reported[3]. USG is the diagnostic modality of choice, however CT scan has been employed for better localization and determining the relation of IUD with surrounding structures[4]. Due to chronic inflammation produced by IUD, the need for necessary removal on diagnosis has to be emphasized[5]. The preferred modality of management is cystoscopic removal, however open cystotomy is done in difficult and impacted cases.
2. Case Report
A 46 year old with previous four vaginal deliveries and four abortions in her late perimenopausal stage presented with six months amenorrhea and urinary complaints ranging from burning micturition to increased frequency on and off. She has been taking symptomatic treatment for her urinary complaints but due to her recurrent episodes of UTI, she came to our institute for further management. History of interval IUD insertion was elicited following her last child birth ten years ago birth which on follow up was documented as lost IUD thread.
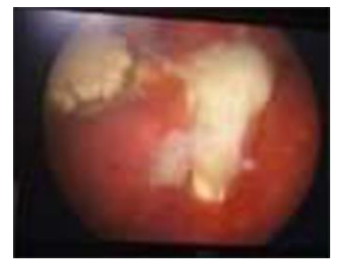
However, no further investigations were carried out in this regard. At the time of presentation there was only suprapubic tenderness on abdominal examination, per speculum examination did not reveal any IUD thread and uterus and adnexa were found normal on bimanual examination. Patient was advised ultrasound and urine for routine examination and culture sensitivity was also performed. Ultrasound revealed an echogenic linear focus on the left side in the bladder approximately 17 mm in the lumen with calcification and rest of 16 mm protruding outside the bladder lumen hence diagnosis of ectopic intravesical IUD was made. Her urine routine showed 10 RBC/hpf and culture was sterile. After urologist consultation decision for cystoscopic removal of migrated IUD was taken. She was hepatitis B positive. Under anesthesia cystoscopic removal of IUD was attempted. On cystoscopy IUD with encrusted calculi formation was seen in one of the horizontal arms and the vertical arm was seen penetrating through the bladder wall. With the help of forceps the vertical limb of Copper T was extracted successfully. No bleeding and defect was observed from the site of removal. A 14 Fr catheter was left in situ and antibiotic was given post-operatively. Catheter was removed after 7 days and patient was discharged. At 6 weeks follow visit no urinary complaints were noted.
3. Discussion
Intravesical migration with secondary calculi formation has been reported in 50% of cases of migrated IUD[6]. The pathogenesis of uterine perforation is postulated by two mechanisms: First, uterine perforation can occur at the time of insertion and gradual pressure necrosis of the uterine wall by IUD at its lead point with migration out of the uterus is the second mechanism. Insertion by unexperienced personal is one of the main factors implicated in intravesical migration of IUD. IUD produces symptoms ranging from being non symptomatic to urinary complaints and even sexual dysfunction has been documented. The time duration between migrated IUD and symptoms produced are variable and independent of the duration in the bladder. Migrace et al have reported alag of fourteen years between insertion and its symptomatology[2]. In this case the IUD was inserted 10 years back. Diagnosis is generally by USG which can be further confirmed by X-Ray. Bladder calculi are approximately 5% of all vesical calculi and are generally associated with foreign bodies[7]. The presence of bladder calculi should always prompt one to take past history of IUD insertion in females. The recommended management is cystoscopic removal. Lithotripsy is used as an adjunct to break the big calculi[8]. In cases of impacted IUD open cystotomy can also be resorted. The prolonged catherization after removal of intravesical IUD is done to prevent fistula formation and are the good practice points in their post-operative management.
4. Conclusion
A regular follow up of IUD for visible thread would help in earlier detection of misplaced IUD and prevent the complications such as intravesical migration. Proper training of paramedical staff is mandatory in developing countries to provide safe and better family planning services. History of IUD insertion should always be elicited with bladder calculi as their origin in denovo is a rarity in females.
References
- Migraci T, Handan C, Erhan Y et al. Intravesical migration of an intrauterine device detected in a pregnant woman. Can Urol Assoc J.2010; 4(5): 141-43.
- Tuncay Y, Tuncay E, Gu zin K et al. Transuterine mig ration as a complicat ion of intrauterine contraceptive device. Six Case reports. Eur J ContraceptReprod Health Care. 2004; 9: 194-200.
- Dimit ropolous K, Shripas K, karvounis G, Tziort zis V. Intrauterie device migration to urinary bladder causing sexual dysfunction. a case report. Hippokratia. 2016; 20(1): 70-2.
- TL-Hefnauy A, El Naras, Os man Y, Borace M. Urinary co mplaints of migration intrauterine device. Int Urogynecol J pelv ic floor dysfunction. 2008; 19(2): 241-45.
- Markovitch O, Klein Z, Gidoni Yet al. Extra uterine migrated IUD is surgical removal mandatory. Contraception. 2002; 66(2): 105-8.
- Hick EJ, Hernandez J, Yo rrdon R, Morey A, Aviles R, Garcia C. Bladder calculus resulting from the migrat ion of an intrauterine contraception device. J Uro l. 2004; 172(5): 1903.
- Stav K, Devyer P. Urinary b ladder stones in wo men. Obstet Gynecol Surv. 2012; 67(11): 715-25.
- Tosun M, Ceilik H, Yavuz E, Meh met B and Cetin kaya. Intravesical mig ration of an intrauterine device detected in a pregnant woman. Can Urol Assoc. 2010; 4(5): 141-43.