Information
Journal Policies
Gestational Trophoblastic Neoplasm; Case Series and Literature Review
Leila Mousavi Seresht1, Amir Hosein Jafarian2, Parvaneh Layegh3, Hamid Reza Tavakoli4, Yousef Yousefi5, Helena Azimi1, gazal ghasemi6, Yasaman Nikooiyan7, Zohreh Yousefi8
2.Assistant professor, Department of Pathology, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran.
3.Associate professor, Department of Radiology, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran.
4.Assistant professor, Department of Thoracic surgery, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran.
5.Resident Fellowship of Thoracic surgery, Department of surgery, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran.
6.Resident of Gynecology Oncology, Department of Obstetrics and Gynecology, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran.
7.Medical student, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran.
8.Professor, Department of Obstetrics and Gynecology, Fellowship of Gynecology Oncology, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran.
Copyright : © 2018 . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Objective: Appropriated management of patients with advanced of Gestational Trophoblastic Neoplasm (GTN) appear to be a great deal. This study was conducted to evaluate the value of the imaging method of fluorine-18-fluorodeoxyglucose positron emission/ computed tomography scanning (PET/CT) in treatment planning and outcome in patients with GTN and localizing of metastatic site.
Methods: A retrospective study on four patients with persistent GTN who had been studied with whole body PET/CT to detected the extension of tumor. Based on these data all our patients underwent surgery, therefor clinical impact strength of PET/CT had been analysis.
Results: In 3 of 4 cases the PET/CT had positive accordance with other anatomical and clinical impact. In one case the PET/CT not enable detected the source of viable neoplasm.
Conclusion: The additional value of the PET/CT with respect to other imaging modality; mainly is in differentiating between residual viable tumor tissue and necrosis, in discloser of chemo resistant lesion in GTN. Due to the expensive equipment despite of its value, unfortunately PET/CT, its use is limited in certain cases to detected the source of viable neoplasm.
Chemo resistance, Gestational trophoblastic tumor, FDG PET/CT Scan,Gynecology, Obstetrics
1. Introduction
GTN It is derived from abnormal proliferation of placenta and includes: the malignant transformation of hydatidiform mole, invasive mole, choriocarcinoma (CC), placental site trophoblastic tumor (PSTT).Serum human chorionic gonadotropin (βHCG) is a sensitive tumor marker in diagnosis and evaluating treatment response of GTN [1]. The diagnosis of GTN is based on plateau ,rise of serial βHCG level or unexplained persistence of βHCG level during 6 months after molar pregnancy evacuation , histopathological diagnosis of CC or PSTT; and presence of metastatic disease on imaging [2]. GTN are a reproductive age malignancy that consider curable. The goal of GTN management is timely diagnosis and accurate treatment planning based on FIGO staging and prognostic scoring [3]. However combination chemotherapy is indicated in high risk GTN. A key issue in the management of GTN is chemo resistance cases which is likelihood mortality. The important issue is finding metastasis sites with the unclear location [4]. Another recommendation have been proposed is to repeat imaging methods again for evaluation of localize metastatic site as follows: abdominal CT- scan, pelvic MRI, chest- XR and pulmonary CT- scan [5,6]. The efficacy of PET/CT as a noninvasive method for detection the active neoplastic tissue is yet has not been adequately investigated [7]. A systematic review of the relevant literature from 1996 until 2018 was performed in PubMed and MEDLINE. For the first time Hebart et all reported on the diagnostic capacity of whole body PET/CT in C. C cases in 1996 [8] in study of Shaw et al., sensitivity and specificity of PET/CT in detect of malignant focuses in PSTT cases was 90% & 80% [9]. Indeed PET/CT is combining of the detailed anatomical information obtained by CT scans with the metabolic localization of PET scans The important thing is we must keep in mind that confounding factor that interfere with interpretation of PET/CT finding most of the time lead to false positive report than false negative. The reason of false positive result interpreted can be because inflammatory and granulomatous lesion makes abnormal FDG tagged isotope uptake [10]. The factors that cause it are surgical inflammation, vascular compromise on the site of surgical retraction, surgical transposition. All of these causes could decrease the accuracy of method PET/CT. Based on this phenomenon it is often recommended that excluding other site of tumor deposit prior to metastatectomy [11,12]. There are few case reports that addressed the efficacy of PET/CT in detecting metastatic site in patients with GTN that was missed or misinterpreted on other investigational radiological modality [13] The aim of the present study is to evaluated accuracy of PET/CT scan in chemo resistance GTN, case series and literature review.
2. Material And Methods
This retrospective study was conducted on 4 chemo resistant GTN patients were referred to the Oncology Department Gynecology at academic hospital, Mashhad, Iran from April 2014 to Feb. Based on conventional evaluations method our department for all particular persistent GTN cases TVS, chest- XR, chest and abdominal CT scan, brain and pelvic MRI was happening as needed. Based on multidisciplinary consultation in the cases of isolated metastatic lesion that these methods were not effective we requested modality of PET/CT. Finally accuracy of PET/CT scan in chemo resistance GTN cases evaluated. It should be noted that all patients received Inform consent conscientious written.
3. Cases Report
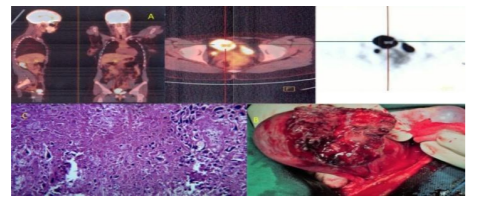
A 27-year-old woman MG2 post-molar refractory GTN,despite second line chemotherapy(EMA-EP) with persistently elevated hCG serum levels is introduced .all our conventional evaluations method above mention Could not be effective. Therefor PET/CT requisite revealed a hyper metabolic lesion in about 35 mm in the anterolateral of the uterus that seems to invade to endometrium .The patient underwent surgery and a necrotic rupture mass in the fondues of uterine was detected. Based on fertility sparing surgery, wedge resection with free margin of the lesion was obtained. Histological examination confirmed pathology of choriocarcinoma (Figure1).
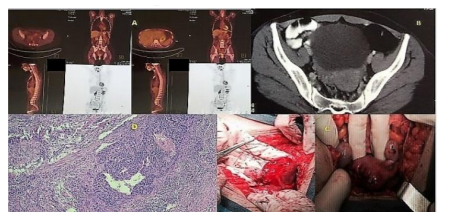
A 25 year-old NG, GTN patient who was treated with (EMA-CO) chemotherapy regimen she had history 7 courses chemotherapy but after that duo to low level quiescent GTN (hCG 120 (mIU/ml) was investigated and discussed at the tumor board meeting. Based on all our conventional evaluations method were not effective therefore PET/CT scan recommended. But because of this modality nothing was found any evidence of occult metastasis, the patient observed with monthly βHCG measurement. After 2 months the βHCG re-elevated to 6000 mIU/ml abdominal CT scan showed a 1.5 cm mass with irregular border foci in left adnexa. In Laparotomy we observed a 3×3 cm mass in right cornea of uterus. Pathologic examination of frozen section showed metastases of choriocarcinoma. Therefore due to fertility sparing surgery wedge resection of cornea of uterine with free margin was performed (Figure2).
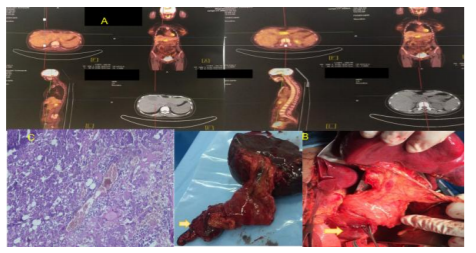
A 35 year-old MG woman with diagnosis of PSTT in abdominal hysterectomy specimen and chemo resistant combined chemotherapy with EMA-CO and EMA-EP regimen was reported . Regarding to evaluation of increased of βHCG level after all investigation; PET/CT scan was requested. Only one hyper metabolic lesion in about 4 cm in lessor sac in favor of metastasis was detected. Laparotomy showed pancreas head mass adjacent to spleen so, partial pancreatectomy with splenectomy was obtained. The pathology confirmed the PSTT metastasis in all of them (Figure3).
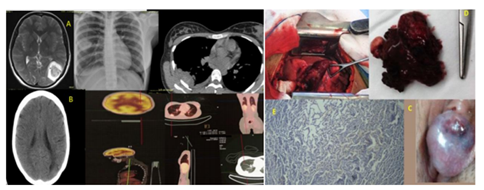
A 20 year-old MG woman with diagnosis of stage IV of GTN (lung, brain) metastasis was referred .despite cranial radiotherapy and 5 cycle of chemotherapy (EMA-CO) regimen, βHCG titer did not reach to normal level. EMA-EP regimen chemotherapy did not respond, therefor traditional our center imaging diagnostic modality were used. However they were able to show lung lesion and smaller size brain lesion, but these findings were not exactly distinguish. so PET/CT was demanded .this modality shown that lung lesion ;abnormal hyper metabolic foci (SUV max 2.9) thoracotomy and wedge resection of this lesion was performed , report of histology confirm metastasis choriocarcinoma ( Figure4).
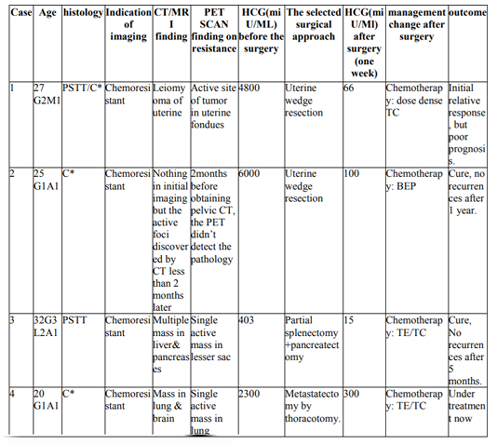
Detailed clinical information, imaging studies, histopathological reports and outcomes are shown in (Table1).
4. Discussion
In our study in 3 of 4 chemo resistant GTN cases PET/CT had positive accordance with other anatomical, histological finding. Generally GTN cases are curable even in the presence of disseminated metastasis. However some of the GTN patients become persistent or recurrence especially in pathology of; which is a critical problem. Most studies believe that emphasis on usefulness of mapping metastatic site to detect the source of viable-resistance tumor and requisiteness of surgery in patient with persistent or rise βHCG titer after chemotherapy [14,15]. Serum βHCG titer is an excellent tumor marker for GTN but it couldn’t suggest the location of tumor. Diagnose of localization metastatic site is a crucial point in treatment of GTN cases. There are limited data on the best management in chemo refractory patients [16]. It is important to note the limitation of the traditional imaging study in differentiation neoplastic lesions from necrotic tissue due to chemo-radiotherapy effect [17]. Although there are some problems with PET/CT. According to recommendations that have been made in cases where the method PET/CT is intended it should be at least 3 & 8 weeks later of chemotherapy and radiotherapy this m modality is to be used [18]. However in study of Chang et al., 7 days is sufficient for this interval for cases under chemotherapy [19]. There are some confounding factor that interfere with interpretation of PET/CT: inflammatory and granulomatous lesion lead to false positive report however radiotherapy and chemotherapy could lead to abnormal FDG uptake[20]. Bone marrow suppression as the chemotherapy side effect might be treated with GCSF, which lead to disseminated FDG uptake in bone marrow and spleen [21]. In the other hand in an article about PET scan pitfall recommended 10-20 days interval between traditional and long acting GCSF administration and PET scan [22].The PET/CT is not much used in malignancy with slow growth malignant cell, which is one of the main reason for false negative reports. Small size tumor (less than 5-7 mm in diameter) couldn’t identified by the PET scan [23]. But conversely, Grisaru et al., in their study on 55 patients showed that accuracy this method for detecting < 1cm lymph node [24]. By the way this study could be useful in GTN which has high potency of prompt progression and it is expected that explain the false negative reports in PSTT cases. One of the preparation criteria before administration of intravenous FDG is patient blood sugar ,which must be less than 140 mg/dl, the hyperglycemia statues is a confounding factor that could easily resolved by consumption 24 hours low carbohydrate diet which followed with 4-6 hour of complete fasting (except water) the day before the imaging evaluation [25]. In articles of Pawar et al., on 56 cases of gynecologic cancer including GTN strong emphasis on using this method for treatment decisions is [26]. The Studies that focus solely on chemoresistant GTN cases are very limited and most are retrospective. (Table2). In general, in all oncology cases sensitivity and specificity of PET/CT in comparing with either conventional imaging modality for detecting malignant tumor location is 90% & 80%[27]. In our study this rate was 75%.
In fact the appropriate treatment and close monitoring in GTN patients is corner stone of treatment. In addition accurate assessment occult viable tumor is crucial. Based on this study PET/ CT is very value in detection of active tumor in metastatic site.
5. Conclusion
With PET/CT there is a lot of diagnostic accuracy in detecting of metastatic disease in chemo resistant GTN cases . The additional benefit of the PET/CT with respect to other imaging modality is differentiating between residual viable tumor tissue and necrosis. However PET/CT has a valuable ability for PSTT patient who are relatively insensitive to chemotherapy and might have distant metastasis that need radical surgery as the mainstay of management.
References
- Mapelli P, Mangili G, Picchio M, Gentile C, Rabaiotti E, Giorgione V, Spinapolice EG, Gianolli L, Messa C, Candiani M. Role of 18F-FDG PET in the management of gestational trophoblastic neoplasia. European journal of nuclear medicine and molecular imaging. 2013 Apr 1; 40(4):505-13.
- Dhanda S, Ramani S, Thakur M. Gestational trophoblastic disease: a multimodality imaging approach with impact on diagnosis and management. Radiology research and practice. 2014; 2014. Raghu Vikram and Revathy B. Iyer
- Nieves L, Hoffman J, Allen G, Currie J, Sorosky JI. Placental-site trophoblastic tumor with PET scan-detected surgically treated lung metastasis. International journal of clinical oncology. 2008 Jun 1;13(3):263-5
- Çerçi SS, Erdemoglu E, Bozkurt KK, Yalcn Y, Erdemoglu E. Placental-site trophoblastic tumor and fluorine-18-fluorodeoxyglucose positron emission tomography/computed tomography. Hell. J. Nucl. Med... 2015 Sep 1; 18(3):264-7.
- Biscaro A, Braga A, Berkowitz RS. Diagnosis, classification and treatment of gestational trophoblastic neoplasia. Revista Brasileira de Ginecologia e Obstetrícia. 2015 Jan;37(1):42-51.
- Zaheer S, Osmany S, Lai HK, Eng DN. Usefulness of F-18 fluorodeoxyglucose positron emission tomography/computed tomography in a case of choriocarcinoma presenting as pulmonary embolism. Clinical nuclear medicine. 2009 Jun;34(6):343-5.
- Kelly T, Alvis C, Abedalthagafi M, Barnes W. Diagnostic evaluation of metastatic placental site trophoblastic tumor. Obstetrics & Gynecology. 2009 Aug 1;114(2, Part 2):465-8.
- Raghu Vikram and Revathy B. Iyer PET/CT imaging in the diagnosis, staging, and follow-up of colorectal cancer Cancer Imaging. 2008; 8(Spec Iss A): S46–S51
- Shaw SW, Wang CW, Ma SY, Ng KK, Chang TC. Exclusion of lung metastases in placental site trophoblastic tumor using [18F] fluorodeoxyglucose positron emission tomography: A case report. Gynecologic oncology. 2005 Oct 1; 99(1):239-42. 9.
- Numnum TM, Leath CA, Straughn JM, Conner MG, Barnes MN. Occult choriocarcinoma discovered by positron emission tomography/computed tomography imaging following a successful pregnancy. Gynecologic oncology. 2005 May 1; 97(2):713-5.
- Ngu SF, Chan KK. Management of chemoresistant and quiescent gestational trophoblastic disease. Current obstetrics and gynecology reports. 2014 Mar 1; 3(1):84-90. 12.
- Yang J, Xiang Y, Wan X, Yang X. The prognosis of gestational trophoblastic neoplasia patient with residual lung tumor after completing treatment. Gynecologic oncology. 2006 Nov 1; 103(2):479-82.
- Rojas-Espaillat L, Houck KL, Hernandez E, Berkowitz RS. Fertility-sparing surgery for persistent gestational trophoblastic neoplasia in the myometrium: a case report. The Journal of reproductive medicine. 2007 May; 52(5):431-4.
- O'donnell JS, Rini J, Chusid J, Shah RD. Abnormal Uptake on PET/CT: Imitators of Malignancy in Thoracic Imaging. Contemporary Diagnostic Radiology. 2011 May 31;34(11):1-6
- Ulaner GA, Lyall A. Identifying and distinguishingtreatmenteffectsand complications from malignancy at FDG PET/CT. Radiographics. 2013 Oct 1;33(6):1817-34
- Gould MK, Maclean CC, Kuschner WG, Rydzak CE, Owens DK. Accuracy of positron emission tomography for diagnosis of pulmonary nodules and mass lesions: a meta-analysis. Jama. 2001 Feb 21; 285(7):914-24.
- Roberts PF, Follette DM, von Haag D, Park JA, Valk PE, Pounds TR, Hopkins DM. Factors associated with false-positive staging of lung cancer by positron emission tomography. The Annals of thoracic surgery. 2000 Oct 1;70(4):1154-9.
- Sironi S, Picchio M, Mangili G, Garavaglia E, Zangheri B, Messa C, Voci C, Taccagni GL, DelMaschioA,FazioF.[18F] fluorodeoxyglucose positron emission tomography as a useful indicator of metastatic gestational trophoblastic tumor: preliminary results in three patients. Gynecologic oncology. 2003 Oct 1;91(1):226-30.
- Chang TC, Yen TC, Li YT, Wu YC, Chang YC, Ng KK, Jung SM, Wu TI, Lai CH. The role of 18 F-fluorodeoxyglucose positron emission tomography in gestational trophoblastic tumours: a pilot study. European journal of nuclear medicine and molecular imaging. 2006 Feb 1; 33(2):156-63.
- Cypess AM, Lehman S, Williams G, Tal I, Rodman D, Goldfine AB, Kuo FC, Palmer EL, Tseng YH, Doria A, Kolodny GM. Identification and importance of brown adipose tissue in adult humans. New England Journal of Medicine. 2009 Apr 9; 360(15):1509-17.
- Blankenstein TN, Eljamel S, Brush J. Pitfalls in positron emission tomography. BMJ: British Medical Journal (Online). 2017 Sep 14;358
- Mangili G, Bergamini A, Giorgione V, Picchio M, Petrone M, Mapelli P, Rabaiotti E, Incerti E, Candiani M. [¹⁸F] fluorodeoxyglucose positron emission tomography/computed tomography and trophoblastic disease: the gynecologist perspective. The quarterly journal of nuclear medicine and molecular imaging: official publication of the Italian Association of NuclearMedicine(AIMN)[and]the International Association of Radiopharmacology (IAR),[and] Section of the Society of... 2016 Jun;60(2):103-16
- Dhanda S, Ramani S, Thakur M. Gestational trophoblastic disease: a multimodality imaging approach with impact on diagnosis and management. Radiology research and practice. 2014;2014.
- Grisaru D, Almog B, Levine C, Metser U, Fishman A, Lerman H, Lessing JB, Even-Sapir E. The diagnostic accuracy of 18F-fluorodeoxyglucose PET/CT in patients with gynecological malignancies. Gynecologic oncology. 2004 Sep 1; 94(3):680-4.
- Dhillon T, Palmieri , Sebire NJ, Lindsay I, Newlands ES, Schmid P, Savage PM, Frank J, Seckl MJ. Value of whole body 18FDG-PET to identify the active site of gestational trophoblastic neoplasia. The Journal of reproductive medicine. 2006 Nov;51(11):879-87.
- Pawar AA, Patil DB, Patel S, Mankad M, Dave P. Role of PET–CT Scan in Gynaeconcology. The Journal of Obstetrics and Gynecology of India. 2016 Oct
- Powles T, Savage P, Short D, Young A, Pappin C, Seckl MJ. Residual lung lesions after completion of chemotherapy for gestational trophoblastic neoplasia: should we operate?. British journal of cancer. 2006 Jan 16; 94(1):51.