Information
Journal Policies
Multiple Repeat Cesarean Deliveries: Is Perinatal Morbidity Really Differs?
Alaa Masood1*, Ragab Dawood1, El-Sayed El-Shamy1,2, Hassan Badr3
2.Department of Obstetrics and Gynecology, King Abdul-Aziz Airbase hospital, Dhuran, Saudi Arabia
3.Department of Pediatrics, Faculty of Medicine, Menoufia University, Shibin El-Kom City, Menoufia governorate, Egypt
Copyright : © 2018 . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Objective: To assess prospectively maternal and perinatal outcome with multiple repeat cesarean deliveries (CDs) with special emphasis on the perinatal morbidity.
Methods: A prospective observational study included a total of 5750 patients with prior CD who were divided into two groups; first group with previous 1-2 CDs (n=4122) and a second group with previous ≥ 3 CDs (n=1628). Patients were followed throughout pregnancy, delivery and puerperium to record maternal and perinatal outcome.
Results: Patients with ≥ 3 CDs exhibited a higher rates of longer operative time (46.6% vs 22.1%), severe intra-abdominal adhesions (50% vs 9.66%), urinary injuries (2.21% vs 1.16%), blood transfusion (10.3% vs 0.58%), peripartum hysterectomy (13.02% vs 0.19%), the need for re-operation (2.83% vs 0.15%), longer hospital stay (14.62% vs 1.1%) , admissions to HDU/ICU (6.02% vs 0.29%) compared to those in the first group respectively (p< 0.001). Poorer perinatal outcome in terms of higher rates of prematurity (4.18% vs 2.13%), low birth weight (6.27% vs 2.28%), low Apgar scores at 5 minutes (19.29% vs 6.98%), admission to NICU (7.13% vs 2.62%), respiratory morbidity (2.33% vs 0.24%), early onset neonatal sepsis (1.97% vs 0.15%), poor suckling (2.83% vs 0.29%) and longer stay at NICU (6.88% vs 2.52%) among patients with ≥3 CDs compared to those with one or two CDs respectively (p< 0.001).
Conclusion: Although multiple repeat cesarean deliveries was not associated with increased perinatal mortality, yet associated with appreciable increase in short term perinatal morbidity. Long term follow up studies of the babies are also warranted.
Multiple repeat cesarean deliveries, maternal outcome, perinatal outcome,Gynecology, Obstetrics
1. Introduction
Cesarean delivery (CD) rate has increased steadily over the past two decades and constitutes a public health problem in terms of the economic burden and the possible maternal and perinatal complications [1].
Most of studies in the literature have reported the effects of multiple repeat CD on maternal morbidity in terms of risks of anesthesia, blood transfusion, abnormal placenta invasion, bladder or bowel injury, and intra-abdominal adhesions [2-6], with little attention paid to the possible short and long-term perinatal complication that may arise from multiple repeat CDs.
The aim of this study was to assess prospectively both the maternal and perinatal outcome with multiple repeat CDs with special emphasis on the perinatal morbidity.
2. Materials And Methods
This prospective 6-year observational study was conducted at the department of Obstetrics and Gynecology in collaboration with the Pediatrics department at Menoufia University hospital during the period between the beginnings of March 2012 and March 2018 which is the date of the last day of puerperium of the last included patient.
The Ethical committee for medical research at Menoufia Faculty of Medicine reviewed and formally approved the study protocol (ethical clearance letter number 267 G/2012); before commencement of the study. All participants signed an informed consent form after thorough explanation of the study objectives. The reported investigations were carried out in accordance with the principles of the Declaration of Helsinki as revised in 2000.
A total of 5874 out of 6056 patients with history of previous CD who attended our antenatal care clinic or referred from other district hospitals during the first trimester were included after thorough history taking, physical examination and antenatal investigations. Gestational age was recorded according to the last menstrual period when known to be confirmed by obstetric ultrasound between 6-12 weeks.
Patients with multiple pregnancy, congenial fetal malformations, those opted for trial of labour after cersarean (TOLAC); were excluded from the study.
Included patients underwent regular antenatal care visits at the outpatient clinic with average 6-10 visits throughout pregnancy while those with known medical disorders attended more frequent visits until delivery with follow up of the mother and the newborn till the end of the puerperium.
Included patients were divided into two groups based on the number of previous CDs:
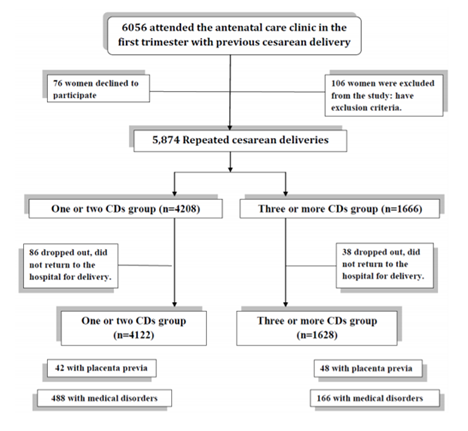
Group 1(n=4208): Included patients with previous one or two CD. 86 cases were dropped out and 4122 completed the study; previous one CD (n=2816) and two CDs (n=1306). Placenta previa complicates 42 cases while medical disorders were encountered among 488 cases.
Group 2 (n=1666): Included patients with previous three or more CDs. 38 cases dropped out and 1628 completed the study; previous three CDs (n=1304), four or more CDs (n=324). Placenta previa complicates 48 cases while medical disorders were encountered among 166 cases (Figure 1: The flow diagram).
This differentiation into two groups was primarily based on the results of a previous systematic review which confirmed the significantly increased maternal morbidity among patients with ≥ three CDs [5].
Elective repeat CD was scheduled at 38-40 weeks gestation according to our hospital policy. Patients developed spontaneous onset of labour underwent CD with senior registrar or consultant on duty according to the clinical scenario of each case.
Maternal Outcome: Miscarriage (interruption or termination of pregnancy before 20 weeks), perioperative details (duration of CD, the type of adhesions, injury to nearby structures, blood transfusion and peripartum hysterectomy), the need for re-operation (secondary to bleeding or organ injury), wound complications (dehiscence or infection), venous thromboembolism, admission to high dependency or intensive care unit, prolonged hospital stay (>4 days) and maternal mortality. Items of maternal morbidity were further described according to the presence or absence of placenta previa/accreta.
Perinatal Outcome: prematurity (delivery before completed 37 weeks irrespective of the indication of delivery), low birth weight (< 2000 gm), intrauterine fetal demise, low Apgar scores (< 7 at 5 minutes), admission to neonatal intensive care unit (NICU), respiratory morbidity (respiratory distress syndrome or transient tachypnea of the newborn), early onset neonatal sepsis, poor suckling, longer stay at NICU (>4 days) and neonatal mortality (death of the neonate during the first 4 weeks after birth). Items of perinatal morbidity were further described according to the presence or absence of associated medical disorders.
3. Statistical Analysis
Data was analyzed with an IBM computer using the SPSS 22 statistical software package (SPSS Inc., Chicago, IL). Student's t test was used for comparing means of two normally distributed continuous Variables while Mann-Whitney test was used for non-parametric variables. Chi square and Fischer’s exact tests were used for comparison of categorical variables. P value less than 0.05 was statistically significant while P value less than 0.001 was considered statistically highly significant
4. Results
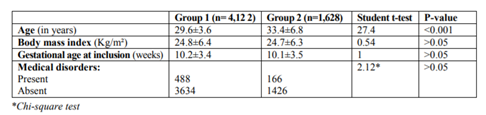
There was no significant difference between the two groups regarding maternal body mass index, gestational age at inclusion and the presence of underlying medical disorders complicating pregnancy (p< 0.05) with patients in the second group being significantly older (p< 0.001) as depicted in table (1).
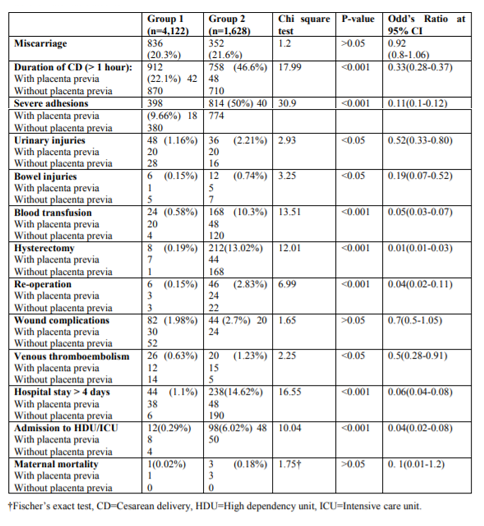
Patients in the second group exhibited higher rates of longer operative time of CD more than one hour (46.6% vs 22.1%), severe intra-abdominal adhesions (50% vs 9.66%), urinary injuries (2.21% vs 1.16%), blood transfusion (10.3% vs 0.58%), peripartum hysterectomy (13.02% vs 0.19%), the need for re-operation (2.83% vs 0.15%), longer hospital stay (14.62% vs 1.1%) , admissions to HDU/ICU (6.02% vs 0.29%) compared to those in the first group respectively as revealed in table (2).
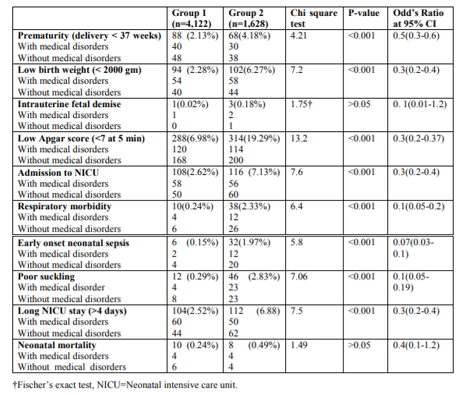
Poorer perinatal outcome in terms of higher rates of prematurity (4.18% vs 2.13%), low birth weight (6.27% vs 2.28%), low Apgar scores at 5 minutes (19.29% vs 6.98%), admission to NICU (7.13% vs 2.62%), respiratory morbidity (2.33% vs 0.24%), early onset neonatal sepsis (1.97% vs 0.15%), poor suckling (2.83% vs 0.29%) and longer stay at NICU (6.88% vs 2.52%) among patients with ≥3 CDs compared to those with one or two CDs respectively as seen in table (3).
5. Discussion
Patients with ≥ three CDs exhibited higher rates of longer operative time of CD more than one hour (46.6% vs 22.1%), severe intra-abdominal adhesions (50% vs 9.66%), urinary injuries (2.21% vs 1.16%), blood transfusion (10.3% vs 0.58%), peripartum hysterectomy (13.02% vs 0.19%), the need for re-operation (2.83% vs 0.15%), longer hospital stay (14.62% vs 1.1%) , admissions to HDU/ICU (6.02% vs 0.29%) compared to those with prior one or two CDs respectively.
Earlier studies reported increased rates of placenta previa, placenta accreta and peripartum hysterectomy with each successive CD [7]. Hysterectomy was required in 0.65% after the 1st , 0.42% after the 2nd , 0.90% after the 3rd , 2.41% after the 4th , 3.49% after the 5th , and 8.99% after the 6th or more CDs among cohort of 30,132 women who had CD without labour in 19 academic centers over 4 years [8].
Even one prior CD was sufficient to increase the risk of an adverse maternal outcome (with a composite of transfusion, hysterectomy, operative injury, coagulopathy, venous thromboembolism, pulmonary edema, or death) from 15% to 23% in another cohort of 868 women [9].
The number of cases with placenta previa was 42/4122 (1.02%) in patients with previous one or two CD compared to 48/1628 (2.94%) patients with≥3 CDs in this series which was in accordance to the figures previously described in an earlier systematic review [5] with reported increase in incidence of placenta previa from 10/1000 deliveries with one previous CD to 28/1000 with ≥3 CD.
A retrospective case-control study of 144 pregnant women with ≥4 CDs was compared with a control group of 288 women having 2-3 CDs reported longer operating times (p = 0.0001) due to severe adhesions (p = 0.0005), with increased blood loss and blood transfusion (p = 0.0001) in the study group [10].
A recent retrospective study included a total of 1,506 patients (444 patients with ≥4 previous CDs and 1062 controls with 3 previous CDs) reported higher rates of dense adhesions, requirement of pelvic drainage, duration of hospitalization and the requirement for blood transfusion in the study group [11].
In this series, multiple repeat CDs were associated with poorer perinatal outcome in terms of higher rates of prematurity (4.18% vs 2.13%), low birth weight (6.27% vs 2.28%), low Apgar scores at 5 minutes (19.29% vs 6.98%), admission to NICU (7.13% vs 2.62%), respiratory morbidity (2.33% vs 0.24%), early onset neonatal sepsis (1.97% vs 0.15%), poor suckling (2.83% vs 0.29%) and longer stay at NICU (6.88% vs 2.52%) among patients with ≥3 CDs compared to those with one or two CDs respectively.
An earlier cohort study of 56 549 prospectively recorded late-preterm and term vaginal and CDs, perinatal morbidities and mortality had a strong gestational age-related trend with the lowest incidences consistently found between 38 and 40 weeks of gestation independent of delivery mode [12].
Another prospective study that included a total of 2021 infants, 1120 born vaginally and 901 by CD, respiratory morbidity was higher only for infants delivered at ≤ 38 weeks when stratified by gestational age only. Also, respiratory morbidity was higher in infants born at ≤ 38 weeks by CD without labour compared to those with labour in addition to reduction of exclusive breastfeeding at discharge [13].
A recent cohort study of 5071 deliveries without labour pains CDs and 731 with labour-onset CDs, a two- to three-fold increased risk of newborn septicemia or antibiotic treatment at early term with higher rates of maternal endometritis were reported in patients with labour-onset CDs [14].
Also, a recent retrospective study included a total of 1,506 patients reported significant reduction in the umbilical artery pH results in patients with four or more CDs[11].
A recent cohort study compared early term elective CD (at 37 weeks) to late term CD (at 39 weeks) reported higher rate of 5-minute Apgar score less than 7 at planned early CD (0.4 vs. 6.4%; p < 0.001) [15].
The rate of perinatal mortality was similar between the two groups in the current study and did not increase significantly with increasing number of prior CDs which is consistent with previous studies [9-11,15].
A recent record-linkage study included 40,145 patients with history of prior CD at term who delivered via elective CD (n = 17,919), unscheduled repeat CD (n = 8,847) with those following TOLAC (n = 13,379), reported higher rate of hospitalization with asthma among children delivered via CD compared to those delivered vaginally [16].
The study design in addition to the large number of included patients constitutes the main strength and the meaningful findings of the current study.
Inability to stratify the confounding factors affecting the perinatal morbidity as well as non inclusion of vaginal delivery group as control in this series was unintended limitations.
Future research should focus on the implementation of adverse short term perinatal outcome to patients with multiple repeat CDs as a part of their preconception counseling.
6. Conclusion
Although multiple repeat cesarean deliveries was not associated with increased perinatal mortality, yet associated with appreciable increase in short term perinatal morbidity. Long term follow up studies of the babies are also warranted.
Acknowledgements
The authors would like to acknowledge the contribution of the residents and nursing staff of the labor and delivery ward of Menoufia University Hospital.
References
- Huang X, Lei J, Tan H, et al. Cesarean delivery for first pregnancy and neonatal morbidity and mortality in second pregnancy. Eur J Obstet Gynecol Reprod Biol. 2011; 158(2): 204–208.
- Qublan HS, Tahat Y: Multiple cesarean section. The impact on maternal and fetal outcome. Saudi Med J, 2006; 27(2): 210–14.
- Bates GW Jr, Shomento S: Adhesion prevention in patients with multiple cesarean deliveries. Am J Obstet Gynecol, 2011; 205(6 Suppl.): S19–24.
- Ben-Ami I, Schneider D, Svirsky R et al: Safety of late second-trimester pregnancy termination by laminaria dilatation and evacuation in patients with previous multiple cesarean sections. Am J Obstet Gynecol, 2009; 201(2): 154.e1–5.
- Marshall NE, Fu R, Guise JM: Impact of multiple cesarean deliveries on maternal morbidity: a systematic review. Am J Obstet Gynecol, 2011; 205(3): 262.e1–8.
- Gregory KD, Jackson S, Korst L, et al. Cesarean versus vaginal delivery: whose risks? Whose benefits? Am J Perinatol. 2012; 29(1): 7–18.
- Makoha FW, Felimban HM, Fathuddien MA, Roomi F, Ghabra T. Multiple cesarean section morbidity. Int J Gynaecol Obstet. 2004; 87(3):227-32.
- Silver RM, Landon MB, Rouse DJ et al. Maternal morbidity associated with multiple repeat cesarean deliveries. Obstet Gynecol. 2006; 107(6):1226-32.
- Grobman WA, Gersnoviez R, Landon MB et al. Pregnancy outcomes for women with placenta previa in relation to the number of prior cesarean deliveries. Obstet Gynecol. 2007; 110(6):1249-55.
- Gasim T, Al Jama FE, Rahman MS, Rahman J. Multiple repeat cesarean sections: operative difficulties, maternal complications and outcome. J Reprod Med. 2013; 58 (7-8):312-8.
- Çintesun E, AI RA. The effect of increased number of cesarean on maternal and fetal outcomes. Ginekol Pol. 2017; 88(11):613-619.
- De Luca R, Boulvain M, Irion O, Berner M, Pfister RE. Incidence of early neonatal mortality and morbidity after late-preterm and term cesarean delivery. Pediatrics. 2009; 123(6):e1064-71.
- Ceriani Cernadas JM, Mariani G, Pardo A et al. Cesarean delivery at term in low risk pregnancies: effects on neonatal morbidity. Arch Argent Pediatr. 2010; 108(1):17-23.
- Glavind J,2, Milidou I, Uldbjerg N, Maimburg R, Henriksen TB. Neonatal morbidity after spontaneous labor onset prior to intended cesarean delivery at term: a cohort study. Acta Obstet Gynecol Scand. 2017; 96(4):479-486.
- Miller ES, Nielsen C, Zafman KB, Fox NS. Optimal Timing of Delivery in Women with Higher Order Cesareans: A Cohort Study. Am J Perinatol. 2018 Apr 16. doi: 10.1055/s-0038- 1641587. [Epub a head of print].
- Black M, Bhattacharya S, Philip S, Norman JE, McLernon DJ. Planned Repeat Cesarean Section at Term and Adverse Childhood Health Outcomes: A Record-Linkage Study. PLoS Med. 2016;13(3):e1001973.