Information
Journal Policies
The Prevalence of Du Phenotype in Rhesus D Negative Patients Attending the Prepregnancy Class in Lagos
G.O. Ajayi
Copyright : © 2017 . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Objective: To determine the prevalence of Du Phenotype in Rhesus D negative Patients attending the Prepregnancy class in Lagos.
Setting: A Prenatal Diagnosis and Therapy Centre of a Tertiary Hospital in Lagos
Design: A Retrospective Study.
Methods and Materials: Samples from 1345 men and women who attended the pre-pregnancy class from January 2003 to December 2009 were analyzed prospectively with respect to their ABO and Rhesus group System. All n =114 Rhesus D negative patients had elaborate indirect antiglobulin test to detect the presence of Du Phenotype for statistical analysis.
Results: The commonest ABO group System was group O. The prevalence of Rhesus D Positive and Rhesus D Negative was 91.53% and 8.47% respectively.
Du Phenotype was detected in only 5.05% (5) of the 99 Rhesus Negative Female Patients
Conclusion: Preconceptional identification of Du carrier women has advantages of eliminating the task of looking for Rh- D Negative blood if such a female needs transfusion and also eliminates the need for the use of costly prophylactic IgG anti-D Immunoglobulin injection post-delivery of a Rhesus D-positive fetus. Preconceptional DuTesting is necessary in our environment where RhD Negative blood is scarce and IgG anti-D Immunoglobulin injections are expensive.
ABO Blood group, Rh D Negative, Du phenotype, Prepregnancy class, Prevalence,Gynecology,Obstetrics
1. Introduction
The Rhesus (Rh) blood group System is the most complex of all erythrocytes blood group System, with more than 40 different anti-helical antigens (two antigens controlled by a pair of allelic genes. The major allelic pairs are C/c and E/e but the antithetical antigens expressed, as the small d has never been demonstrated. The Rhesus genes reside on chromosome with the D gene acting as an autosomal dominant (Mary 1989 [1]).
The use of the terms Rh Positive and Rh Negative refer only to the presence or absence of the D antigen. Routine testing for the Rhesus System in our environment involves only the use of monoclonal and or polyclonal anti-D Sera. In developed countries reagent antigens are available for D, C, c, E and e antigens that are used to resolve antibody problems or conduct family studies.
According to Mary (1989[1]) the phenotype is not considered to be an antigen separate from the D antigen and can arise in three [3] different forms. Suppression of D-Antigen expression because of genetic interaction, inheritance of a gene that codes for less D Antigens (weak D) and absence of a portion of the total material that comprises the D antigens (D mosaic or D variant). These weak D and the D variant antigens can give a discrepant result in D grouping serology (Szymanski 1989 [2]). Accurate determination of the D antigen Status in before and during pregnancy is very important in women because of the immunogenicity of the D antigen. (Walters1995[3]). If an Rh (D) negative mother is erroneously grouped as Rh (D) positive, they carry the risk of being transfused with Rh (D) positive blood that may result in sensitization and can cause haemolytic disease of the newborn in subsequent pregnancies (Szymanski et al 1989 [2]).
Such pregnant women could also be receiving prophylactic IgG anti- D immunoglobulin and other serological screening for artificial antibodies (Marcela and Anatole 1999[4]). The prevalence rate between 90-99% and 1-9.5% have been reported respectively for Rh (D) positivity and Rh (D) negativity in previous reports from Nigeria (Nwauche et al 2004 [5], Falusi et al 2000 [6], Odunaiya 1976 [7], Worlledge et al 1974 [8], Issit et al 1998 [9], Ajayi 2006 [10].
In our environment the information on the prevalence of Du Phenotype among prepregnant and pregnant women is very limited. Based on this, the study was undertaken to determine the prevalence of Rhesus D negative and the Du phenotype among population attending the pregnancy class at Prenatal Diagnosis and Therapy Centre, College of Medicine, University of Lagos, Lagos, Nigeria, and to see whether this elaborate IAT (Indirect Antiglobulin Test) to detect Du Phenotype should be routine or not.
2. Methods And Materials
Between January 2003 and December 2006, a total of n= 1345 Patients attending prepregnancy class at the Prenatal Diagnosis and Therapy Centre, College of Medicine, University of Lagos, Lagos Nigeria venous blood were collected after inform consent taken. Samples were allowed to clot and then centrifuged at 3400 rev/ min for 15minutes. The Sera were separated and 2% suspension of the cells were made in Saline for immediate analysis. All the samples were analyzed with 2-4hours of collection. The ABO and Rh (D) group were performed at the same time according to Dacic and Lewis [11] with appropriate controls. Anti-A and Anti-B monoclonal reagent and blended monoclonal anti-A, B reagent (BiotecLaboratory UIV) were used for the cell grouping and standard A, B and O cells locally prepared from pooled cells were used for the serum grouping. Anti-D IgM/IgG blend, KB-DB-10 and BG-DB-71 (BiotecHomsard Diagnostics, UK) capable of detecting weak forms of D antigens were used for the Rh (D) grouping. All cells that did not react with saline Anti-D were tested for the Du antigen as follows: Label a 10×25mm (Khan) tube with appropriate name or number, put few drops of blood (that did not agglutinate with saline Anti-D and suspend with saline almost to brim of the tube). Stain for about 60seconds decant supernatant, re-suspend cells in tube and add equal volume of incomplete Anti-D. Incubate at 37oc for 30minutes. Wash cells 4× in saline, making sure to resuspend cells in residual drop of saline between washings. Decant fully at the last wash. Put a drop of Anti human globulin (AHG) on clean tile. With the aid of a clean Pasture pipette, transfer 1 drop of washed cells on AHG on tile. Mix with wooden or plastic applicator stick and start rocking the tile forth and back for about 5minutes. Observe or check for agglutination. (RESULT: Agglutination present – Du positive, Agglutination absent - Du negative).Negative and Auto control were also set up concurrently for the Du typing. To all tubes that were negative 1 drop of 100mlscontrol cells was added to verify the activity of AHG anti sera. 100mlscontrol cells must agglutinate in all tubes that were initially negative. Data were statiscally analyzed using SPSS software version 11.0.
3. Results
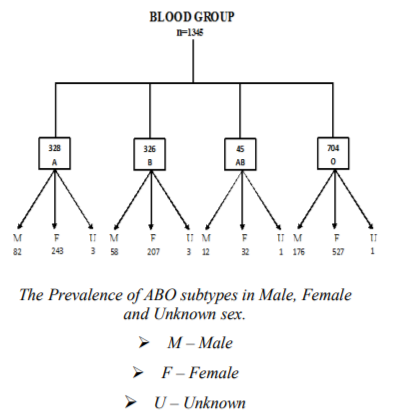
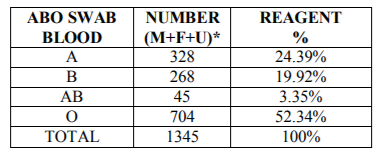
A total of n= 1345 samples from n= 1345 patients were analyzed. The mean age of the patients was 28.6 ±6.3 years SD. The commonest ABO blood group was O followed by A, B and AB being the least (Figure1, Table1).
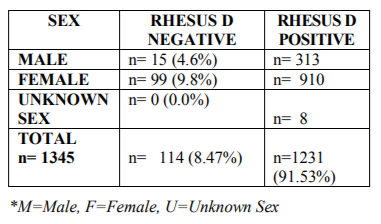
The prevalence of Rh (D) positive and Rh (D) negative blood group was male and females 95.4% / 4.6% and 90.2% / 9.8% respectively (Table 2).Out of a total of n= 99 female patients, only 5.05% (5) were Du positive.
4. Discussion
Our overall result from n=1345 discussed the prevalence rate of 91.53% and 8.47% respectively for Rhesus D positive and Rhesus D negative also confirm other studies from Nigeria (Nwauche et al 2004 [5], Falusi et al 2000 [6], Odunaiya et al 1976 [7]Kagu et al 2005[12]). The result is also similar to earlier results among black Americans who has Rhesus D negative prevalence rate of 7 to 8% (Issit et al 1998 [9], Ajayi 2006 [10], Joseph et al 1991 [13]) Mark et al 1993 [14] Genetic and racial variation may explain the findings. The prevalence rate of 4.39% observed for Du Antigen of Du phenotype is very lowswabin about 15% of the samples, the use of protein typing reagent for Rhesus D grouping and Du testing couple with strict adherence to manufacturing instructions could reduce enough of mistyping Rhesus D negative mothers as Rhesus D negative, Du positive by the Du test. The clinical implication of not detecting Du phenotype in Rhesus D-negative pregnant women is that it will lead to unnecessary use of anti-D-immunoglobulin. The cost of which is beyond the reach of most of the pregnant mother in our study confirms the results of Kaguetal 2005[12] who had 3.84%, which is much higher than the prevalence rate of 9.5% reports from Port Harcourt by Nwauche et al 2004 [5], geographical location and methodology may be responsible for the differences. Marcela et al 1999[4] has shown that although Du tests do not detect all examples apart from this, misclassifying Du positive women as D negative will cause great anxiety due to hardship associated with getting D negative blood in case of the need for blood transfusion. There is therefore the need for a large collaborating study to determine the prevalence of the Du phenotype before and during pregnancy in different part of the world and to rule out whether it should be a routine test.
References
- Mary L.T. The Rh, Lewis, and others Blood group Systems in: Fundamentals of Immunohematology, Theory and Technique. Lea and Febiger, Philadelphia 1989; 127-131.
- Szymanski I.O and Arasᵶkiewicz, P. Quantitative studies on the D antigens of red cells with the Du phenotype transfusion 29(2): 103-105
- Walters A. H. Laboratory aspects of blood transfusion, September 2016
- Marcela, C. and Anatole, L. Antigens in human blood. In: Hoffbrand A.V, Lewis, S.M and TuddenhamEdward.G Post graduate Haematology4th Edition, Reed Educational and Publishing Ltd. 1999; 195 – 196.
- Nwauche CA and Ejele OA Rhesus D Negative Status in Females of Reproductive age in the Niger Delta area of Nigeria. Sahel med. J. 2004; 7 (2)64-68
- Falusi AG, Ademowo OG, Latunji CA, Okeke AC, Olatunji PO. Et al Distribution of ABO and RH genes in Nigeria AfriJ.Med. Sci. 2000 Mar;29(1) 23-26
- Odunaiya OA Serological study of the ABO and Rhesus blood group of 11, 120 pregnant women in Lagos Nig. Med J 1976; 6(3):279-280
- Worlledge S, Ogiemudia SE, Thomas CO,Ikoku BN, Lazzatto L: Blood group Antigens and Antibodies in Nigeria Nig.Ann.Trop.Med. Parasitol. 1974; Sep; 68(3); 249-264
- Peter D Issitt, David JAnstee: Applied Blood group Serology 4th Ԑd Montgomery Scientific Publication Durham 1998
- Ajayi G. Rhesus Cell Isoimmunization and ABO Incompatibility In: Text Book of Obstetrics and Gynecology for Medical Students 2nd Edition, Editor: Akin Agboola, Pub: Heinemann Educational Books (Nigeria) Plc. 2006:381 -38
- In: Dacie JV, and Lewis SM (eds). Practical Haematology 8thedition Churchill-Livingstone, Edinburgh 1995; pp 480 - 486).
- Kagu MB Ahmed S.G. &Olasoji T.A. The Prevalence and Clinical Significance of Du phenotype in Rhesus D Negative Pregnant Women in Maiduguri, Nigeria. Journal of Health and Biomedical Sciences 2005, 4:180 – 182.
- Joseph KS. Controlling Rh haemolytic disease of the newborn in India Br. J. Obstet andGynaecol. 1991 Apr;98(4):369-77
- Mak KH, Yan KF, Cheng SS, Yuen MY: Rh Phenotypes of Chinese blood donors in Hongkong with special reference to weak D antigens. 1. Transfusion. 1993 Apr;33(4):348-51
- Nwauche CA, Ejele OA, Okpani AO The prevalence of Du phenotype among Rhesus D negative females in Port Harcourt, Nigeria Afr J ReprodHealth. 2003Apr; 7(1): 27-31.