Information
Journal Policies
The Impact of Transvaginal Meshes on Sexual Function-the Provis Study
Huelder T1,Lobodasch K2,Pauli F3,Adelhardt W4,Hornung R5
Copyright : © 2017 . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction and hypothesis: Due to a potential risk of de novo dyspareunia, transvaginal meshes (TVM) are mainly used in postmenopausal women and in case of recurrent prolapse. Partially absorbable TVM are based on a highly flexible macroporous polypropylene of which half is absorbed within 84 days. These meshes have been assumed to affect sexual experiencing less than conventional TVM do. Therefore, we hypothesized that there is no worsening in vita sexualis after implantation of this product.
Methods: We conducted a prospective single-arm multicentre post-marketing study with intrapersonal comparison. Prolapse was quantified by ICS-Pelvic organ prolapse quantification system (POPQ). Patients filled in the validated German versions of the Female Sexual Function Index Questionnaire (FSFI-d) and the Pelvic Floor Questionnaire (PFQ) before and 12 months after mesh implantation. Twelve months after surgery patients were interviewed on their level of satisfaction with the operation by a Visual Analog Scale (VAS), the Patient Global Impression (PGI) question and the question whether they would undergo that procedure again. Patient accrual was closed after11 patients due to the withdrawal of the product from the market.
Results: Postoperative FSFI-d total score showed not only non-inferiority but even superiority compared to baseline. FSFI-d subscore pain also disproved non-inferiority and showed a tendency towards superiority. All PFQ subscores improved 12 months after surgery. Patient satisfaction was high.
Conclusions: Despite the lack of statistical power, there was no worsening of sexual experiencing following implantation of TVM.
Pelvic Organ Prolapse, Transvaginal Mesh, Dyspareunia, Sexual Function,Gynecology,Obstetrics
1. Introduction
Pelvic organ prolapse (POP) is defined as the descensus of intraabdominal organs into the vagina or even below the hymen. POP may occur in the anterior (bladder), the middle (uterus or vaginal vault) or the posterior compartment (bowel) of the lower pelvis. A woman’s lifetime risk to undergo surgery for POP or incontinence is 11.1%, as reported by Olsen (1997) who investigated data from around 150’000 women in a retrospective cohort study. Relapse surgery was indicated in almost 30% of the cases, as symptomatic recurrent prolapse is known to deteriorate the patient’s quality of life. The interval between relapse surgeries decreased from operation to operation [1]. Multiple operations are often associated with an increased risk of surgical or anaesthesialogical complications. Therefore, particularly in young women with a long life expectancy, recurrent POP should be avoided.
Some POP are sufficiently treated by conservative treatment such as pelvic floor muscle training, pessaries etc. However, others require surgical intervention. Traditional surgical strategies for treating POP are colporrhaphy with or without sacrospinous fixation. Newer pelvic floor repair techniques involve the use of meshes. Meshes have been successfully used for a long time in abdominal hernia surgery. Transvaginal meshes (TVM) reinforce the tissue and stabilize the fascial structures of the pelvic floor. Reisenauer (2007) showed that if TVM are applied as recommended, injuries of the major surrounding neurovascular structures can be avoided and defects in all three compartments of the pelvic floor can be repaired [2]. A randomized controlled study compared traditional pelvic floor repair with mesh-supported repair and showed a reduction of anatomic recurrence rates from 41% to 13% within 3 years if a mesh was used for the anterior vaginal wall repair [3]. However, there is a concern on dyspareunia directly caused by the meshes themselves, their shrinking, or by their exposure to the vaginal surface.
Dyspareunia (recurrent or persistent genital pain associated with sexual intercourse) is a common problem in sexually active women undergoing POP surgery. Due to not standardised definitions, rates of dyspareunia in a normal population range from 8% to 21.8% [4]. Up to 31% of sexually active patients complain of dyspareunia due to POP [5,6]. On one hand TVM have a lower rate of POP recurrence than traditional repair has. On the other hand, there are only a few studies investigating sexual function after pelvic floor repair, especially with TVM. The rate of de novo or worsened dyspareunia in these studies is controversial, ranging from 0-24% [5-8].
Due to the potential risk of de novo dyspareunia, TVM are mainly used in postmenopausal women and in case of recurrent prolapse. Partially absorbable meshes might have the potential for less impact on sexual experiencing compared to conventional non-absorbable meshes.
The aim of our study was to show that partially absorbable TVM do not impair sexual function, and particularly do not cause or worsen dyspareunia.
2. Materials And Methods
PROLIFT+MTM is a TVM that consists of macroporous polypropylene, a synthetic material which causes less foreign body response compared to conventional meshes. In detail, PROLIFT+MTM combines the durability of PROLENE® suture material with the absorbability of MONOCRYL® suture material. On average, half of the material (i.e. 51% which corresponds to the MONOCRYL® part of the mesh) is absorbed within 84 days. Large pores of the mesh allow good tissue integration.
PROLIFT+MTM is available as total implant, anterior implant and posterior implant. The total implant is shaped for performing a total vaginal repair. It has six straps: four for securing the anterior portion of the implant via a transobturator approach and two for securing the posterior portion of the implant in the sacrospinous ligament via a transgluteal approach. The anterior implant is shaped for repair of anterior vaginal defects and has four straps that are secured via a transobturator approach. The posterior implant is shaped for repair of posterior and/or apical vaginal vault defects. It has two straps that are secured in the sacrospinous ligament via a transgluteal approach.
PROLIFT+MTM was used as described by Reisenauer (2007)[2] and Fatton (2007)[9].
Participating surgeons had performed a minimum of 30 PROLIFTTM or PROLIFT+MTM procedures before participating in the study.
Study Design: We conducted a prospective single-arm multicentre post-marketing study with intra individual comparison. Patients with POP stage 2 or higher (according to ICS-POPQ[10]) were operated with an anterior and/or posterior or total transvaginal mesh implant.
We hypothesized that there is no worsening in vita sexualis with PROLIFT+MTM. As far as the primary objective is concerned, vita sexualis was assessed using the Female Sexual Function Index (FSFI-d), a validated 19-item questionnaire for the assessment of female sexual dysfunction. This questionnaire has been validated for the use in German speaking countries [11]. The primary endpoint was assessed by intrapersonal paired comparison, preoperative versus 12 months postoperative, Secondary objectives included the assessment of pain (FSFI-d pain sub score), pelvic floor function (German version of pelvic floor questionnaire, PFQ) [12], patient satisfaction, recurrence, mesh exposure and safety. Ethical approval was obtained from local Human Subjects Review Committee and the study was registered under ClinicalTrials.gov (NCT01997996).
Due to the withdrawal of the study product from the market we stopped recruitment after inclusion of 11 patients. The withdrawal was by decision of the manufacturer and not enforced by health care authorities. Customers have not been provided with further insight into the decision process of the manufacturer.
Patient Selection and Characteristics: In order to be included in this study, subjects must meet all inclusion and exclusion criteria listed in table1. Patient characteristics at baseline are shown in table 2.
Assessments: Sexual function as the primary endpoint was assessed comparing the FSFI-d total score at 12 months following surgery to the preoperative baseline score. The minimal score is 2, the maximum is 36 points. The evaluation of pain during sexual intercourse was assessed comparing the FSFI-d pain subscore at 12 months following surgery to preoperative baseline subscore. Pain was assessed in questions 17 to 19 of the FSFI-d. A minimal score of 0, and a maximum of 6 points can be reached[11].
Pelvic floor function was assessed using the validated self-administered German pelvic floor questionnaire preoperatively and at 12 months postoperatively (Deutscher Beckenboden-Fragebogen, validated German version of the Australian Pelvic Floor questionnaire, PFQ)[12]. Additive scores were calculated separately for bladder, bowel, prolapse and sexual function domains. Resulting scores were divided by the number of relevant questions within each domain and multiplied by a factor of 10, resulting in values between 0 and 10 for each of the four domains and a maximum total pelvic floor dysfunction score of 40.
Patient satisfaction was assessed at 12 months postoperatively by utilising the following three tools: The satisfaction Visual Analogue Scale (VAS) system used in this study has been adapted from the one developed by Bullens (2001) [13] to evaluate patient satisfaction after total knee arthroplasty at follow-up. The scale consists of a 100-mm-long horizontal line ranging from “completely satisfied” to “totally unsatisfied”. On top of the scale the question “How satisfied are you with the result of your operation?” is placed. All patients were asked to mark the line at a point that matches their satisfaction. With a ruler, the number of millimetres was measured and converted to points. The satisfaction VAS system ranges from 0 (completely satisfied) to 100 (totally unsatisfied) points.
One year after surgery, the patients were asked the following Patient Global Impression (PGI) Question: “Compared with how you were doing before your recent pelvic floor operation, how would you rate your situation during the last 12 months: much better/a little better/about the same/a little worse/much worse.” This question has been evaluated in a study to assess the reliability and validity of condition-specific health-related quality-of-life measures in women who were treated surgically for POP and urinary incontinence[14].
Additionally, the patients were asked whether they would have that operation done again or not. This is a “yes” or “no” outcome variable.
Statistical Approach: A paired t-test was used for statistical analysis. To reach statistical power we aimed to include 125 patients. This assumes a one-sided paired t-test for non-inferiority with significance level 0.025, 90% power, and non-inferiority margin of 3.3 points in FSFI-d total score. The estimated standard deviation for the difference between pre-operative and post-operative scores is 9.4, as computed from Pauls (2007) [15]. Final sample size estimate also assumes a drop-out rate of no more than 30%. Secondary endpoints analysis includes the difference in postoperative FSFI-d pain subscore (minimal score of 0, maximal score of 6 points), compared with preoperative pain subscore using paired t-test, with a non-inferiority margin of 1 point.
3. Results
One patient was lost to follow-up.
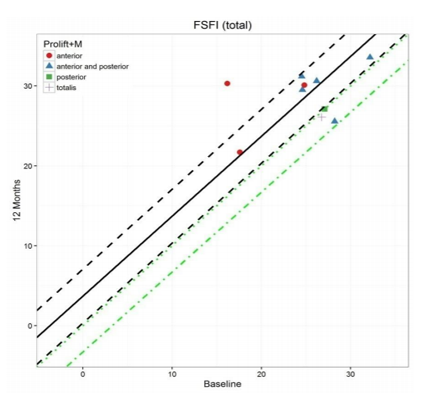
Primary Endpoint Total FSFI-d scores are on average 3.72 (95% CI (0.35, 7.09)) higher at 12 months than at baseline (p = 0.00055, with non-inferiority margin of -3.3). A higher score indicates less sexual problems. As the lower bound of the confidence interval is above both the non-inferiority margin and above 0, strict superiority is implied (p = 0.0171). Thus, postoperative FSFI-d total score shows not only non-inferiority but even superiority compared to the baseline (Figure. 1).
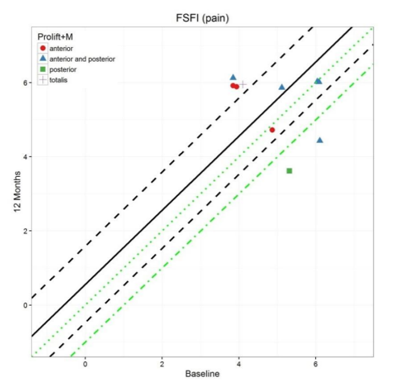
Secondary Endpoints FSFI-d pain subscores are on average 0.56 (95% CI (-0.47, 1.59) higher at 12 months than at baseline (p = 0.0038, with non-inferiority margin of -1)). Here, too, a higher score indicates less sexual problems. As the lower bound of the confidence interval is above the non-inferiority margin but not above 0, strict superiority is not shown (p = 0.12).Therefore, FSFI-d pain subscore also disproves non-inferiority and shows a tendency towards superiority (Figure . 2).
Results of the PFQ show improvement of all subscores (bladder, bowel, prolapse, sexual function) 12 months after operation (sexual function, see Figure. 3).
Patient satisfaction measured by VAS and PGI documents the patients overall satisfaction with the operation and its outcome. Median VAS was 2.5 (range 0-20) on a scale from 0-100 (0 = very satisfied, 100 = not at all satisfied). 9/10 patients answered the PGI question with “much better”, one patient assessed her status as “unchanged”.10/10 patients would choose the operation again.
No recurrence (defined as POP-Q ≥ Stage 2) was seen. One patient showed a small mesh exposure (< 1cm).
Safety
14 mild to moderate adverse events but no serious adverse events or serious adverse device effects occurred. Most events were not related to device or surgical procedure.
4. Discussion
The literature shows controversial findings regarding sexual outcome after prolapse repair. Kuhn (2009) showed that sexual function after native tissue prolapse repair is improved and dyspareunia is less common than before surgery [16]. In the same year Altman (2009) showed a worsening of overall sexual function scores after insertion of TVM while at the same time dyspareunia did not change significantly. The decreased sexual function scores in his study were mainly attributed to behavioural-emotive and partner-related items[17]. If meshes are compared to traditional interventions for POP, dyspareunia is possibly the same in both groups or even less in the mesh group (9% mesh versus 16% colporrhaphy) [8]. A recent review on sexual function after prolapse repair assumes a negative impact of TVM on sexuality while the data were inconsistent[18]. Indeed, a Cochrane Database analysis from 2016 on 11 studies with 764 participants reveals that meshes have a lower risk for de novo dyspareunia than native tissue repair, but the quality of evidence was low[19].
As far as we can deduct from our results, implantation of TVM does not seem to worsen sexual life. In contrary, our study implies a tendency towards improvement in sexual function after mesh-supported surgery for POP – at least for partially absorbable meshes. Patient satisfaction with study procedure and material is high and function of all pelvic floor compartments is improved. Improvement of sexual function might mainly be explained by elevation of the prolapse. But even if we concentrate only on dyspareunia we did not see any worsening after the operation.
The main limitation of our study is that, unfortunately, we could not reach statistical power due to the ahead of time study termination. Further prospective studies need to follow to verify our hypothesis. It would also be desirable to conduct this study as a randomized controlled trial comparing intra individual pre/postoperative changes between a conventional surgery group and a TVM group. But to our opinion, indications for conventional POP repair vary substantially to those for mesh supported surgery. Therefore, a randomized controlled trial might be difficult to be performed. There is currently a wide range of meshes on the market which are made from various materials and are designed for various ways of fixation (i.e. transobturator approach versus single incision, fixation of the middle compartment versus no concurrent fixation, anchors versus stitches). This fact complicates future interpretation of results and their generalization not only concerning dyspareunia but also concerning all functional and anatomical outcome measures.
5. Conclusions
Although our study lacks statistical power to reach significance, we present good evidence, that implantation of partially absorbable TVM for the treatment of POP does not negatively affect sexual function. The implantation of these meshes seems to improve the function of all pelvic floor compartments, but especially the bladder function and bulge symptoms. No major complications - caused by the device or the type of surgery occurred. Hence, neither sexual activity nor age are contraindications for this type of surgery if mesh reinforcement of the pelvic floor structures is indicated.
References
- Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL (1997) Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstetrics and gynecology 89 (4):501-506. doi:10.1016/s0029-7844(97)00058-6
- Reisenauer C, Kirschniak A, Drews U, Wallwiener D (2007) Anatomical conditions for pelvic floor reconstruction with polypropylene implant and its application for the treatment of vaginal prolapse. European journal of obstetrics, gynecology, and reproductive biology 131 (2):214-225. doi:10.1016/j.ejogrb.2006.03.020
- Nieminen K, Hiltunen R, Takala T, Heiskanen E, Merikari M, Niemi K, Heinonen PK (2010) Outcomes after anterior vaginal wall repair with mesh: a randomized, controlled trial with a 3 year follow-up. American journal of obstetrics and gynecology 203 (3):235.e231-238. doi:10.1016/j.ajog.2010.03.030
- Latthe P, Latthe M, Say L, Gulmezoglu M, Khan KS (2006) WHO systematic review of prevalence of chronic pelvic pain: a neglected reproductive health morbidity. BMC public health 6:177. doi:10.1186/1471-2458-6-177
- Hinoul P, Ombelet WU, Burger MP, Roovers JP (2008) A prospective study to evaluate the anatomic and functional outcome of a transobturator mesh kit (prolift anterior) for symptomatic cystocele repair. Journal of minimally invasive gynecology 15 (5):615-620. doi:10.1016/j.jmig.2008.05.009
- Gauruder-Burmester A, Koutouzidou P, Tunn R (2009) Effect of vaginal polypropylene mesh implants on sexual function. European journal of obstetrics, gynecology, and reproductive biology 142 (1):76-80. doi:10.1016/j.ejogrb. 2008.09.010
- de Tayrac R, Deffieux X, Gervaise A, Chauveaud-Lambling A, Fernandez H (2006) Long-term anatomical and functional assessment of trans-vaginal cystocele repair using a tension-free polypropylene mesh. International urogynecology journal and pelvic floor dysfunction 17 (5):483-488. doi:10.1007/ s00192-005-0046-x
- Nguyen JN, Burchette RJ (2008) Outcome after anterior vaginal prolapse repair: a randomized controlled trial. Obstetrics and gynecology 111(4):891-898. doi:10.1097/ AOG.0 b013e31816a 2489
- Fatton B, Amblard J, Debodinance Pea (2007) Transvaginal repair of genital prolapse: preliminary results of a new tension-free vaginal mesh (Prolift(TM) technique) - a case seires multicenter study. Int Urogynecol J.
- Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, Shull BL, Smith AR (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. American journal of obstetrics and gynecology 175 (1):10-17
- Berner M, Kriston L, Zahradnik HP, Härter M, Rohde A (2004) Validity and Reliability of the German Female Sexual Function Index (FSFI-d). Geburtshilfe und Frauenheilkunde 64 (3):293-303. doi:10.1055/s-2004-815815
- Baessler K, Kempkensteffen C (2009) [Validation of a comprehensive pelvic floor questionnaire for the hospital, private practice and research]. Gynäkol Geburtshilfliche Rundsch 49:299-307. doi:10.1159/000301098
- Bullens PH, van Loon CJ, de Waal Malefijt MC, Laan RF, Veth RP (2001) Patient satisfaction after total knee arthroplasty: a comparison between subjective and objective outcome assessments. The Journal of arthroplasty 16 (6):740-747. doi:10.1054/ arth. 2001.23922
- Wren PA, Janz NK, Brubaker L, Fitzgerald MP, Weber AM, LaPorte FB, Wei JT (2005) Reliability of health-related quality-of-life measures 1 year after surgical procedures for pelvic floor disorders. American journal of obstetrics and gynecology 192 (3):780-788. doi:10.1016/j.ajog.2004.10.603
- Pauls RN, Silva WA, Rooney CM, Siddighi S, Kleeman SD, Dryfhout V, Karram MM (2007) Sexual function after vaginal surgery for pelvic organ prolapse and urinary incontinence. American journal of obstetrics and gynecology 197 (6): 622.e621-627. doi:10.1016/j.ajog. 2007.08.014
- Kuhn A, Brunnmayr G, Stadlmayr W, Kuhn P, Mueller MD (2009) Male and female sexual function after surgical repair of female organ prolapse. The journal of sexual medicine 6 (5):1324-1334. doi:10.1111/j.1743-6109.2009.01229.x
- Altman D, Elmer C, Kiilholma P, Kinne I, Tegerstedt G, Falconer C (2009) Sexual dysfunction after trocar-guided transvaginal mesh repair of pelvic organ prolapse. Obstetrics and gynecology 113 (1):127-133. doi:10.1097/ AOG.0b013e3181922362
- Shatkin-Margolis A, Pauls RN (2017) Sexual function after prolapse repair. Current opinion in obstetrics & gynecology 29 (5):343-348. doi:10.1097/gco.0000000000000403
- Maher C, Feiner B, Baessler K, Christmann-Schmid C, Haya N, Marjoribanks J (2016) Transvaginal mesh or grafts compared with native tissue repair for vaginal prolapse. The Cochrane database of systematic reviews 2:Cd012079. doi:10.1002/14651858.cd012079