Information
Journal Policies
Transplantation in Patients with Autoimmune Liver Diseases
Tsvetelina Velikova MD PhD
Copyright : © 2018 . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Autoimmune diseases of the liver, autoimmune hepatitis (AIH), primary biliary cirrhosis (PBC) and primary sclerosing cholangitis (PSC), often lead to organ failure which indicates the need of allogeneic organ transplantation as definitive therapy as well as other liver pathology. One has kept in mind the immunological mechanisms of the underlying autoimmune diseases, the immune-mediated processes occurring after transplantation, and also the possibility of recurrence or de novo origin of the autoimmune liver disease. The outcomes of the intervention for these patients are very good, despite the high frequency - of recurrence of the liver disease. Early diagnosis of relapse and de novo occurred illness is critical for proper treatment and sufficient survival of the graft and the patient.
liver transplantation, autoimmune liver disease, autoimmune hepatitis, primary biliary cirrhosis, primary sclerosing cholangitis, Gastroenterology
1. Introduction
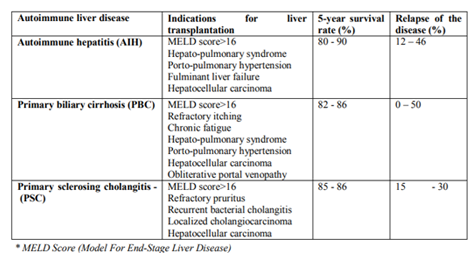
Autoimmune diseases of the liver often lead to organ failure which raises the issue of allogeneic transplantation as definitive therapy. Immunological mechanisms of the underlying autoimmune diseases, however, and the immune-mediated processes occurring after transplantation despite the administration of immunosuppressive therapy, define a number of problems in these patients. In addition to the risks associated with the transplantation itself, consideration should also be given to the possibility of recurrence or de novo origin of the autoimmune liver disease [1].Table 1 presents the main liver diseases that require liver transplantation, as well as the prognosis after transplantation [1].
2. Autoimmune Hepatitis And Liver Transplantation
Of patients with AIH, only about 10% do not respond to immunosuppressive therapy and need a liver transplant in the progression of the liver disease. Candidates with AIH for priority liver transplantation are most often those who have not achieved remission after a 4-year treatment period, and patients with acute liver insufficiency who are unaffected by the therapy administered; and also patients reached end-stage liver cirrhosis and those which developed hepatocellular carcinoma [2].Acute liver failure as a complication of AIH can occur in approximately 20% of patients. One-third of them respond to corticosteroid therapy, but for the rest, emergency liver transplantation is the only treatment [3]. Other criteria for prioritization and emergency liver transplantation are MELD score > 28, the presence of massive necrosis on histological examination, lack of normalization of bilirubin and INR after first four days of treatment, and a lack of change in the MELD score after seven days of corticosteroid treatment. During monitoring of clinical and laboratory parameters in the course of corticosteroid therapy when there is an absence of effect after treatment or even worsening within the first week, these patients may be pulled back to the waiting list for liver transplantation [3].After liver transplantation, the most widely used treatment regimen is the combination of prednisolone and calcineurin inhibitors, where a 5 - and 10 – year survival rates are 80- 90% and 75%, respectively, with 1- and 5-year survival of the graft - 84% and 75%, respectively.
3. Primary Biliary Cirrhosis And Liver Transplantation
Indications for liver transplantation in PBC are MELD score > 16, refractory pruritus, obstructive portal venopathy, hepatocellular carcinoma (Table 1)[1]. Retrospective studies have reported survival rates of the patient after transplantation as follows: from a living donor 1 -, 3 - and 5-year - 94%, 91% and 82%, resp., and the survival rates of the graft: 85%, 83% and 75%, resp., and from deceased donor - 90%, 87%, and 85% for the patients and 85%, 83% and 81% for the graft, resp. [2,4].
4. Primary Sclerosing Cholangitis And Liver Transplantation
Liver transplantation is discussed in PSC patients when they have reached a terminal stage of liver cirrhosis - MELD score > 16. In some cases, non-treatable pruritus, recurrent bacterial cholangitis in the presence of bile strictures that cannot be endoscopically managed and the presence of localized cholangiocarcinoma, transplantation can be performed regardless to the MELD score [1,2,4]. When liver transplantation is performed, Roux-en-Y anastomosis is preferred because the illness often affects ductus choledochus and may reoccur. It is also thought that the colectomy could prevent the recurrence of the disease after liver transplantation. The outcomes of the transplantations are usually more than satisfactory [4].It should be kept in mind that children with PSC often have chronic inflammatory bowel disease (ulcerative colitis, Crohn's disease) and high titers of antinuclear antibodies (ANA) and/or anti-smooth muscle antibodies (ASMA), high levels of IgG, interface hepatitis. Despite the immunosuppressive therapy (mainly corticosteroids and azathioprine), this disease of the biliary tract progresses resulting in the need for liver transplantation in up to 50% of cases [1].The outcomes of liver transplantation in PSC showed very good survival rates at 1st, 2nd, and 5th year - 90%, 86%, and 85%, respectively, and survival of the graft - 82%, 77%, and 72%, respectively [3].
5. Risk Of Recurrence Of Underlying Autoimmune Liver Disease After Liver Transplantation
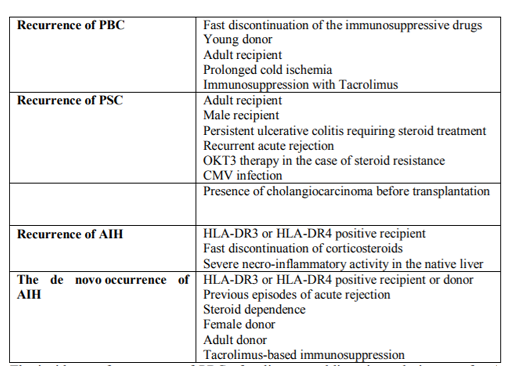
The relapses of the underlying autoimmune liver disease after liver transplantation are often reported (Table 2) [1].
The incidence of recurrence of PBC after liver transplantation is 0 - 50%, most often in 3-5 years. The wide range of differences documented in the different centers is probably due to the reduced number of biopsies in the transplanted patients. Diagnosis of PBC in the graft is harder than in the native liver [5]. The persistence of immunological findings, such as high levels of anti-mitochondrial antibodies (AMA) and IgM, suggests that the immune defect is not corrected by the removal of the affected liver and administered immune
suppression. The histological examination confirms the relapse or the new appearance of PBC in the graft on the basis of the following picture: the presence of granulomatous biliary tract damage, lymphoplasmacytic infiltrates, lymphoid aggregates, etc. In contrast to the high incidence of disease recurrence, there is evidence of the very rare need for re-transplantation in this disease [5].
For PSC, the incidence of recurrence is 15-30% and the average time between liver transplantation and recurrence is 3-5 years. The distinction between the relapse and newly emerging secondary cholangitis is also difficult. It relies heavily on visuals differentiation of diffuse strictures of the bile ducts (via MRI cholangiography or percutaneous trans-hepatic cholangiography), but also on the exclusion of all other reasons for them. The typical histological findings are fibro- obliterative lesions of the bile ducts
or periductal concentric fibrosis, which, however, are observed in less than 10% of patients with relapsed PSC. In children with juvenile autoimmune sclerosing cholangitis, the recurrence after liver transplantation is about 70%, especially if accompanied by chronic inflammatory bowel disease, and is associated with serious graft damage and shortening of survival [5].As far as AIH is concerned, liver transplantation is a very successful method of treating, despite the chance of relapse in about 30% of patients - children or adults [5]. The diagnose of AIH recurrence relies on clinical manifestations, and positive autoantibodies and the occurrence of interface hepatitis on histology, along with an increase in aminotransferases, IgG levels, and response to treatment with prednisolone and Azathioprine [6]. Some genetic markers, such as the presence of HLA-DR3 and HLA-DR4, can be used to predict the relapse of AIH. In patients with an acute fulminant form of AIH, the likelihood of recurrence is lower than in those with a chronic form of AIH. This suggests that transplant patients due to chronic AIH are likely to have a resistance to immunosuppressive therapy while patients with fulminant hepatitis who were not immunosuppressed prior to liver transplantation had a better immunosuppressive response.
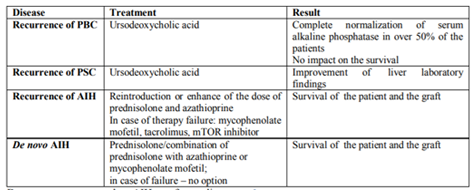
The principal treatment for the relapsing autoimmune disease is presented in Table 3[1].
De novo occurred AIH after liver transplantation was observed in patients who were transplanted for other liver diseases (i.e., extrahepatic biliary atresia, Alagille syndrome, acute liver failure, alpha-1- antitrypsin deficiency, primary familial intrahepatic cholestasis, PSC, and Budd-Chiari syndrome) [7].The immunological constellation for de novo occurred AIH is the following: hypergammaglobulinemia, the presence of autoantibodies ANA, ASMA, anti- LKM- 1 and others, as well as a histological picture of chronic hepatitis with portal and periportal inflammation, identical to classical AIH [7]. Suspicion for de novo occurred AIH raises when graft dysfunction origins which cannot be explained by rejection or surgical complications and, once diagnosed, should be aggressively treated. Treatment with prednisolone or prednisolone in combination with azathioprine or mycophenolate mofetil results in very good results in both survivals of the patients and graft. It is interesting to note that these patients do not respond satisfactorily to a short-term - high-dose corticosteroid drugs use that are used to treat acute cell rejection but respond only to standard AIH treatment, indicating the need for an early diagnosis to prevent the loss of the graft. The significance of the sustained corticosteroid treatment has been demonstrated - in a study reporting that all steroid-naive patients developed cirrhosis of the liver, died or had been re-transplanted until none of the patients treated with steroids developed a progressive disease. In conclusion, de novo occurred AIH does not respond satisfactorily to treatment for graft rejection but respond well to classical AIH treatment [6].
6. Conclusion
Patients with autoimmune liver diseases are indicated for liver transplantation as well as other patients with liver pathology. The outcomes of the intervention for these diseases are very good, despite the high frequency - of recurrence of the liver disease. Early diagnosis of relapse and de novo occurred illness is critical for proper treatment and sufficient survival of the graft and the patient.
References
- Spasov L., M. Vasilev, K. Penkova, I. Altankova, D. Baltadzhieva. Transplantation of organs in autoimmune diseases. B: Autoimmune Diseases in Clinical Practice, 2015, Sofia, pp. 393-406.
- Kashyap R, Safadjou S, Chen R, Mantry P,Sharma R, Patil V, et al. Living donor and deceased donor liver transplantation for autoimmune and cholestatic liver disease-an analysis of the UNOSdatabase. J Gastrointest Surg 2010; 14: 1362-1369.
- Futagawa Y, Terasaki PI An analysis of the OPTN / UNOS liver transplantation registry. Clin Transpl 2004: 315-329.
- Liberal R1, Zen Y , Mieli-Vergani G, Vergani D. Liver transplantation and autoimmune liver diseases. Liver Transp. 2013; 19 (10): 1065-77.
- Rowe IA, Webb K, Gunson BK, Mehta N, Haque S, Neuberger J. The impact of disease recurrence on graft survival following liver transplantation: a single center experience. Transpl Int 2008; 21: 459-465.
- Mazariegos GV, Reyes J, Marino IR, Demetris AJ, Flynn B, Irish W, et al. Weaning of immunosuppression in liver transplant recipients. Transplantation 1997; 63: 243-249.
- Kerkar N, Hadzi N, Davies ET, Portmann B, Donaldson PT, Rela M, et al. De- novo autoimmune hepatitis after liver transplantation. Lancet 1998; 351: 409-413.