Information
Journal Policies
Perforated Jejunal Diverticulum Due to Mechanical Ileus: A Rare Combination of Circumstances
A.J. Van Nieuwkoop1*, F.C. den Boer2
2.Department of Surgery, Zaans Medical Centre, The Netherlands.
Copyright : © 2018 . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Small bowel diverticula, especially the more common duodenal, usually remain asymptomatically. Jejunal diverticulosis may present more acutely and up to 15% develop complications that require surgery. We present a 69-year-old woman with a perforated jejunal diverticulum due to a mechanical ileus. She was seen at the emergency department with a 2-day history of lower abdominal cramps, nausea and vomiting. The computed tomography scan showed an image suspected for an ileus due to an internal herniation. An emergency laparotomy was performed and an obstructing adhesion was seen with proximal strongly dilated loops, multiple expanded jejunal diverticula and one of these was necrotic and perforated. Surgical removal of the necrotic diverticulum and closure of the defect was ultimately inadequate, because the patient developed three weeks postoperatively a sepsis based on a new perforation of the previously sutured diverticulum of the jejunum. Partial resection of the affected jejunum and side-to-side anastomosis did not have the desired effect and the patient died 30 days after the initial operation. The best treatment of jejunal diverticulosis still unclear, with conflicting recommendations in the literature. For patients diagnosed with a perforation and peritonitis, immediate segmental resection and primary anastomosis remains the preferred intervention.
Diverticulum, jejunal, perforated, ileus, surgical, necrotic, segmental, resection, peritonitis, anastomosis.
1. Introduction
Diverticulosis of the small bowel is a relatively rare clinical entity, first described by Sommering in 1794 [1]. Small bowel diverticula, especially the more common duodenal, usually remain asymptomatically [2]. However, jejunal diverticulosis may present more acutely. Symptoms relating to its presence are non- specific, such as malabsorption and vague abdominal pain. Therefore, alternative small bowel disorders are usually considered and cause the delay in the correct diagnosis. As a result, complications that require surgery, such as bleeding, mechanical obstruction and perforation, increase up to 15% [3].
We present a patient with a perforated jejunal diverticulum due to a more distal obstruction of the small intestine, caused by an adhesion with a mechanical ileus.
2. Case Presentation
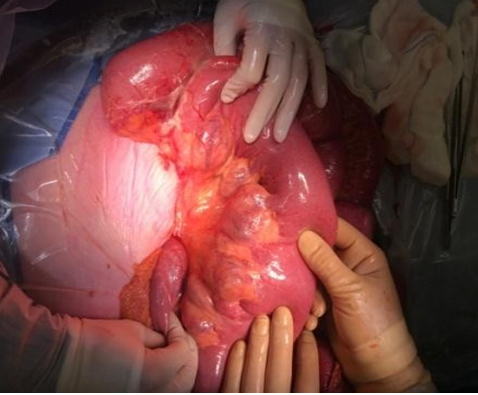
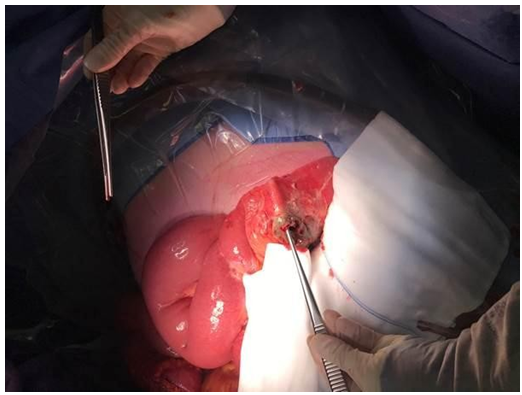
A 69-year-old woman was seen at the emergency department with a 2-day history of lower abdominal cramps, nausea and vomiting. Past medical history included chronic asymptomatic atrial fibrillation with a good left ventricular function, idiopathic Parkinson’s disease and an uterus extirpation. On physical examination, she was hemodynamically unstable after 500 cc filling, with a blood pressure of 100/65 mm Hg and a heart rate 100 bpm. Remaining vital parameters included a temperature of 37.1 C, respiratory rate 14 and oxygen saturation 93% on room air. There was tenderness in the right lower quadrant of the abdomen without signs of peritonitis. Labaratory investigations showed an initial white cell count of 9.9x10E9/L, a C-reactive protein of 96 mg/L and a lactate of 3.3 mmol/L. We started with 2 L infusion NaCL 0.9% with 80 mmol potassium. An ultrasound scan of the abdomen revealed dilated small bowel with wall thickening, a modest amount of ascites and a lot of air in the intestines. The next day, a computed tomography scan showed an image suspected for an ileus due to an internal herniation. Furthermore, there was a collaps from almost the entire colon and dilatation of the small bowel. In the CT room, the patient suddenly developed ventricular tachycardia for which electric cardioversion was applied. The patient was intubated on the Intensive Care and we started with ceftriaxone, metronidazole and a single gift of gentamycin. The result of the CT scan combined with the clinical decline of the patient required us to perform an emergency laparotomy. After opening the abdomen an obstructing adhesion of the distal part of the jejunum was seen with proximal strongly dilated loops. It also demonstrated multiple expanded diverticula on the mesenteric side of the jejunum and one of these was necrotic and perforated. A resection of the necrotic perforated diverticulum was performed and the remaining hole was sutured. The obstructing adhesion, the most likely cause of the expanded diverticula and the necrosis and perforation of one diverticulum, was devided.
Post-operatively, the patient was admitted 5 days in the Intensive Care Unit where she required ventilatory support and tube feeding. A highly sensitive E. Coli bacterium was isolated from the blood culture and the antibiotics were switched to Augmentin. After a few days, the patient could be detubated and there was a return to normal bowel function. Eleven days postoperatively, she was admitted to the regular surgical ward again and she recovered slowly in the next week. Unfortunately, despite the initial clinical progress, she suddenly developed signs of sepsis three weeks after the operation. On a CT scan, there was a thickened jejunal loop with a fluid collection and free air around it. Again, an emergency laparotomy was performed and a new perforation of the previously sutured diverticulum of the jejunum was seen. During the operation, approximately 50 cm of the jejunum was resected and a side-to-side anastomosis was constructed. Postoperatively, she recovered from her sepsis, but there seemed to be brain damage as evidenced by a failure to regain consciousness. The following days no improvement of her neurological situation was seen and in consultation with her family, abstinence from further treatment was instituted. The following day, 30 days after the initial operation, she died.
3. Discussion
Small bowel diverticula are commonly seen in the duodenum and the ileum. Only 18% of the small intestine diverticulas consists of jejunal diverticula [4]. There is an association of jejunal diverticula with diverticula at other sites, such as the colon (35%), the duodenum (26%) and the esophagus (2%) [5]. The etiology is not entirely clear. It is thought that these false diverticula develop as a result of peristaltic deficiencies and intestinal dyskinesia leading to high segmental pressure. As a result, herniation of the mucosa and submucosa on the mesenteric border occurs, trough gaps in the muscle layers along pathways of the visceral vessels [6, 7]. This role of visceral myopathy and weak intestinal wall structure also explains the causal association with connective tissue diseases such as scleroderma, CREST syndrome and Ehlers-Danlos syndrome [1]. Jejunal diverticula are in many cases asymptomatic, sometimes discovered incidentally in imaging studies or at laparotomy. The incidence of symptomatic small bowel diverticular disease is estimated at 0.5%. However, this might be an underestimation because this entity is usually associated with vague abdominal complaints. These symptoms such as vague cramping abdominal pain, along with postprandial flatulence, diarrhea and malabsorption are often attributed to small bowel enteropathies, gastro-oesophageal reflux disease or irritable bowel syndrome [6,8].Peritoneal irritation signs have been reported to be found on physical examination in approximately half of the patients [9]. The rarity of the disease and the varying presentation may explain why upwards to 15% of the patients will develop serious complications, such as obstruction, perforation, abscess, fistula and gastrointestinal bleeding [3,10].
On blood examination, systemic signs of inflammation such as elevated WBC count and CRP can be demonstrated. Stasis and bacterial overgrowth inside the diverticula can cause hyperbilirubinemia by bacterial mediated conjugation. Anemia can also be seen, because of bacteria release siderophores and upregulate hepcidin. Bacterial siderophores form significantly more stable complexes with iron than the siderophores of humans. This means that they can extract iron from the hemoglobin and transferrin in the human body. Hepcidin, the central iron regulating hormone, is synthesized in the liver. In chronic inflammation circulating cytokines cause an upregulation of hepcidin and as a result the iron remains in enterocytes and macrophages [7] Possible complications such as an ileus, a perforation or an abscess can be detected on radiological examination [11-13].
The best treatment of jejunal diverticulosis is still unclear, with conflicting recommendations in the literature. Reviewing the recent literature shows that patients with uncomplicated jejunal diverticulosis are treated conservatively [14,15].
If there are complications such as obstruction, bleeding or perforation, a more aggressive approach is warranted. If the clinical situation allows, elective surgery with resection and primary anastomosis can result in a good surgical outcome [10]. For patients diagnosed with free perforation and peritonitis, immediate segmental resection and primary anastomosis remains the preferred intervention [3,16,17]. However, a more recent series suggested laparoscopic lavage and drainage as a possibility in some cases with a sealed perforation without obstruction or fistula [18]. In addition, Novak et al. [19] have described a few cases where a localized perforation of jejunal diverticula could be treated with either intravenous antibiotic therapy or CT-assisted percutaneous drainage of the abscess.
Concerning our patient, we initially chose to divide the obstructing strand, to resect the necrotizing diverticulum and to close the resulting hole. The obstructive distal cord was the cause of the dilatation of the jejunum and the associated increased pressure had caused a perforation in one of the diverticula. So, we did not have the expectation that one of the other diverticula would perforate spontaneously in the future and we decided not to take the high risk of segmental resection and primary anastomosis with an associated high risk of anastomotic leakage because of the dilatation. During the first three weeks, she recovered well. Unfortunately, 3 weeks postoperatively our patient developed a new sepsis and again, a perforation in the sutured part of the jejunum was seen. The subsequent resection of 50 cm jejunum and the anastomosis unfortunately did not lead to full recovery. Retrospectively, it would have been better to perform the jejunal resection and primary anastomosis or an end enterostomy during the first operation. We recommend, using this patient history, not to be reluctant to resect a part of small intestine in patients with free perforated diverticula.
4. Conclusion
Although jejunal diverticula are not very common and are usually asymptomatic, upwards to 15% of the patients will develop serious complications, such as obstruction, perforation, abscess, fistula and gastrointestinal bleeding. We presented a patient with a perforated jejunal diverticulum due to a mechanical ileus in whom surgical removal of the necrotic diverticulum and closure of the defect was ultimately inadequate. Segmental resection and primary anastomosis or construction of an end enterostomy remains the preferred intervention for patients diagnosed with free perforation and peritonitis.
References
- Krisnamurthy S, Kelly MM, Rohrmann CA, Schuffler MD, Jejunal diverticulosis. A heterogenous disorder caused by a variety of abnormalities of smooth muscle or myenteric plexus, Gastroenterology. 1983 Sep; 85(3):538- 47.
- Tsiotos GG, Farnell MB, Ilstrup DM, Non- meckelian jejunal or ileal diverticulosis: an analysis of 112 cases, Surgery. 1994 Oct; 116(4):726-31; discussion 731-2.
- Wilcox RD, Shatney CH, Surgical significance of acquired ileal diverticulosis, Am Surg. 1990 Apr; 56(4):222-5.
- Akhrass R, Yaffe MB, Fischer C, Ponsky J, Shuck JM, Small-bowel diverticulosis: perceptions and reality, J Am Coll Surg. 1997 Apr;184(4):383-8.
- Baskin RH Jr, Mayo CW, Jejunal diverticulosis; a clinical study of 87 cases, Surg Clin North Am. 1952 Aug: 1185-96.
- Patel VA, Jefferis H, Spiegelberg B, Iqbal Q, Prabhudesai A, Harris S, Jejunal diverticulosis is not always a silent spectator: A report of 4 cases and review of the literature, World J Gastroenterol. 2008 Oct 14; 14(38):5916-9.
- Kavanagh C, Kaoutzanis C, Spoor K, Friedman PF, Perforated jejunal diverticulum: a rare presentation of acute abdomen, BMJ Case Rep. 2014 Mar 22;2014. pii: bcr-2013-202673. doi:10.1136/bcr-2013-202673.
- Edwards HC. Diverticula of the small intestine, Br J Radiol. 1949 Aug; 22(260):437-42.
- Horesh N, Klang E, Gravetz A, Nevo Y, Amiel I, Amitai MM, Rosin D, Gutman M, Zmora O, Jejunal diverticulitis, J Laparoendosc Adv Surg Tech A. 2016 Aug;26(8):596-9. doi: 10.1089/ lap.2016.0066. Epub 2016 May 16.
- Kouraklis G, Mantas D, Glivanou A, Kouskos E, Raftopoulos J, Karatzas G, Diverticular disease of the small bowel: Report of 27 cases, Int Surg. 2001 Oct-Dec;86(4):235-9.
- Coulier B, Maldague P, Bourgeois A, Broze B, Diverticulitis of the small bowel: CT Diagnosis, Abdom Imaging. 2007 Mar-Apr; 32(2):228-33. Epub 2006 Sep 12.
- Gayer G,Zissin R, Apter S, Shemesh E, Heldenberg E, Acute diverticulitis of the small bowel: CT findings, Abdom Imaging. 1999 Sep-Oct; 24(5):452-5.
- Greenstein S, Jones B, Fishman EK, Cameron JL, Siegelman SS, Small-bowel diverticulitis: CT-findings, AJR Am J Roentgenol. 1986 Aug; 147(2):271-4.
- Macari M, Faust M, Liang H, Pachter HL, CT of jejunal diverticulitis: Imaging findings, differential diagnosis, and clinical management, Clin Radiol. 2007 Jan; 62(1):73-7.
- Levack MM, Madariaga ML, Kaafarani HM, Non-operative successful management of a perforated small bowel diverticulum, World J Gastroenterol. 2014 Dec 28; 20(48):18477-9. doi: 10.3748/wjg.v20.i48.18477.
- Roses DF, Gouge TH, Scher KS, Ranson JH, Perforated diverticula of the jejunum an ileum, Am J Surg. 1976 Nov;132(5):649-52.
- Matteoni R, Lolli E, Barbieri A, D'Ambrosi M,Perforated jejunal diverticulitis: personal experience and diagnostic with therapeutic considerations, Ann Ital Chir. 2000 Jan-Feb; 71(1):95-8.
- Spasojevic M, Naesgaard JM, Ignjatovic, Perforated midgut diverticulitis: Revisited, World J Gastroenterol. 2012 Sep 14;18(34): 4714-20.
- Novak JS, Tobias J, Barkin JS, Nonsurgical management of acute jejunal diverticulitis: a review, Am J Gastroenterol. 1997 Oct; 92(10): 1929-31.