Information
Journal Policies
Antral Hemangioma: A Rare Cause of Gastrointestinal Bleeding
Chabib Fatima-Zahra1*, Imane Benelbarhdadi2, Fatima-Zohra Ajana2
2.Professor at the Faculty of Medicine and Pharmacy, Mohammed V University, Morocco.
Copyright : © 2018 . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Digestive hemangiomas are rare benign tumors, most often they are revealed by a GI hemorrhage. We report a case of antral Hemangioma presented by a recurrunt digestive bleeding. The diagnosis was suspected by upper endoscopy and confirmed by histology. The patient was treated by argon plasma coagulation (APC) with good clinico-biological evolution.
Antral Hemangioma, Argon Plasma Coagulation, Melena, Gastroenterology
1. Introduction
Hemangiomas are benign and rare tumors of the digestive tract. The diagnosis of these lesions is made by endoscopy, the treatment is endoscopic or surgical. We report a new case of antralhemangioma revealed by recurrent upper GI bleeding in form of melena.
2. Case Report
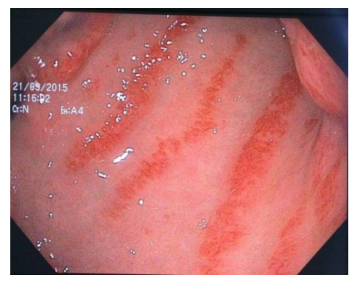
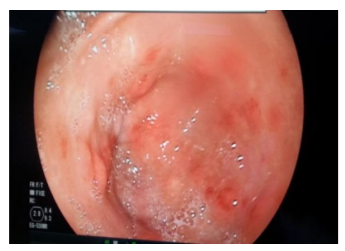
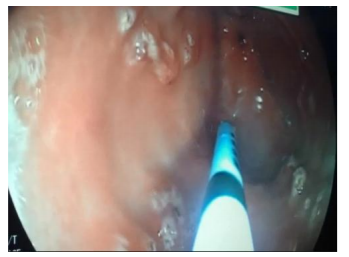
70-year-old woman, admitted to the emergency unitfor melena with anemic syndrome. With a history ofarterial hypertension under treatment, diabetes type 2 complicated with diabetic nephropathy under insulin, dyslipidemia under treatment presented by repeated episodes of melena treated symptomatically by transfusions and by oral iron supplementation. The clinical examination at admission included a patient in a moderate general condition (WHO = 1), hemodynamicallystable ; pale with melena at digital rectal examination. Biologically she had hypochromic microcytic anemia with a hemoglobin level of 6 g / dl. After blood transfusion, upper endoscopy performed showed an appearance of parallel linear antral congestive trabeculae converging towards the pylorus suggesting an ectasia or antralhemangioma (Figure 1). The histological study shows hemangioma. Colonoscopy with ileal intubationdid not show any other localization as well as an abdominal angiography scan and CT enterographywere normal. Therapeutically, she received local treatment by argan plasma electrocoagulation (APC) and 2 other sessions at 6 weeks interval with good clinical and biological evolution (Figure 2). However, 8 months later she recurred with anemic syndrome without external bleeding (Figure 3), and received the same treatment (Figure 4) with good evolution (1 year follow-up).
3. Discussion
The term "angioma" has long been used to describe both tumors and vascular malformations, in this case the International Society for the Study of Vascular Anomalies (ISSVA) adopted a classification which allows to distinguish them. Thus for tumors, we distinguish between benign tumors (angiomas or hemangiomas), tumors with intermediate or uncertain malignancy (hemangioendotheliomas) and malignant tumors (angiosarcomas) [1]. Hemangioma is a benign tumor that can be seen in many organs. GI hemangiomas are extremely rare, about 200 cases of gastrointestinal hemangiomas have been reported in the literature since 1839 [2]. The overall incidence of digestive hemangiomas is estimated at 1/14000 patients [3]and represent 0.05% of all gastrointestinal tumors and jejunal localization is the most common. Often it is unique but can be multiple or part of systemic vascular disorders: such as Bean syndrome (blue rubber bleb nevus, BRBNS), Maffucci syndrome and Klippel-Trenaunay-Weber syndrome [5]. Hemangiomas are observed at any age, as they have been reported in patients ranging from 2 months to 79 years. There inNo sexual predominance [4]. Clinically; GIhaemorrhage is the most common mode of presentation, more rarely unexplained anemia, occlusion or platelet sequestration [6]. Endoscopy is the method of choice in the diagnosis of these lesions. Gastrointestinal hemangiomas originate from submucosal vascular plexuses and may invade the muscular layer. They rarely exceed the serosa [7]. According to the endoscopic aspect, Abrahamson and Shandling have distinguished three types: The first type is capillary haemangioma, described as a small tuft of submucosal capillaries with intraluminal development that can sometimes be sessile or pedunculated; The second type is represented by the capillary and cavernous mixed hemangioma; The third type is cavernous hemangioma, the most common is in the form of dilated submucosal varicosities, whose colour varies from dark purple to a lighter bluish or sometimes red color associated with mucous congestion. The interest of imaging remains limited for the diagnosis of vascular anomalies and superficial mucosal lesions. Arteriography and angio-scanning require active bleeding to be useful for diagnosis [8]. Hemangiomas are benign tumors with a very good prognosis and are exceptionally fatal especially in the presence of endoscopy whose interest has far exceeded the stage of diagnosis. Indeed, endoscopy is the mainstay of treatment and must always be proposed as first intention. APC is considered the first-line endoscopic treatment in the management of gastrointestinal vascular lesions. The technique is safe, effective in the long term and has a net cost advantage over hospitalizations and repetitive transfusions. It can be used even in patients with comorbidities [9]. At the extreme, in rebellious cases, surgical resection may be discussed in localized forms. Low dose radiation therapy, cryotherapy, sclerotherapy or arterial embolization have been used in unresectable and diffuse haemangiomatosis with poor success[10].
4. Conclusion
Digestive hemangiomas with antral location are exceptional. Presented either by anemic syndrome or gastrointestinal bleeding. Endoscopy remains the gold standard for diagnosis and treatment, particularly by argon plasma electro coagulation.
References
- M. Wassef et al. Tumeurs et malformations vasculaires, classification anatomopathologique et imagerie. Annales de chirurgie plastique esthétique 51 (2006) 263–281.
- Garvin P, Herrman V, Kaminski D: Benign and malignant tumors of the small intestine. CurrProbl Cancer 1979, 3:4-46
- Ramanujam PS, Venkatesh KS, Bettinger L, et al . Hemangioma of the small intestine : case report and literature review. Am J Gastroenterol 1995 ; 90 : 2063-4.
- Enziger FM, Weiss SW: Soft tissue tumors. 3rd edition. St. Louis, Mo: Mosby-Yearbook; 1995:679-89 .
- Boyle L, Lack EE. Solitary cavernous hemangioma of small intestine. Case report and literaturereview. ArchPatholLab Med 1993 ; 117 : 939-41.
- Corsi A, Ingegnoli A, Abelli P, et al: Imaging of a small bowel cavernous hemangioma: report of a case with emphasis on the use of computed tomography and enteroclysis . ACTA BIOMED 2007; 78: 139-143
- Ruiz AR, Gınsberg AL: Giant mesenteric hemangioma with small intestinal involvement: An unusual cause of recurrent gastrointestinal bleeding and review of gastrointestinal hemangiomas. Dig Dis Sci 1999, 12:2545-51.
- Antonella Corsi, Anna Ingegnoli, Pietro Abelli, Flavia De Chiara et al. Imaging of a small bowel cavernous hemangioma: report of a case with emphasis on the use of computed tomography and enteroclysis . Acta Biomed. 2007; 78 (2): 139 .
- Kwan et al. APC in the Management of Vascular Lesions.Am J Gastroenterol 2006;101:58–63.
- MircelalKazimi et al A rare cause of recurrent gastrointestinal bleeding: mesenteric hemangioma. World Journal of Emergency Surgery 2009, 4:5