Information
Journal Policies
Effect of Smoking Index on Cardiovascular System in Some Libyans
Elmrghni S,Kaddura M
Copyright :© 2017 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Smoking is a major cause of cardiovascular disease (CVD) and causes one of every three deaths from CVD, according to the 2014 Surgeon General’s Report on smoking and health. Even people who smoke fewer than five cigarettes a day may show signs of early CVD. The risk of CVD increases with the number of cigarettes smoked per day, and when smoking continues for many years. Smoking Cigarettes with lower levels of tar or nicotine does not reduce the risk for cardiovascular disease. Exposure to second hand smoke causes heart disease in non-smokers. More than 33,000 non smokers die every year because of coronary heart disease caused by exposure to second hand smoke. Exposure to second hand smoke can also cause heart attacks and strokes in non-smokers. Smoking Index is a parameter used to express cumulative smoking exposure quantitatively. This is especially useful in defining risk ratio of a smoking related disease. This parameter is similar to Pack Year. In order to observe the effect of cigarette smoking on cardiovascular systems of active and passive Libyan smokers; 100 volunteers 50 males and 50 females were enrolled for the study and then further sub classified according to smoking index as mild, moderate and heavy. Furthermore our study also indicated that the effect of passive smoking as a risk for cardiovascular diseases is more in females than that in males, and female non-smokers have higher risk than that in males.
Keywords: Smoking; Libyans; Cardiovascular disease,Forensic Science
1.Introduction
The pathophysiological mechanisms by which smoking results in the development of atherothrombosis are unknown. However, suggested mechanisms include endothelial disturbance, changes in fibrin formation and turnover, changes in lipids and lipoproteins and reduced availability of antioxidants. It had been postulated that cigarette smoking is associated with abnormal lipid profile in the form of raised plasma triglycerides and cholesterol [1]. The impact of smoking on blood hemostatic mechanisms revealed increased levels of fibrinogen and alterations of fibrin turnover [2]. These changes were, smoke exposure correlated with the degree of elevated tissue plasminogen activator (t-PA) and Von Will brand factor antigen levels were shown in the coronary artery of smokers and indicate impaired fibrinolytic activity [2]. Moreover, smoking related alterations in blood clotting factors have been proved [[3],[4]]. Both active and passive smoking are associated with deterioration in the elastic properties of the aorta and big arteries [5].
Recent studies have suggested the involvement of impaired endothelial cell dependent vasodilatation in the genesis of smoking induced hypertension [3]. This impaired relaxation of the arteries may be, at least in part, mediated through the degradation of released nitric oxide (NO) by superoxide anions derived from cigarette smoke [[5], [6]]. Increased vascular tone in smokers has been claimed to be primarily due to sympathetic over stimulation as a direct effect of nicotine on sympathetic ganglia with release of catecholamines [7]. A role of endothelin-l, a potent vasoconstrictor, in the initiation of smoking associated vascular changes have also been postulated [[7], [8]], a role for smoking induced activation of renin-angiotensin system in the patho-genesis of vasomotor changes associated with smoking was also proposed. Smokers have also been shown to have reversible rise in blood viscosity compared to non smokers due to increased haematocrit value and plasma viscosity [2]. Rise in plasma viscosity is largely due to elevated fibrinogen levels together with acute phase reactant proteins such as alpha-2 macroglobulin [[9], [10].
2. Types Of Smokers
Types of active smokers include psychological smokers, indulgent smokers, tranquilization smokers, stimulation smokers and addictive smokers. In the addictive smokers the with-drawal symptoms are felt when the subject has been about 30 minutes without smoking and he has to smoke to relieve this tension [11,12].
Passive smoking is the involuntary inhalation of tobacco combustion products by non-smokers. The situation is characterized more precisely by the term forced smoking which should be used in preference to passive smoking [11]. Passive smoking is estimated to account for approximately 3000 new cases of lung cancer per year in the USA [12]. In passive smoking, environmental tobacco smoke (ETS) is inhaled by someone in the presence of active smoking [12]. The ETS emerges from either mainstream smoke which is emitted from the mouth piece during puffing and then exhaled by the smoker or side stream smoke which is emitted between puffs at the burning cone and from the mouth piece [13, 14].
Main stream smoke (MS) contributes about 15 to 43% of the particulate matter in ETS [13, 14].
Side stream smoke usually contains relatively high concentrations of many noxious substances including heavy metals. As particle sizes are smaller inside stream smoke than in main stream smoke, their deposition in the lung tissues of passive smokers reaches deeper into the alveolar spaces, some of the components of the inhaled side stream smoke occur in relatively higher concentration than in main stream smoke, such as, nicotine, benzene, and nitrosodimethylamine [[13], [14]].
3. Smoking Index
Smoking index (SI) is the product of multiplying the number of cigarettes smoked per day by the number of years of smoking. The smokers are categorized into: Mild Having less than 200 SI Moderate Having 200-600 SI Heavy Having more than 600 SI Both active and passive smoking expose an individual to the same substances but the relative concentrations differ. Thus, being exposed to passive smoking 2 hours/day for 25 years was found to be equivalent to having actively smoked an average of 20 cigarettes/ day for 20 years [15, 16].
4. Subjects And Methods
100 healthy volunteers consisting of 50active smokers adult males and 50 passive smokers adult females from different age groups (20-70 years). Which divided to (mild, moderate and severe) according to smoking index (the number of cigarettes smoked per day multiply by the duration of smoking by years).
Those volunteers selected when they presented with their relative patients in hospital after complete informed consent. All chosen subjects were medically examined in seven October hospital with negative past medical history (no diseases detected before especially heart diseases). Questioner form was designed to be filled with each volunteer to record all necessary personal data (these data includes personal information and medical history).
Data was analyzed by statistical package of social science (SPSS) Program.
Data was presented in percentage for comparing the variables, tables and pie charts were used to summarize and presenting the data.
5. Results
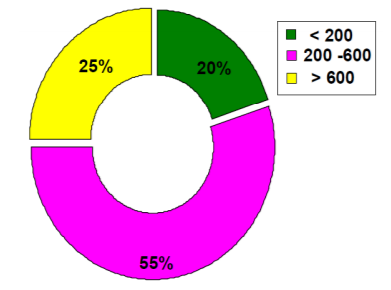
Table 1 and Figure 1 show the distribution of active smokers according to smoking index. Smoking index = number of cigarettes per day multiply by duration of smoking (in years) Mild smoking index < 200 = 20% 4 cases Moderate smoking index = 200-600 = 55% 11 cases Heavy smoking index > 600 = 25% 5 cases.
6. Discussion
Smoking causes more than 230,000 deaths from heart and blood vessel disease each year in the United States, Smoking is a major risk factor for getting heart and blood vessel disease. The more you smoke, the greater your risk [17-25]. We show that from our cross sectional study that the results in the volunteers is slightly higher in males than in females. Except with passive smoking, when compared with passive male smokers the female passive smokers may have the higher level due to the method of exposure in passive females more close and contact to smoking inside houses that in males, this will go with studies that prove the risk of exposing to exhale of cigarette smoking. As female passive smokers exposed to smoking per year and per hours per day increased the risk of cardiovascular diseases, any passive smoker expose to smoking more than 25 years and 2 hours per day will be accepted as active smoker for 20 years [16]. According to control groups of females and males (non-smokers) we observe from our study that the female non-smokers have higher risk than that in males, this as we discussed above because the method of exposure in females is more close to smoking inside houses than in males, and this will open a door for more studies about this result and to take the non-smoker females as a profile for Libyan population to be compared with others.
7. Conclusion
Our cross-sectional study suggested that smoking habits according to smoking index considered as a risk factor for cardiovascular system both in active males as well as in passive females.
References
- Athukorala TM, Ranjini LP (1991) Lipid patterns and fibrinogen levels of smokers and non-smokers. Ceylon Med J 36: 98-101.
- Miller GJ, Bauer KA, Cooper JA, Rosenberg RD (1998) Coagulant pathway in cigarette smokers. Thromb Haemost 79: 549-553.
- Stefanadis C, Vlachopoulos C, Tsiamis E, Diamantopoulos L, Toutouzas K, et al. (1998) Unfavourable effects of passive smoking on aortic function in men. Ann Intern Med 128: 426-434.
- Tsekoura D (1998) Fetal nicotine or cocaine exposure: which one is worse? J Pharmacol Exp Ther 285: 931-934.
- James EI (1999) Lung Tumors. In: Richard KA, Stephen GS (eds.) Comprehensive Medicine. Harcourt Brace and Company Limited, New York, pp: 1-24
- Wei Q, Cheng L, Amos CI, Wang LE, Guo Z, et al. (2000) Repair of tobacco carcinogen-induced DNA and lung cancer risk: a molecular epidemiologic study. J Natl Cancer Inst 92: 1764-1772.
- Lundberg JM, Hökfelt T, Martling CR, Saria A, Cuello C (1984) Substance P-immunoreactive sensory nerves in the lower respiratory tract of various mammals including man. Cell Tissue Res 235: 251-261.
- Marting CR, Sorhein LE, Landberg FM (1987) Occurance effects of multiple tackikinnins; substance F, neurokinin A in human lower airways. Life Sci 40: 1633.
- Williams SA, Kwan SY, Parsons S (2000) Williams SA, Kwan SY, Parsons S. Parental Smoking Practices and Caries Experience in Pre-School Children. Caries Research 34: 117-122.
- Kenny PJ, File SE, Neal MJ (2000) Evidence for a complex influence of nicotinic acetylcholine receptors on hippocampal serotonin release. J Neurochem: 2409-2424.
- Dybing E, Sanner T (1999) Passive smoking, sudden infant death syndrome (SIDS) and childhood infections. Human and B Stem villous arteries from placentas of heavy smokers: functional and mechanical properties. Hum Expt Toxicol 18: 202-205.
- Morabia A, Bernstein MS, Bouchardy I, Kurtz J, Morris MA (2000) Breast cancer and active and passive smoking: the role of N-acetyltransferase 2 genotype. Am J Epiderniol 152: 226-232.
- Baker RR, Proctor CJ (1991) The origins and properties of environmental tobacco smoke. Environ Int 16: 23-24.
- Chiba M, Masironi R (1992) Toxic and trace elements in tobacco and tobacco smoke. Bulletin of the World Health Organization 70: 269-227.
- Nitti V, de Michele G, Famiglietti B, Miniccuci E, Ortolani G, et al. (1976) Epidemiological surveof chronic bronchitis in the city of Napels with special reference to the role and possible interaction of various exogenous factors. Bull Int Union Tuberc 51: 685-699.
- Marcus PM, Bergstralh EJ, Zweig MH, Harris A, Offord KP, et al. (2007) Extended lung cancer incidence follow-up in the Mayo Lung Project and overdiagnosis. J Natl Cancer Inst 99: 898-899.
- Gerritsen T, Vaughn JG, Waisman HA (1962) The identification homocystine in the urine. Biochem Biophys Res Commun 9: 493-496.
- Carson NA, Neill DW (1962) Metabolic abnormalities detected in a survey of mentally backward individuals in Northern Ireland. Arch Dis Child 37: 505-513.
- Mudd SH, Finkelstein JD, Irreverre F, Laster L (1964) Homocystinuria: An Enzymatic Defect. Science143: 1443-1445.
- Gibson JB, Carson NA, Neill DW (1964) Pathological Findings in Homocystinuria. J Clin Pathol 17: 427-437.
- Schimke RN, McKusick VA, Huang T, Pollack AD (1965) Homocystinuria. Studies of 20 Families with 38 Affected Members. Jama 193: 711-719.
- Splaver A, Lamas GA, Hennekens CH (2004) Homocysteine and cardiovascular disease: biological mechanisms, observational epidemiology, and the need for randomized trials. Am Heart J 148: 34-40.
- Zetterberg H (2004) Methylene tetrahydrofolate reductase and transcobalamin genetic polymorphisms in human spontaneous abortion: biological and clinical implications. Reprod Biol Endocrinol 2: 7.
- Refsum H, Smith AD, Ueland PM, Nexo E, Clarke R, et al. (2004) Facts and recommendations about total homocysteine determinations: an expert opinion. Clin Chem 50: 3-32.
- Ridker PM, Rifai N, Clearfield M, Downs JR, Weis SE, et al. (2001) Air Force/Texas Coronary Atherosclerosis Prevention Study Investigators Measurement of C-reactive protein for the targeting of statin therapy in the primary prevention of acute coronary events. N Engl J Med 344: 1959-1965.