Information
Journal Policies
Review of Dermatological Problems among the Homeless
Memar Omeed MD PhD1, Bell James R MSN NP-C2, Caughlin Benjamin MD3
2.Los Angeles LGBT Center, Los Angeles, CA.
3Department of Surgery / Division of Otolaryngology, John H. Stroger, Jr. Hospital of Cook County, Chicago, Illinois. Division of Facial Plastic and Reconstructive Surgery, Jesse Brown VAMC, Chicago, Illinois. Division of Facial Plastic and Reconstructive Surgery, University of Illinois Health Hospital System, Chicago, IL. Kovak Cosmetic Center, Oakbrook Terrace, Illinois.
Copyright : © 2018 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
We are experiencing an ever-growing homeless population. Their healthcare needs are not met for multiple reasons, including lack of services and mental health issues prevalent in the population. We have reviewed the literature for reporting on skin disease among the homeless. The most common conditions identified are infectious, with tinea pedis, being the most prevalent. The lower extremities are most commonly affected by skin conditions identified. There is little STD testing among the homeless, especially syphilis. Most alarming is the absence of information on melanoma in this population.
Keywords: Homeless, Skin cancer, tinea pedis, syphilis, Dermatology
1. Introduction
There is a growing number of homeless individuals in the U.S.A., Including sheltered and unsheltered scenarios. 2017 showed the first increase in the number of the homeless since 2009[1]. Their access to healthcare, including dermatologic care is limited[2]. Due to the fact that skin is the most common barrier to the elements, it is logical that the homeless have many skin disorders. Secondly, due to the high prevalence of mental illness[3] amongst the homeless, and the correlation between some skin disorders and mental illness[4] , the homeless present with numerous skin disorders. It is estimated the 20% of emergency room visits by the homeless are skin related[5]. However, in one study, only 24% of the homeless in Los Angeles County reported ever having a skin exam[6]. In this review, we shall present the current data, both national and international, on the dermatologic manifestations in the homeless. We divide the skin problems as diseases with inflammation, Infection/infestation and growths, including cancer.
2. Body Of Article
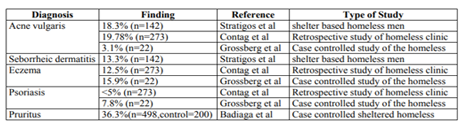
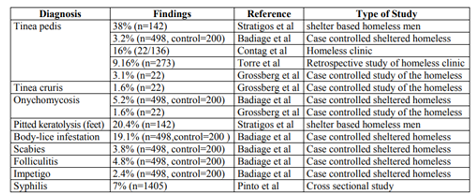
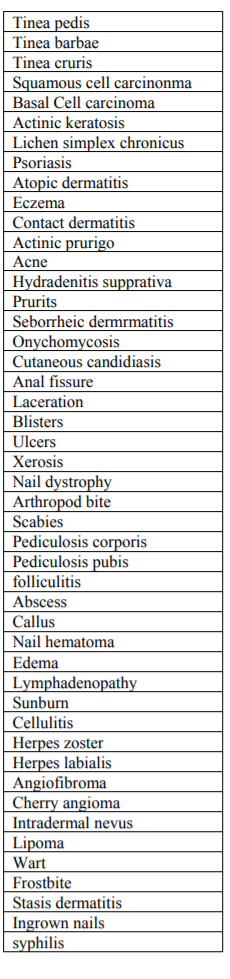
The skin without proper protections is at the mercy of the elements and can be easily traumatized acutely. In one study, 19.7% of shelter-based homeless men had traumatic skin injuries[7]. Frostbite is another serious problem, especially yon the lower extremities[8]. A study of 273 homeless patients revealed that Acne was the most common diagnosis, and 2 patients had lesions suspicious for melanoma[9]. A study at a student-run clinic at the University of California, (UCSF) homeless shelter examined 254 patients, and found that half had dermatologic complaints. Over have did not identify as Caucasian. They found that 45.7% had an infectious/infestation etiology, while 22.2% had Inflammatory skin conditions, with lichen simplex chronicus being the most prevalent. Only 3.7% had growths. However, the one most common diagnosis of the homeless was tinea pedis. The study revealed that the most commonly affected location was the lower extremities, with fungal infections being the main reason[10]. In Brazil, a rapid test for syphilis, revealed 7% out of 1,450 homeless tested positive[11]. Pruritus was found to be the most common skin finding amongst a case control study of sheltered individuals in France[12]. Furthermore, conditions such as pruritus are chronic and effective long-term regimens are not provided due to the lack of continuity of care[13].
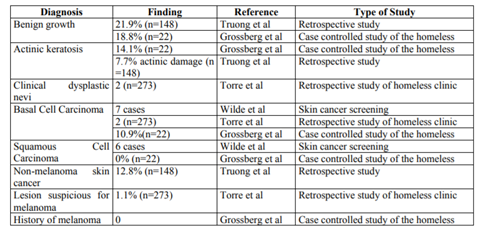
Due to the fact that skin cancer detection requires a full body skin exam, with disrobing, the detection of skin cancer is a challenge in the homeless. Since most melanomas on men are on the back and legs for women, and total skin exam is necessary[14]. In one study, pre-cancers/skin cancers were the most prevalent skin condition, especially amongst the Caucasian population, and did not see a difference in no other skin conditions when compared to a controlled population[15]. Wild et al[16] performed skin cancer screenings at a clinic for the homeless identified 7 basal cell carcinomas per biopsy, and 6 squamous cell carcinomas per biopsy. They found that between 45-50% of the homeless seek out shaded areas, when possible. Truong et al presented a study of 260 skin cancer evaluations on the homeless and found benign growths as the most common finding, followed by non-melanoma skin cancers. No melanoma was reported amongst this population[17].
3. Discussion
In review of the published literature, there seems to be great need for dermatologic care to the homeless. The population data do not corroborate on one particular diagnosis that is most prevalent. However, that might just be due to the differences in homeless populations in different regions. Secondly, if healthcare providers do not have the appropriate tools and skills, like KOH, microscopes, or dermoscopy, along with knowing how to use it, then many diagnoses are missed. Author (JB) spent four years providing basic and dermatologic care as an adult NP to the homeless at Heartlalnd Health Centers in Chicago, IL. The experience brought to life the numbers published in the data.
The extreme stasis ulcers and cellulitis we saw on an almost daily basis was often complicated by uncontrolled diabetes. The challenge was getting patients connected to long-term, ongoing wound care, not only from an insurance standpoint but from a patient compliance standpoint as well. Lack of transportation to specialty appointments, mental illness, and choosing between getting shelter and food versus going to medical appointments (i.e. having to be at shelters at specified times to get a meal or bed).
Scabies and lice were very prevalent. Although patients got therapy, they lacked access to adequate disinfection of for bites, i.e., access to washer and dryers, etc.
Severe abscesses due to injection drug use was an ongoing challenge, since substance rehab services and/or the motivation to utilize them was often limited. The high prevalence of HIV and Hepatitis C resulted in many various skin manifestations[18], including itching. Lack of compliance with HIV treatment regimens and lack of access to HCV treatments complicate therapy[19]. Cutaneous viral infections are prevalent and need adequate diagnosis and treatment[20].
Healthcare Providers who do healthcare for the homeless may not be trained in doing skin biopsies to get accurate diagnoses, detect malignancies, etc. For example, I (JB) was the only Provider at Heartland doing biopsies. Often the wait to get into Dermatology could be several weeks to months at the local Cook County Hospital (Stronger). It proved very helpful to have biopsy results in expediting appointments for skin cancer treatment.
Some medical specialty offices simply were not welcoming to manage homeless patients. For example, one Podiatrist basically thanked me (JB) for the referral but then went on to say she was not "equipped" to take care of homeless patients and not to refer to her in the future. Again, mental illness, disheveled appearance and poor hygiene often marginalize these patients from getting the care they need.
Drug reactions from psych (and other) meds were also frequently seen in Primary Care. There was also a self-esteem component to providing Dermatologic care in the homeless setting. Patients with prominent and sometimes disfiguring lesions on their faces, severe, uncontrolled psoriasis, moderate to severe acne had lowered self-esteem due to their life circumstances. Therefore, depression in the setting of dermatologic disease was harder to treat. Addressing these issues would help boost confidence when patients would have social interactions, including job interviews.
Skin cancer, which is the most common form of cancer in the United States of America is not being detected sufficiently in the homeless and proper treatment, such as Mohs surgery, is not being offered to the homeless[21,22]. In searching Google scholar and PubMed, there were no reported cases of biopsy-confirmed melanoma or dysplastic nevi in any homeless individuals; this is hard to believe. Most likely due to the difficulty of doing a full body skin exam and having the right tools to diagnose. Torre et al presented patients with lesions suspicious for melanoma, but no confirmed melanomas[9].
4. Results
5. Conclusion
There are three takeaway messages from this review. First, the homeless are on their feet, and great many of their skin problems are located on the feet. They need better foot care. Secondly, there needs to be better STD testing, especially for syphilis, but also other STDs, including condylomas. Finally, there is a paucity of total skin exams amongst the homeless. The homeless need skin cancer exams for multiple reasons, including health and reintegration into society.
References
- Henry M, Watt R, Rosenthal L, Shivij A, and Abt Associates. The 2017 annual homelessness assessment report (AHAR) to congress: part 1, point-in-time estimates of homelessness. 2017.
- Kushel, MB, Vittinghoff E, Haas JS. Factors associated with the health care utilization of homeless persons. JAMA.2001; 285:200-2006.
- Folsom DP, Hawthorne W, Lindamer L, Gilmer T, Bailey A, Golshan S, Garcia P, Unützer J, Hough R, Jeste DV. Prevalence and risk factors for homelessness and utilization of mental health services among 10,340 Patients with serious mental illness in a large public mental health system. American J Psychiatry. 2005; 162(2):370-376.
- Attah Johnson FY, Mostaghimi H. Co-morbidity between dermatologic diseases and psychiatric disorders in Papua New Guinea. Int J Dermatol. 1995; 34(4):244-248.
- Romero LS, Broder K, Natsis N, Boder R. Dermatologic conditions in the homeless population. In: Homeless Older Populations: A Practical Guide for the Interdisciplinary Care Team. Edited by Chau D, Gass AP, Springer Publishing Company, 2018. (Book).
- Chau S, Chin M, Chang J, Luecha A, Cheng E, Schlesinger J, Rao V, Huang D, Maxwell AE, Usatine R, Bastani R, Gelberg L. Cancer risk behaviors and screening rates among homeless adults in Los Angeles County. Cancer Epidemiology Biomarkers Prev. 2002; 11:431-438.
- Stratigos AJ, Stern R, González E, Johnson RA, O'Connell J, Dover JS. Prevalence of skin disease in a cohort of shelter-based homeless men. JAAD. 1999; 41:197-202.
- Wrenn K. Foot problems in homeless persons. Annals of Internal Medicine. 1990; 113:567-569.
- Torre K, Shahriari N, Payette M, Murphy M. A retrospective chart review of the most common dermatologic diagnoses at the South Park homeless shelter clinic and efforts to improve access to treatment options: 5697. JAAD. 2017; 76:AB25. DOI: 10.1016/j.jaad.2017.04.115
- Contag C, Lowenstein SE, Jain S, Amerson EH. Survey of symptomatic dermatologic disease in homeless patients at a shelter-based clinic. Our Dermatology Online. 2017; 8:133-137.
- Pinto VM, Tancredi MV, De Alencar HD, Camolesi E, Holcman MM, Grecco JP, Grangeiro A, Grecco ET, Prevalence of syphilis and associated factors in homeless people of Sao Paulo, Brazil, using a Rapid Test. Rev Bras Epidemiol. 2014; 17:341-354.
- Badiaga S, Menard, Dupont HT, Ravaux I, Chouquet D, Graveriau C, Raoult D, Brouqui P. Prevalence of skin infections in sheltered homeless of Marseilles (France). European J Dermatology. 2005; 15:382-386.
- Djalilian HR, Memar O. Topical pimecrolimus 1% for the treatment of pruritic external auditory canals. Laryngoscope. 2006 Oct; 116(10):1809-12. DOI: 10.1097/01.mlg.00002 31562.83733.53.
- Hosler GA, Patterson JW. Lentigines, nevi and melanomas. In: Weedon's Skin Pathology IV edition. Edited by JW Patterson. Elsivir 2016. (book)
- Grossberg AL, Carranza D, Lamp K, Chiu MW, Lee C, Craft N. Dermatologic care in the homeless and underserved populations: observations from the Venice Family Clinic. Cutis 2012; 89:25-32.
- Wilde M, Jones B, Lewis BK, Hull CM. Skin cancer screening in the homeless population. Dermatology Online Journal. 2013; 19:14.
- Truong A, Laggis C, et al. 260 Evaluation of skin cancer diagnoses in dermatology patients seen in a homeless clinic. J Investigative Dermatology. 2018; 138 (suppl):S44. DOI: https://doi.org/10.1016/j.jid. 2018.03.266.
- Memar OM, Rady PL, Tyring SK. Human herpesvirus-8: detection of novel herpesvirus-like DNA sequences in Kaposi's sarcoma and other lesions. J Mol Med (Berl). 1995 Dec; 73(12):603-9. PMID: 8825757.
- Memar O, Cirelli R, Lee P, Tyring SK. Cutaneous manifestations of HIV-1 infection. J Am Podiatr Med Assoc. 1995 Jul; 85(7):362-74. DOI: 10.7547/87507315-85-7-362.
- Memar O, Tyring SK. Cutaneous viral infections. JAAD. 1995 Aug; 33(2 Pt 1):279-87. PMID: 7622657.
- Memar O, Caughlin B. Post-Mohs Reconstruction Methods of a Combination Dermatologist and Facial Plastic Surgeon Practice. Clinical Research in Dermatology. 2018; 1:1-4. DOI: https://doi.org/10.5281/ zenodo.14 70684.
- Memar O, Caughlin B. Reconstructive Methods on Different Parts of the Periocular Region after Mohs Micrographic Surgery in a Combination of Dermatologist and Facial Plastic Surgeon Practice. Clinical Research in Dermatology. 2018; 1:1-4. DOI: https://doi.org/ 10.5281/zenodo.1470677.