Information
Journal Policies
ARC Journal of Dermatology
Volume-1 Issue-1, 2016, Page No: 18-19
Vulval Lichen Sclerosus Associated with Vitiligo
Rosa Giménez-García; Javier Cortejoso Hernandez
Department of Dermatology, Hospital Rio Hortega, Calle Dulzaina 2, 47012 Valladolid, Spain.
Citation : Rosa GG, Javier CH. Vulval Lichen Sclerosus Associated with Vitiligo. ARC Journal of Dermatology. 2016;1(1):18–19. DOI: dx.doi.org/10.20431/2456-0022.0101004
Copyright : © 2016 Rosa GG. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Vulvar Lichen Sclerosus; Vitiligo; Vulvar Squamous, Carcinoma
1.Introduction
Lichen sclerosus (LS) is an autoimmune, chronic inflammatory dermatosis with predilection for localized involvement of anogenital skin. Several lines of evidence support the hypothesis of an autoimmune basis for LS like a frequent association with autoimmune disorders. [1] We describe a 71 year-old patient with genital LS associated with vitiligo.
2.Case Report
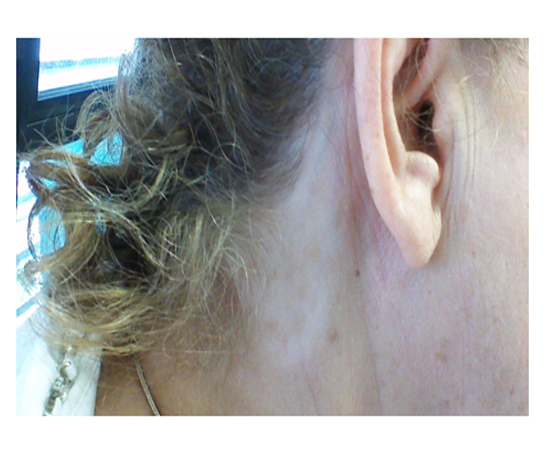
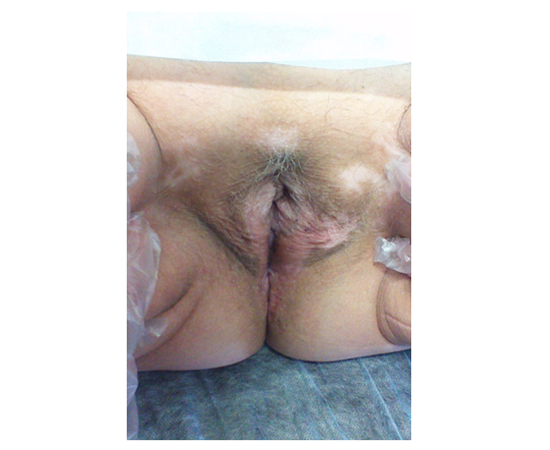
A 71-year-old woman presented to us with a 2 years history of genital pruritus. She had family history of vitiligo and thyroid disease, and personal history of vitiligo diagnosed 10 years ago. On physical examination the patient had depigmented macules on her left axillae, on her neck Figure 1)and on the pubic area consistent with vitiligo. Examination of the genital region revealed vitiligo patches on the pubis and scleroatrophic lesions on the vulva and perianal area (Figure 2). Histopathological study of a skin biopsy showed hyperkeratosis with parakeratosis, focal vacuolization of the basal layerand a dermal lichenoid infiltrate that was compatible with lichen sclerosus. Laboratory test including thyroid-stimulating hormone and autoantibodies were negative. She has been treated with pimecrolimus cream applied 2- 3 times per week.
3.Discussion
The pathogenesis of LSA is thought to be a combination of environment and genetic factors. LS has a clear female preponderance and has two peak ages of presentation, in the prepuberal girls and boys and postmenopausal women and adult men [1]. Association of LS with autoimmune diseases, especially thyroid disease, alopecia areata, morphea and pernicious anaemia, have been found [1,3]. In women, lichen sclerosus was significantly more often associated autoimmune thyroid disease,antithyroid-antibodes and elevated autoantibodies as compared to men. [2]
Vitiligo, a chronic systemic disease that mainly affects melanocytes from epidermis basal layer leading to achromic or hypochromic patches, and LS have been reported to be highly associated with autoimmune diseases and can co-occur [4].However Attili et al [5] reviewed 266 vitiligo cases and did not find association with LS . They suggest that association of vitiligo and LS may have been documented due to the clinical misdiagnosis of vitiligoid LS lesions as vitiligo.Several mechanisms of hypopigmentation in LSA have been proposed as decreased melanin production, block in transfer of melanosomes to keratinocytes and melanocyte loss. Melanocyte loss, as consequence of a lichenoid dermatitis triggering an autoimmune reaction to melanocytes, has been proposed as pathogenic connection of documented association of LS with vitiligo
The risk of malignancy in LS is small but if it occurs it tends to develop rapidly. Squamous cell carcinoma, and less commonly melanoma, basal cell carcinoma has been reported predominantly in patients with vulval LS [1].
4.Conclusion
Patients with LS, especially women with LS,should be screened for other autoimmune diseases. Vitiligo must be differentiated from vitiligoid LS. Long-term follow-up is appropriate for patients with vulval LS.
References
- Zhuang K, Ran Y, Xu F, Lama J.AtypicalinfantilegenitalMolluscumcontagiosum.An Bras Dermatol . 2015;90:403-5.
- Cardoso T, Almeida M, Friedman ND, Aragão I, Costa-Pereira A, SarmentoAE,et al.Classification of healthcare-associated infection: a systematicreview 10 yearsafterthefirst proposal.BMC Med. 2014;12:40
- Choong KY,Roberts LJ. Molluscumcontagiosum, swimmingandbathing: a clinicalanalysis. Australas J Dermatol.1999;40:89-92.
- Beard MA, Mclntyre A, Rountree PM. Sphygmomanometers as a reservoir of pathogenicbacteria Med J Aust.1969;2:758-60.
- LucianaMolina. RicardoRomit. Molluscumcontagiosum on tattoo.An BrasDermatol. 2011; 86:352-4.
- Strauss S, Sastry P, Sonnex C, Edwards S, Gray J.Contamination of environmental surfaces by genital humanpapilloma viruses.SexTransmInfect. 2002;78:135-8.
- SStrauss, H Stephen, C Sonnex, and J Gray. Contamination of environmental surfaces by genitalhumanpapilloma viruses (HPV): a followupstudy.SexTransmInfect. 2003; 79:426-7.