Information
Journal Policies
Smiles Preserved: Pediatric Dentistry Made Painless
Dr. Shreshta Sathish
Copyright : © 2018 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Not just pediatric dentists, but general dentists too require patience and calmness while handling children. Pediatric patients become assets to dentists if treated well. The mission in delivering care to our young patients is simple: provide optimal preventive, interceptive, and restorative dental care in a stress-free environment. This is made possible with the advent of lasers in our practice. But like a double edged sword, lasers used without knowledge may cause trouble in treatments too. Thus proper knowledge and handling skills of lasers must be learnt before using lasers.
Keywords: Smiles Preserved, Pediatric Dentistry, Made Painless,Dental Science
1. Introduction
The mission in delivering care to our young patients is a simple though: optimal preventive, restorative and interceptive dental care in a stress-free environment. This has become a dream come true with the introduction of lasers into our day to day practice. Painless dentistry is now the new hashtag and is the most attractive feature for pediatric patients. Treating children with love, care and compassion in a painless environment, makes then more confident and cooperative. The American Academy of Pediatric Dentistry in 2013, validated the judicious use of lasers as a beneficial tool in providing dental restorative and soft-tissue procedures for infants, children, and adolescents — including those with special health care needs[8].
The concept of light amplification by stimulated emission of radiation (LASER) was first introduced by Albert Einstein 1916[12]. Towens proposed the concept of MASER, an acronym coined for microwave amplification by stimulated emission of radiation. Gordon Gould in 1957 used the term LASER for the first time. The use of lasers in dentistry has been evolved since 1960’s by Maiman. Advantages attributed to lasers include: targeted ablation, hemostasis,analgesia, decontamination, and photobiomodulation[1].
2. Laser Basics[2]
‘LASER’ is an acronym for Light Amplification by Stimulated Emission of Radiation. Within a laser, an active medium is stimulated to produce photons of energy that are delivered in a beam of monochromatic light of a specific wavelength. Wavelengths in the range of 193 – 10,600 nanometers (nm) are applicable in medicine and dentistry.
3. Properties Of Laser Light
This refers to the beam having specific spatial boundaries which ensures that there is a constant beam size and shape that is emitted from the laser unit.
A unique property of lasers that states that they have identical frequency and identical wavelength.
The property of lasers that it possess one specific color which is finely focused.
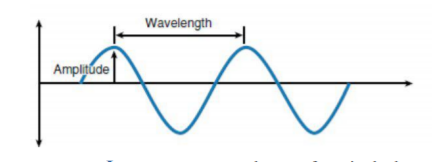
There are three measurements that can define the wave of photons produced by laser-.
a. Velocity
b. Amplitude
c. Wavelength
4. Interaction Between Laser And Matter[15]
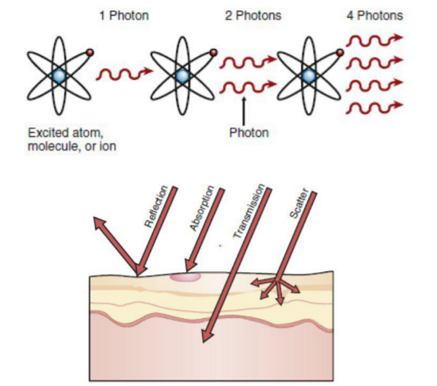
Process indicated by the transfer of an electron from energy level E1 to E2.
Mechanism for reciprocal electronic transition E2 to E1, which is the result of typical radiative decay of excited electronic states of atoms or molecules.
Represents decay mechanism that can occur only if a photon interacts with an atom in the excited state causing emission of a second, identical photon.
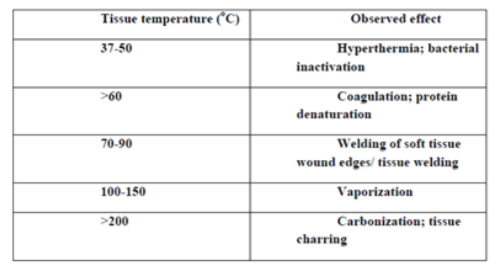
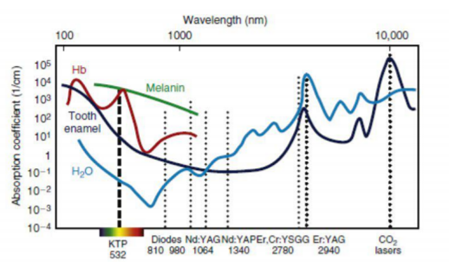
Different laser wavelengths have different absorption coefficient, with the primary oral tissue components of water, pigment, blood contents and minerals. The primary components are termed chromophores, which are absorbers of specific laser energy.
Laser-supported dental diagnosis and treatment, which allows us to meet the important aim of “filling without drilling,” is an excellent approach from the tissue preservation point of view and, as reported by Martens and reiterated by Gutknecht, “children are the first in line to receive dental laser treatment[9]. The main principle in the application of laser is the use of light energy instead of rotation forces and sharp blades. It is also possible to remove caries without anesthesia or with less local anesthesia. Therefore, the dangers of lips and tongue bites which are frequent problems with children can be avoided[14].
Laser fluorescence (LF) can be used as an additional tool combined along with conventional methods for detection of occlusal caries in cases of questionable findings with visual examination. The portable diode laser system interprets the emitted fluorescence on the occlusal surface, which is then correlated with the extent of demineralization in the tooth. Laser digitalized readings indicate the proportional amount of caries present. LF caries detection is not recommended under dental resins or sealants due to a high probability of unreliable readings as a result of the intrinsic fluorescence from the sealant material.
Various mechanisms which suggest caries prevention by lasers are:
1. Increased acid resistance in lased enamel by ultrastructural alterations of enamel, as a result of melting and resolidifying.
2. Organic blocking theory: the partial denaturation of organic matrix may block the diffusion pathway in enamel, resulting in retardation of enamel demineralization.
3. Combination of reduced enamel permeability and enamel solubility as suggested by Stern et al.
4. Laser can alter the chemical composition and morphology of the highly mineralized (96%) dental enamel.
1. Accessory treatment by laser for indirect pulp capping
The discovery of closure of dentinal tubule by laser energy and the sedative effect on pulpitis has led to the development of indirect pulp capping of carious teeth.
2. Direct pulp capping
When using the CO2 laser for this treatment, laser irradiation of the exposed dental pulp must be performed to stop bleeding and sterilize the area around the exposure.
3. Laser pulpotomy of primary teeth
In vital teeth, the laser cleans the pulp chamber in 10-20 s. The laser seems to provide adequate hemostasis and allows some vital tissue to remain at the apex. In non-vital teeth, the laser’s success rates seem equal to conventional pulpotomy procedures.
The treatment involves low power settings, and the laser energy is directed at the target tissue in a noncontact fashion. The involved area is lased in 15-30 s intervals, no local anesthesia is used and the procedure is repeated three or four times until the patient reports relief. The tissue may appear drier at the end of the treatment, without much change in color.
It is not uncommon for children whose first permanent molars are erupting to develop discomfort, swelling, or infection in the tissue overlying the emerging tooth. Lasers can be used in a noncontact mode to ablate the involved tissue and expose clinical crown of the involved tooth.
Gingival hyperplasia related to orthodontis are treated effectively with diode and erbium lasers.
1. Apexogenesis[6]
2. Labial frenectomy[11]
3. Tongue tie removal
Er: YAG laser can be used for frenectomy in infants with tight maxillary frenums or for upper and lower frenectomy in infants with severe ankyloglossia.
Laser doppler flowmetry (LDF) indicates the pulp blood flow (PBF) and can be used to assess pulp vitality. This method is accurate, noninvasive, reproducible, reliable and painless and is well tolerated by children. It appears that LDF can also be helpful for monitoring of revascularization and mobile teeth.
Laser irradiation can be used for preservation of pulp vitality. Different wavelengths with 0.5-1 W power, non-concentrated beam, low frequency and pulse mode without water and for durations less than 10 seconds (in order not to cause coagulation) and with 30-second intervals (to prevent over-heating of the pulp) can be useful for this purpose.
Dentinal tubules in primary teeth are anatomically larger in diameter than those found in secondary teeth. Therefore carious dentine in primary teeth will have a faster rate of ablation, which must be taken into consideration when the laser energy parameters are selected for the procedure.
Laser increases the pain threshold of patients and decreases the need for local anesthetics.when used in non concentrated mode, diode laser provides 15mts of pulpal analgesia.
5. Conclusion
The use of lasers in pediatric patients renders safe, painless and children friendly dental treatments. Both hard tissue and soft tissue applications are seen.
References
- Coluzzi, D. and Parker, S. (n.d.). Lasers in Dentistry—Current Concepts.
- Convissar, R. (2011). Principles and practice of laser dentistry. St. Louis, Mo.: Mosby Elsevier.
- Mahitab M Soliman., et al. “Lasers Use in Different Dental Pediatric Aspects”. EC Dental Science 17.3 (2018): 150-159.
- Fatima T. Lasers in Pediatric Dentistry. J Adv Med Dent Scie Res 2015; 3(3):59-64.
- I. E. Neena, P. Poornima, Ganesh Edagunji, K. B. Roopa, K. P. Bharath, “Lasers in pediatric dentistry: A review,” Int J Contemp Dent Med Rev, Vol. 2015, Article ID: 030115, 2015.
- Sharma, m. (2016). Diode Laser Applications in Pediatric dentistry. Journal of applied dental and medical sciences, 2(1).
- Nazemisalman, B., Farsadeghi, M. and Sokhansanj, M. (2015). Types of Lasers and Their Applications in Pediatric Dentistry. Journal of lasers in medical sciences, 6(3), pp.96-101.
- Aapd.org. 2018 [cited 30 June 2018]. Available from: http://www.aapd.org/media/Policies_Guideline s/ P_LasersUse.pdf
- Kotlow L. Lasers in pediatric dentistry. Dental Clinics of North America. 2004; 48(4):889-922.
- Mulder R, Melman G, Karic V. Lasers in Paediatric Dentistry. SADJ. 2016; 71(9):421.
- Martinez Menchaca H, Rivera Silva G. Lasers in Pediatric Dentistry. OHDM. 2015; 14(6).
- Prathima G. Microdentistry with Lasers. Journal of International Oral Health. 2015; 7(9):134-137.
- KOTLOW L. Lasers and Soft Tissue Treatments for the Pediatric Dental Patient. Alpha Omegan. 2008; 101(3):140-151.
- LASER IN PEDIATRIC DENTISTRY. World Journal of Pharmacy and Pharmaceutical Sciences. 2017; 6(10):224-232.
- Martens L. Laser physics and a review of laser applications in dentistry for children. European Archives of Paediatric Dentistry. 2011; 12(2):61-67.