Information
Journal Policies
Ectodermal Dysplasia with Uncommon Diabetes Ketoacidosis as First Presentation of Apoplectic GH Secreting Macroadenoma
Dr. Manel Jemel1*, Dr. Mariem Riahi1, Hana Ben Haj Hassen1, Dr. Hajeur Kandara1, Pr. Sonia Neji2, Dr. Ines Kammoun1
2.National Institute of Neurology, University of Tunis El Manar Tunis, Tunisia.
Copyright : © 2018 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Ectodermal dysplasia (EDs) are a heterogeneous group of disorders characterized by developmental dystrophies of one or more ectodermal derivatives such as hair, nails, teeth, skin, and sweat glands. Hypohidrotic, or anhidrotic, ectodermal dysplasia are the two major forms characterized by a triad of signs comprising sparse hair (hypotrichosis), abnormal or missing teeth (anodontia or hypodontia), and inability to sweat (anhidrosis or hypohidrosis). The cardinal features of this syndrome can be associated to some facial traits including prominent forehead, thick lips, and flattened bridge of the nose. These facial features overlaps with dysmorphic syndrome of acromegaly. Moreover, even pituitary gland is entirely ectodermal in origin; few cases have reported an association between hypothalamic pituitary disorder and (EDs). The main disorder described was hypothalamo−pituitary insufficiency resulting the defects of hypothalamic and pituitary developmental. We report in this paper a case of a men presenting features of hypohidrotic ectodermal dysplasia, who was admitted to our institute with Diabetes Ketoacidosis as the first presentation of a spontaneous remission of acromegaly after pituitary apoplexy.
Ectodermal Dysplasia, Diabetes Ketoacidosis, Apoplectic GH, Secreting Macroadenoma,Clinical Case Reports
1. Introduction
Ectodermal dysplasia (EDs) results from the abnormal development of embryonic ectodermal structures. Thus, it affects the development of keratinocytes and causes aberrations in the hair, sebaceous glands, eccrine and apocrine glands, nails, teeth, lenses and conjunctiva of the eyes, anterior pituitary gland, nipples, and the ears [1,2].
They are relatively rare and occur with a frequency varying between 1:10,000 and 1:100,000 live births [3]. More than one hundred and seventy different varieties of these clinical conditions have been recognized [4]. Individuals affected have abnormalities in different ectodermal structures and some types of EDs are mild. Developmental hypothalamic pituitary defects was suggested to be involved by this pathology but commonly lead to pituitary insufficiency reported in some forms [5,6].
Nevertheless, here we present an exceptional association of ED with GH secreting macroadenoma.
2. Patient And Observation
A 27 years old men presented to our emergency department with a new onset diabetes with moderate DKA. After three days he was referred to our department for evaluation of his diabetes mellitus. He had a recent history of polyuria, polydipsia, and weight loss. He reported no regular medications, no family history of diabetes, and no history of autoimmune diseases.
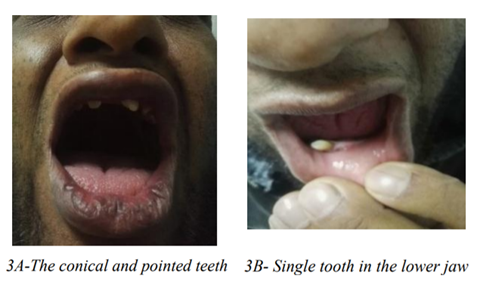
On questioning he reported that he has continuous fronto-orbital headache during the past 5 years, with a sudden episode of increased cephalalgia concomitant to the ketoacidosis episode. The clinical examination acromegaly was suspected based on prognathism, macroglossia, enlargement of the forehead, thickened lips (figure 1) and enlarged hands (figure 2). He agreed to have noticed an increasing shoes size. Moreover on clinical examination we noted a partial edentulism with a single tooth erupted in the lower jaw which was since his childhood (figure 3A and 3B). Lips were reverted. He had sparse, thin, lightly pigmented scalp hair. There was periorbital hyperpigmentation (figure 1). When asked about a similar history in the family patient gave a positive history of his nieces (brother’s daughters) suffering from a similar complaint of edentulism. These findings matched typical features of anhidrotic ectodermal dysplasia.
Investigations on admission included blood glucose of 19 mmol/l, glycosuria, and 2+ ketonuria on urinalysis it, A1cHb: 11%; a series of plasma GH showed a nadir at 0.8 ng/ml, IGF-1:275.8 (ng/ml) (reference range 82-241), adrenocorticotropic insufficiency and hypogonadotrophic hypogonadism.
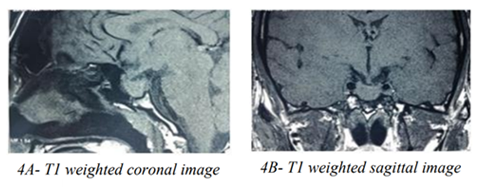
Pituitary MRI: showed a necrotic pituitary macroadenoma (10x16x16mm), enlarged sellaturcica, intrasellararachnoidocele, deviation of the left pituitary stalk and optic chiasm ptosis. (figures 4A and 4B). Which was suggestive of pituitary apoplexy.
Our patient received, hydrocortisone: 15 mg daily and basal insulin therapy. When seen three month later he reported that he had withdraw her insulin treatment because of intermittent episode of hypoglycemia. Spontaneous glycemia was: 5,6 mmo/l, A1cHb: 7%. IGF1: 100 ng/ml.
Owing to the clinical features, hormonal investigations, radiologic findings and the evolution we retain the diagnosis of a spontaneous remission of acromegaly after a pituitary apoplexy of a macroadenoma.
3. Discussion
EDs have two main forms: (A) hypohidrotic form/Christ-Siemens-Tourian syndrome which exhibits the classic triad-hypohidrosis, hypotrichosis, and hypodontia. (B) Hidrotic form/Clouston syndrome exhibits hair, nail defect, and spare sweat glands abnormality [2]. Hypohidrotic form is usually, X-linked recessive inheritance thus; males are affected severely, while females show only minor defects.
The presentation of our patient: characteristic faces associated to hypotrichosis, hypodontia with peg-shaped incisors, is in agreement with existing literature, which confirm the diagnosis of hereditary hypohydrotic ectodermal dysplasia. The family history of his nieces (brother’s daughters) suffering from an edentulism is another argument of our hypothesis.
After careful perusal of literature, few cases are reported, and they commonly focused on dental defect [7].
Even pituitary gland is entirely ectodermal in origin few cases have reported an association between hypothalamic pituitary disorder and (EDs). The main disorder described was hypothalamo−pituitary insufficiency as consequence of hypothalamic and pituitary developmental defects in patients affected by Ectrodactyly−ectodermal dysplasia−clefting (EEC) syndrome [5].
This syndrome is a rare form of ectodermal dysplasia symptoms can vary from mild to severe and most commonly include missing or irregular fingers and/or toes (ectrodactyly or split hand/foot malformation); abnormalities of the hair and glands; cleft lip and/or palate; distinctive facial features; and abnormalities of the eyes and urinary tract [6].
The first exclusivity of our case is the association of GH macroadenomawich is not previously described in the ectodermal dysplasia which paradoxalement is associated to pituitary defect.
On the other hand, diabetic ketoacidosis is have been anecdotally reported as the first presentation of acromegaly [8,9].
The mechanisms for DKA in acromegaly include an excess of growth hormone, which counteracts the action of insulin to stimulate lipolysis and promote triglyceride hydrolysis into free fatty acids [10]. Moreover the increase in IGF-l levels, which increases insulin resistance results in reduced lipoprotein lipase activity, reduced catabolism of very-low- density lipoproteins, increasing lipolysis of adipose, and increasing fatty acid influx to the liver [11]. Glucagon has also been considered as a possible contributing factor to DKA and may be increased in acromegaly [12].
Moreover, pituitary apoplexy wich is defined as pituitary hemorrhage occurring spontaneously in a preexisting pituitary is a rare but life-threatening event owing to complications including severe headache, risk of vision loss, and endocrine crisis due to adrenal insufficiency [13].
It can be precipitated by many risk factors such as hypertension, medications, major surgeries, coagulopathies, dynamic testing of the pituitary, or pregnancy. Diabetes ketoacidosis has been described as precipitating factor of this event [14].
The pituitary adenomas prone to apoplexy are non functioning, macroprolactinemia and GH secreting adenoma. Several published series reported clinical and biochemical resolution of hormonally GH pituitary adenomas following pituitary apoplexy on follow-up [15,16].
The clinical features of our patient were very suggestive of acromegaly but the GH and IGF1 were slightly above the normal range. In light of MRI funding, a remission of GH macroadenoma is the final diagnosis.
The question is whether the ectodermal dysplasia can be involved in the infraction pathogenesis of the macroadenoma as a result of the fragility of the relative defect of the pituitary, or the apoplexy was precipitate by DKA.
4. Conclusions
This is an atypical case with KAD as the first presentation of an apoplectic growth hormone pituitary adenoma and remission of acromegaly associated with ectodermal dysplasia.
Prompt recognition of acromegaly can be challenging in some cases because of the insidious symptoms, which can overlap with other pathologies. The possibility of a secondary diabetes should draw the attention of the clinician even in the context of DKA. Early identification of an underlying cause will ensure that prompt and appropriate investigation and medical management.
References
- Itthagarun A, King NM. Ectodermal dysplasia: A review and case report. Quintessence Int 1997; 28:595-602.
- Vaidya S, Risbud M, Kshar A, Ramdurg P. Hereditary ectodermal dysplasia: Report of 11 patients from a family. Indian J Dent Res 2013; 24:502-6.
- Ammanagi R, Keluskar V, Bagewadi A. Ectodermal dysplasia: Report and analysis of eleven South Indian patients with review of literature. J Indian Acad Oral Med Radiol2010; 22:93-8.
- Priolo M, Laganà C. Ectodermal dysplasias: A new clinical-genetic classification. J Med Genet 2001; 38:579-85.
- Gershoni−Baruch R, Goldscher D, Hochberg Z. Ectrodactyly−ectodermaldysplasia−clefting syndrome and hypothalamo−pituitary insufficiency. Am J Med Genet. 1997; 68:168– 172.
- NihalHatipoğlu, SelimKurtoğlu, Derya Büyükayhan, and Mustafa Akçakuş Hypo- thalamo−Pituitary Insufficiency Associated with Ectrodactyly−Ectodermal Dysplasia −Clefting Syndrome J Clin Res Pediatr Endocrinol. 2009; 1(5): 252–255.
- Singh G, Kapoor A, Sharma V, Mukesh D. Ectodermal dysplasia: A case report. Indian J Stomatol 2012; 3:187-9
- He-Jiun Jiang Wei-Wen Hung Pi-Jung Hsiao. A case of acromegaly complicated with diabetic ketoacidosis,pituitaryapoplexy,and lymphoma. Kaohsiung J Med Sci. 2013; 29(12):687-90.
- Rupal V Dosi, Rushad D Patell, Pratik J Shah, and Harshal K Joshi. Diabetic ketoacidosis: an unusual presentation of acromegaly. BMJ Case Rep. 2013; 11: 2013. Pii
- A. Vijayakumar, R. Novosyadlyy, Y. Wu, S. Y akar, D. LeRoithBiological effects of growth hormone on carbohydrate and lipid metabolism. Growth Horm IGF Res. 2010; 20: 1-7
- Lebovitz HE. Hyperglycemia secondary to non diabetes condition and therapies. In: DeGroot LJ, ed. Endocrinology. 5th edn. Vol 1. Elsevier Saunders Company, 2006:1122.
- Lisa R. Simmons, BSc, MBBS (Hons), MPhil, FRACP, Kiernan Hughes, MBBS, MSc, FRACP, Tania P. Markovic, MBBS, FRACP, PhD, and Elizabeth L. Chua, MBBS, FRACP, PhD. Diabetic Ketoacidosis as a Presenting Feature of Acromegaly: When Excess Hormone Meets Hormone Deficiency. Clinical Diabetes 2012 Oct; 30(4): 170-172
- M. Turgut, Y. Ozsunar, S. Basak, E. Guney, E. Kir, I. Meteoglu Pituitary apoplexy: an overview of 186 cases published during the last century. ActaNeurochir (Wien), 152 (2010), pp. 749-761
- Biousse V, Newman NJ, Oyesiku. Precipitating factors in pituitary apoplexy. J Neurol Neurosurg Psychiatry. 2001; 71: 542–5.
- Cinar N, Metin Y, Dagdelen S, ZiyalSelcuk M. I, Soylemezoglu F, Erbas T. Spontaneous remission of acromegaly after infarctive apoplexy with a possible relation to MRI and diabetes mellitus. Neuro Endocrinol Lett 2013; 34:339–42.
- Fraser LA, Lee D, Cooper P, Van Uum S. Remission of acromegaly after pituitary apoplexy: case report and review of literature. EndocrPract2009; 15:725–31.