Information
Journal Policies
Pericarditis: Uncommon Onset of Anti-Neutrophil Cytoplasmic
Antibody-Associated Vasculitis Induced by Methimazol
Manel Jemel1,2*, HanenSayadi3, Ines Khochtali4
2.Manar Tunis University.
3.Fattouma Bourguiba University Hospital, department of Endocrinology, Monastir, Tunisia.
4.FattoumaBourguiba University Hospital, department of Endocrinology, Monastir, Tunisia.
Copyright : © 2018 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Anti-neutrophil cytoplasmic antibodies (ANCA)-associated vasculitis (AAV) can be induced by antithyroid drugs (ATDs). It is more commonly associated with propylthiouracil (PTU) but remains misdiagnosed. The cardiac involvement is uncommon. Case report: we report a case of 25-year-old women who had a history of Graves’ disease treated by Methimazole (MMI) 20 mg daily during one year. She was admitted because of pericardial effusion. Two days after, necrotic-looking vasculitic skin lesions appeared. Anti-neutrophil cytoplasmic antibodies (ANCA)-associated vasculitis (AAV) was confirmed by serum test and skin biopsy. The MMI was suspected to be the culprit and was immediately withdrawn. She progressively improves her symptoms, and her skin lesions and pericardial effusion were resolved. Conclusion: This is the first case report of pericarditis as the first sign AAV induced by Methimazole. The withdrawal of the offending medication is the fundamental pillar of the therapeutic approach to avoid more severe complications.
anti-thyroid drug, Methimazole, vasculitis, Anca, pericarditis,Clinical Case Reports
1. Introduction
Anti-neutrophil cytoplasmic antibodies (ANCA)-associated vasculitis (AAV) is a group of small vessel vasculitides characterized by necrotizing inflammation, with few or no immune deposits associated with myeloperoxidase (MPO) ANCA or proteinase 3 (PR3) ANCA. It includes microscopic polyangiitis, granulomatosis with polyangiitis (Wegner’s), eosinophi lic granulomatosis with polyangiitis (Churg-Strauss) and single-organ AAV (for renal example, renal-limited AAV)[1]. Even the etiology of this vasculitis is still unclear several factors have been reported to be associated with AAV with more consideration of drug-associated ANCA-associated vasculitis [2]. Antithyroid drugs (ATDs) which are generally well tolerated can be associated with minor side effect, but serious and potentially life-threatening complications can occurred in very rare cases with such AAV [3]. To date Propylthiouracil (PTU) is more likely to be associated with AAV than Carbimazole (CBZ) or his active metabolite Methimazole (MMI) [4]. Skin lesions and kidney involvement are the most common clinical features reported in this field. Here we present the first case report of a 25-yr-old woman who developed AAV initially presenting with pericarditis after 1 year of MMI use.
2. Case Study
A 25-yr-old woman was admitted with a recent history of precordial pain and dyspnea. Graves ' hyperthyroidism was diagnosed 1 year before; she was clinically euthyroid on Methimazole (MMI) 20 mg daily. In the two weeks prior to admission, she reported progressive weakness followed by fever. The examination revealed blood pressure of 120/60 mm Hg. Rhythmic cardiac sounds with pericardial rub, and no edema. The analysis showed TSH: 1, 9 mUI/l, free T4: 13ng/l haemoglobin levels of 11.7mg/dl, GFR (MDRD) > 60 ml/min/1.73m, and systemic/urine sediment showed no abnormalities. The chest radiography showed severe cardiomegaly. An emergency echocardiography showed a moderate-to-severe pericardial effusion. The ECG was normal. Direct Coombs test was negative, haptoglobin was 4g/l, LDH 370U/l, C3 and C4 within the normal range, ANA was negative, ANCA was positive (1/300), with a p-ANCA pattern. Cryoglobulinemia was negative. Treatment was started with doses of steroids at 1mg/kg/day, and the patient’s state start to improve considerably.
Two days after her admission, necrotic-looking vasculitic skin lesions were revealed and progressively extended on bilateral lower extremity and on her right ear. (Figure 1)
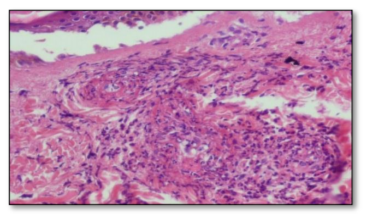
The MMI induced vascularitis was suspected, so we stopped the offending treatment. Skin biopsy was performed and showed leukocytoclastic vasculitis. (Figure 2).
In her follow up, the skin lesion disappeared progressively. (Figure 3)
Echocardiography was repeated after 7 days of steroid administration, revealed no signs of pericardial effusion. In the light of above clinical and laboratory findings she was diagnosed to have leukocytoclastic vasculitis caused by MMI, with positive p-ANCA. Our patient underwent an I131 iodine ablation therapy.
3. Discussion
Thiamazole (Methimazole) and Benzylthiouracil are the antithyroid drugs (ATDs) which are the most commonly used as first-line therapy in the treatment of thyrotoxicosis due to Grave’s disease and toxic nodular goiter in Tunisia.
These drugs are associated up to 15% to minor side effect such as cutaneous reactions (usually urticaria or macular rashes), arthralgia, and gastrointestinal upset. However, serious and potentially life-threatening complications can occurred in very rare cases such as agranulocytosis, and Anti- neutrophil cytoplasmic antibody-associated vasculitis (ANCA-associated vasculitis)[3]. It was first described with PTU [5] and up to now more than 260 cases have been published with higher incidence of PTU induced AAV than MMI with an average incidence of 6.5 patients per year versus 0.8 patients per year respectively [6].
A recent case report study reported the occurrence of AAV as soon as a woman with Graves' disease, who wished to become pregnant, was switched from MMI to PTU [7]. Many studies report that there is a high prevalence of MPO- ANCA in patients treated with PTU compared with patients treated with MMI but less than 1 of 6 ANCA-positive patients treated with ATDs developed AAV. In fact in recent review the AAV risk of AAV was estimated to occur in about 3% [4]. Moreover, ANCAs was detected in patient with Grave’s disease even without exposition to the ATDs [8].
Although the pathogenic role of ANCA is, still controversial but cumulative evidence from in vivo, in vitro and clinical studies supports the involvement of ANCAs in the pathogenesis of AAV [9-11]. The ANCAs represent the serological hallmarks for this entity. Two patterns of ANCAs can be found: a cytoplasmic staining pattern (cANCA) with PR3 as target antigen, and a perinuclear staining pattern (pANCA) having (MPO) as the most important target antigen [12].
Several hypotheses have been proposed to explain the association of AAV with the PTU use. It was postulated that there is an interaction between MPO, the major antigen of ANCA, and PTU. PTU could bind to myeloperoxidase, and alters its structure and function, leading to formation of autoantibodies in susceptible individuals [13]. There are no published data suggesting that Methimazolee can also alter the configuration and the function of myeloperoxidase leading to the vascular injury. Zhang et al [14] postulate that activated neutrophils lead to a higher amounts of myeloperoxidase which oxidize the PTU into reactive oxide species. Then these substances activate immunocompetent cells resulting in paucity of immune deposits and the production of MPO-ANCA causing vascular injury.
The clinical manifestation can vary from nonspecific constitutional symptoms, such as fever, fatigue, flu like syndrome, arthralgia, to multisystem disease with organ-threatening or even life-threatening disease, including acute kidney injury and severe pulmonary hemorrhage.73 The kidney involvement is the most described in the literature followed by the skin and then skin and respiratory track.
The prevalence of these various presentations is similar to that occur in primary vasculitis but less severe. Cardiac involvement is uncommon in drug-indced AAV[11]. The median time of onset AAV caused by ATD was reported to be an average of 42 months (range, 1–372 months) after starting drug treatment [11].
As a primary manifestation of the disease, cardiac involvement is more frequent in Churg-Strauss disease [15,16]. The Skin lesions asleukocytoclastic vasculitisare commonly describe in the litterature, and affects preferentially the lower extremities [17].
Our patient has acute pericarditis with flu-like syndrome. Her skin lesion caught our attention and help us in our diagnosis approach. In fact the unusual onset of antithyroid drug-induced AAV as pericardial effusion, in our knowledge, was reported in only one case in 2001by HristoColakovski et al.[18]. But in this case the AAV was induced by PTU, thus our case is the first case report of pericarditis as the first presenting symptom of Methimazole induced AAV.
As soon as antithyroid drug is suspected to be the culprit in ANCA-associated vasculitis it should be discontinued and importantly, this has a good prognosis, as it was in our case. The unawareness of this uncommon adverse reaction of ATDs can cause the occurrence of potentially life-threatening complications.
4. Conclusions
The importance of this case is to call attention to the possible occurrence of pericarditis as a first symptom of ant thyroid drug-induced AAV. Even the PTU is more often incriminated than the Methimazole, patients on MMI treatment need a longtime follow up. Proper examination and evaluation of complementary tests is mandatory. The withdrawal of the offending medication is the fundamental pillar of the therapeutic approach in this field to avoid more severe complications.
References
- Jennette JC, Falk RJ, Bacon PA, Basu N, Cid MC, Ferrario F, et al (2013). 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum. 65:1–11.
- Chen M, Kallenberg CG (2010). The environment, geoepidemiology and ANCA-associated vasculitides. Autoimmun Rev. 9, A293-8.
- David S. Cooper. Antithyroid Drugs, M.D (2005). N Engl J Med, 352, 905-17
- Jacques Orgiazzi (2016). How should We Consider the Risk of Antineutrophil Cytoplasmic Antibody (ANCA) Positive Small-Vessel Vasculitis Associated with Antithyroid Drug Therapy? ClinThyroido, 28, 18–21.
- Stankus SJ, Johnson NT (1992). Propylthiouracil-induced hypersensitivity vasculitis presenting as respiratory failure. Chest, 102, 1595–6.
- Noh JY, Yasuda S, Sato S, Matsumoto M, Kunii Y, Noguchi Y, Mukasa K, Ito K, Ito K, Sugiyama O, et al. (2009). Clinical characteristics of myeloperoxidase antineutrophil cytoplasmic antibody-associated vasculitis caused by antithyroid drugs. J Clin Endocrinol Metab, 94, 2806-11.
- Kimura M, Seki T, Ozawa H, Ishihara T, Komatsu M, Tajiri S et al (2013). The onset of antineutrophil cytoplasmic antibody- associated vasculitisimmediatelyafter Methimazolee was switched to propylthiouracil in a woman with Graves' disease who wished to become pregnant. Endocr J, 60(3), 383-8.
- Gumà M, Salinas I, Reverter JL, Roca J, Valls-Roc M, Juan M, et al (2003). Frequency of antineutrophil cytoplasmic antibody in Graves’ disease patients treated with Methimazolee. J Clin Endocrinol Metab, 88, 2141–2146.
- Xiao H. Hu P. • Falk R.J. (2015). • JennetteJ.C. Overview of the pathogenesis of ANCA associated vasculitis kidney dis, 1, 205-2015.
- Kallenberg CG. Pathogenesis and treatment of ANCA-associated vasculitides. (2015). Clin Exp Rheumatol., 33(Suppl 92), S11–4
- Lazarus B., John G. T., C. O’Callaghan, and RanganathanD (2016). Recent advances in anti-neutrophil cytoplasmic antibody-associated vasculitis.Indian J Nephrol, 26(2), 86–96.
- Jennette, J. C. & Falk, R. J. (1997) Small-vesselvasculitis. N. Engl. J. Med, 337, 1512– 1523.
- Gao Y., Chen M., Ye H., Guo X.-H., Zhao M.-H., Wang H.-Y (2007). The target antigens of antineutrophil cytoplasmic antibodies (ANCA) induced by propylthiouracil. International Immunopharmacology. , 7(1), 55–60.
- Zhang, A. H., Chen, M., Gao, Y., Zhao, M. H. & Wang, H. Y. (2007) Inhibition of oxidation activity of myeloperoxidase (MPO) by propylthiouracil (PTU) and anti-MPO antibodies from patients with PTU-induced vasculitis. Clin. Immunol, 122, 187–193.
- Kane GC, Keogh KA (2009). Involvement of the heart by small and medium vessel vasculitis. Curr Opin Rheumatol, 21, 29-34.
- Keogh KA, Specks U (2003). Churg-Strauss: clinical presentation, antineutrophilic cytoplasmic antibodies and leukotriene receptor antagonist. Am J Med, 115, 284-90.
- Bilu Martin D1, Deng A, Gaspari A, Pearson F. (2006). Perinuclear antineutrophil cytoplasmic antibody-associated vasculitis in a patient with Graves' disease treated with Methimazolee,” Skinmed, 5(6), 302-5.
- HristoColakovski, and Daniel L. Lorber, (2001). Propylthiouracil-induced perinuclear-staining antineutrophil cytoplasmic autoantibody-postive vasculitis in conjunction with pericarditis. Endocrine Practice,7(1), 37-39