Information
Journal Policies
Intestinal Atresia Type III B in Newborn. Case Report
Alicia Santa Cortes Gonzalez1*, Daniel Chan Vazquez2, Veronica Lopez Espinoza3, Fernando Alberto Gonzalez Gomez4
2.Pediatric Surgeon, Service of pediatrics General Hospital of Zone num.11 Mexican Social Security Institute of Xalapa Veracruz, Mexico.
3.Gastroenterologist Pediatrician, Service of pediatrics General Hospital of Zone num.11 Mexican Social Security Institute of Xalapa Veracruz, Mexico.
4.Resident of Pediatrics, Service of pediatrics General Hospital of Zone num.11 Mexican Social Security Institute of Xalapa Veracruz, Mexico.
Copyright : © 2018 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction: Bowel atresia is the most frequent of the obstructive congenital malformations of the digestive tract in newborn children, it is reported in almost a third of the cases of neonatal intestinal obstruction. The world incidence is 2.25 per 10,000 live births, and in Latin America it is 1.3 per 10,000 live births. We present the case of a 2-month-old male with intestinal atresia type III b in Apple peel, with anendosteal / oblique anastomosis with intestinal resection, leaving 10 cm of small intestine with presence of ileocecal valve and colon integrity, its clínical evolution and maintenance with nutritional support, based on parenteral nutrition, amino acid formula by gastrostomy and breast feeding.
Conclusion: The patients with sic are a challenge for the pediatrician, gastroenterologist and pediatric surgeon, nutritionist and nurse, the prognosis is in function to the opportune handling, the length of there section and the nutritional maintenance.
intestinal atresia, short bowels índrome (SBS) parenteral nutrition, anastomosis,Clinical Case Reports
1. Introduction
the obstructive congenital malformations of the digestive tract in newborn children, it is reported in almost a third of the cases of neonatal intestinal obstruction[1]. The world incidence is 2.25 per 10,000 live births, and in Latin America it is 1.3 per 10,000 live births. The incidence varies from 1 in 350-500 live births to 1 in 10,000[2].
It is reported that in 50% of the cases the atresia occurs in the duodenum, 36% in the jejuno-ileal segment and in 7% in the colon; in only 5% of cases, atresia has multiple manifestations[3]. lethality has decreased in recent years, from 36.5% in 1969 to 10% in later revisions is more frequent in preterm infants (35.4%) and in those with low birth weight (52%). Multiple atresias, mortality is 57%, surpassed only by meconium ileus (65%) and gastroschisis (66%)[4].
The short bowel syndrome secondary to surgical resection represents an important and significant management challenge and in the absence of adequate treatment is manifested by chronic diarrhea, malnutrition, weight loss, deficiency of nutrients and electrolytes, as well as failure to grow that occurs more frequently in the neonatal period[5]. Caso clínico.
2. Clinical Case
Male, 2 months old, with a perinatal history of being a product of pregnancy 2 of a healthy 24-year-old mother, I have prenatal control, course of cervicovaginitis in the 7th month of pregnancy, received treatment without complications, obtained by cesarean section at 36 weeks of gestation due to acute and circular fetal distress of cord to neck, qualified with apgar of 8/9 with weight of 2,200 grs (low weight for gestational age) father of 35 years of age carrier of testicular cancer in remission with left orchiectomy, of medium low economic partner, enters in a binomial with the mother to joint housing after his birth being released to the second day at home.
He is fed to the maternal breast from birth, on the third day of life he enters the pediatric emergency department for vomiting at all ingestion, absence of stools since birth, jaundice and oliguria with poor general condition with severe dehydration in hypovolemic shock, laboratory tests are taken with a report of 17.6 g / dl hto 52% platelets 371,000 leukocytes 11.5 10 / UL neutrophils 64%, glucose 71 mg / dl urea 105.5mg / dl creatinine 4.1 mg / dl total bilirubin 23.6 mgdl direct bilirubin 0.7 mg / dl indirect bilirubin 22.9 mg / dl ALT 8 ui / dl AST 30 ui / dl DHL 943ui / dl calcium 9 mmol / l chlorine 87 mmol / l potassium 5.1mmol / l sodium 139mmol / l TP13.9 sec TTP 27.3 sec. With data of acute prerenal renal failure due to dehydration, hypochloremia due to vomiting and hemoconcentration, hyperbilirubinemia with phototherapy criteria, blood group b + compatible with the mother.
It is covered with double antimicrobial scheme with cefotaxime and ampicillin at renal dose. A radiograph of the abdomen is requested, which shows a triple bubble image with suspicion of intestinal atresia, (figure. 1) evaluation by pediatric surgery is requested.
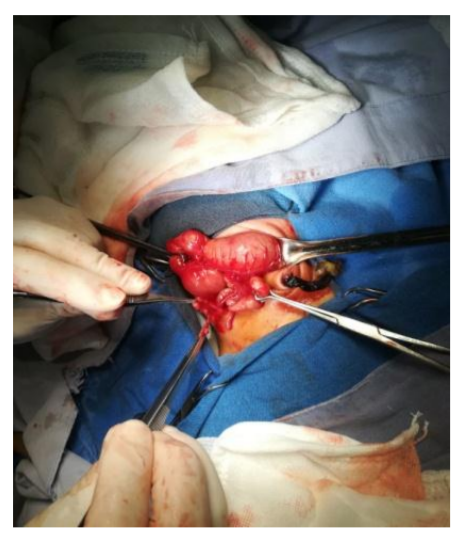
In the first assessment, it is suggested to stabilize the patient to perform exploratory laparotomy, which is performed on the 4th day after corrected renal failure, with surgical finding of atresia of the entire small bowel type III b only 2 cm of terminal ileum of 1 mm in diameter, it is not possible to perform anastomosis or intestinal bypass (Figure 2). It is determined to close and no change is made, parents are informed about their life prognosis that would not be viable with high chances of dying at any time. Support and support management is provided with parenteral nutrition in the neonatology service.
During two weeks of postoperative course with good evolution, without complications, remains stable without dehydration data or electrolyte imbalance, with normal vital signs monitoring, fed with parenteral nutrition is requested new assessment by pediatric surgery in another level of unanswered attention, what is revaluated in the second level requesting radiographs with contrast medium to evaluate intestinal transit, observing passage of contrast medium to the angle of treitz, contrast medium is introduced through the colon observing that there is permeability of the entire colon, a second surgical intervention at one month of age, finding as a very dilated duodenum and proximal jejunum of 5 cm continuing with non-viable atresicmidgut in apple peel, which is resected and viability and permeability is observed in 5 cm of the distal ileum in its vicinity to the ileocec valve al, anastomosis of the proximal-end distal ileum / oblique anastomosis in total approximately 10 cm of small intestine, intact ileocecal valve and the entire colon.
3. Surgical Technique
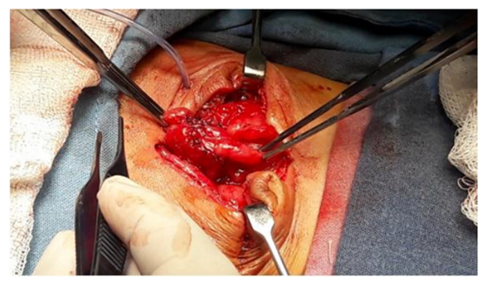
under general anesthesia, the midline approach to the cavity is followed by multiple firm adhesions, which are released and identified as stomach, duodenum, proximal jejunum of 5 cm, non-viable atresicmidgut of approximately 5 cm, resection is only viable and permeable 5 cm of distal ileum, in proximity to the ileocecal valve where resection and termination / oblique anastomosis with thread pds 6/0 simple points in a plane, permeability is confirmed and gastrostomy is performed with Foley probe 6 fr, closed with vicryl 4/0 the peritoneum and with vicryl 3/0 the wall, the subcutaneous tissue with vicryl 3/0 and the skin with nylon 3/0 with simple points is placed pen rose in the pelvic cavity next to the anastomosis (Figure. 3) Once again, intestinal transit was performed, where the contrast medium of the stomach was passed to the colon and patency of the anastomosis was observed. (Figure 4) gastrostomy tube feeding was started with amino acid formula and fed to the mother's breast presenting a scarce evacuation on the second day of feeding.
4. Nutritional Management In Charge Of Pediatric Gastroenterology
When it is stabilized after having presented acute renal failure and after the first surgery, nutritional management with parenteral nutrition was initiated, giving a protein intake of 3 grkg, lipids 3 grkg, carbohydrates from 10 to 11 grkg giving a total caloric contribution of 70 calories x kg, with 50 to 60% of carbohydrates, 15% of proteins and 20% of lipids, which allows the increase of weight to 2,500, after the second surgery with anastomosis oblique term, conserving 10 cm of intestine considered as small intestine.
Management is started with medication to decrease the number of stool-based bowel movements, cholestasis due to prolonged parenteral nutrition with administration of ursodeoxycholic acid, water-soluble and fat-soluble vitamins due to decreased intestinal absorption, probiotics that improve prealbumin levels as well as speed of weight gain and height, cholestyramine for colerethic diarrhea at pediatric doses. During his hospital stay he has remained without complications, without dehydration data or electrolyte imbalance, fed to the maternal breast at free demand, gastrostomy with amino acid formula and parenteral nutrition awaiting intestinal adaptation.
5. Discussion
Few entities in pediatrics especially in gastroenterology, nutrition and pediatric surgery, represent an important and significant management challenge, as represented by a child with short bowel syndrome (SIC) secondary to a surgical resection. The challenge begins for the pediatric surgeon when facing a child with an event that can be considered as catastrophic, with no possibility of survival unless a resection is practiced. He continues with a gastroenterologist and nutritionist where they face the challenge of feeding and / or nourishing a child, in whom the anatomical and functional surface of the intestine has been significantly reduced, conditioning a state of malabsorption of water, electrolytes and nutrients (proteins, fats, carbohydrates, vitamins and minerals). Giving the doctor the opportunity to put into play his knowledge of anatomy and physiology of the gastrointestinal tract[6]. why the importance of this case.
In this patient the opportunity to survive was found to be stable after his first surgery, not finding data of complications, maintaining his state of hydration and electrolyte balance, irrigation was performed with saline through the rectum to distend the intestinal surface of the ileum terminal and intestinal transit series was performed to verify the permeability of the colon and rectum.
The objective of surgical treatment will always be to achieve a continuity and a longer intestinal length, which will result in a greater absorption surface. When practicing an anastomosis it is very convenient to do it with good technique avoiding the edges to be injured, since the tissues of a newborn are very delicate, so the union of the distal ends should be hermetic, hemostatic, isoperistaltic, peritonizing and not stenosing[7]. Anastomoses were performed with a fenestrated, end-terminal and end-diamond probe, improving the prognosis. In this patient, an end / oblique technique was performed with suture threads that can be used for urological anastomoses to prevent wound dehiscence. And ensure permeability. The presence of ileocecal valve and the integrity of the colon allowed to improve the prognosis of this patient for their survival.
Enteral nutrition plays a predominant role by stimulating intestinal trophism through mechanisms of direct stimulation of enterocytes, gastric and pancreatic secretion with trophic effect in the intestine, breast milk provides probiotics and prebiotics such as galactooligosaccharides, hormonal and growth factors [8], as well as the administration of parenteral nutrition with macro and micronutrients, glutamine, electrolytes and water, providing the nutritional requirements during the most critical phases and favoring intestinal adaptation [9]. This patient is currently stable without nutritional, metabolic or infectious complications, in hydroelectric balance the adaptation period is from 2 months to 2 years.
6. Conclusion
Patients with short bowel syndrome are a challenge for the pediatrician, gastroenterologist and pediatric surgeon, nutritionist and nurse, so a multidisciplinary approach must be established focused on achieving optimal nutritional support, which meets the needs for growth and development decreasing complications in the short and medium term. The nutritional support plays a fundamental role for the survival of these patients.
References
- Reynoso E. y Cols. Atresia intestinal multiple: reporte de un caso. Revista medica del Hospital General de México. 2008; 71 (2): 94-98.
- Baeza-Herrera C, Salinas-Montes J, Salinas-Montes G, Montero-Uscanga CA, López-Castellanos J. Obstrucción duodenal congénita: comparación de dos métodos correctivo. RevGastroenterolMex. 2009; 74 (1): 1-5.
- Valdovinos D, Cadena J , Montijo E, Zárate F, Cazares F , Toro E, Cervantes R y Ramírez-Mayans J . Síndrome de intestino corto en ninos: actualidades en su diagnóstico y manejo. RevGastroenterolMex. 2012,77(3): 130-140.
- Cano-Salazar A, Tovar PL. Atresia yeyunal tipo IIIb o en cáscara de manzana. Reporte de caso clínico. Revista de la Facultad de Ciencias de la Salud. 2012; 9 (1): 68-71.
- Guzman MA, Prasad R, Duane S, Chadarévian JP. Multiple intestinal atresias associated with angiodysplasia in a newborn. Journal of Pediatric Surgery. 2011; 46: 1445–1448.
- Onofre LS, Albuquerque-Maranhão R, Soares-Martins EC, Girardi-Fachin C, Martins JL. Apple-peel intestinal atresia: Enteroplasty for intestinal lengthening and primary anastomosis. Journal of Pediatric Surgery. 2013; 48 E5–E7.
- J. Wang et al. Prolonged feeding difficulties after surgical correction of intestinal atresia: a 13-year experience. Journal of Pediatric Surgery. 2014; 49: 1593–1597.
- Ferrara G et al. More than (Double) Bubble. J Pediatr (internet) 2015 (citado 28 de abril del 2018); 1: 1-2. Disponible en: http://dx.doi.org/ 10.1016/j.jpeds.2015.06.06
- Cano-Muñoz I, Montoya-Mendoza N. Obstrucción duodenal en pacientes pediátricos. Anales de Radiología México. 2011; 4: 258-273.