Information
Journal Policies
ARC Journal of Clinical Case Reports
Volume-2 Issue-2, 2016, Page No: 12-15
Chronic Urticaria Due to Unusual Site and Trigger of Inflammation: A Case Report and Review of Literature
Latifa AlShekaili1, Safiah Sumayli1, Sulaiman Al Gazlan1,Farrukh Sheikh 1, Hasan Al Rayes1, Agha M. Rehan Khaliq1,2,Rand Arnaout 1, 2*
1 Section of Allergy/Immunology, Department of Medicine, King Faisal Specialist Hospital & Research Centre, Section of Allergy & Immunology, Kingdom of Saudi Arabia.
2 Al Faisal University, Riyadh, Kingdom of Saudi Arabia.
3Section of Allergy/Immunology, Department of Pediatric, King Faisal Specialist Hospital & Research Centre, Kingdom of Saudi Arabia.
2 Al Faisal University, Riyadh, Kingdom of Saudi Arabia.
3Section of Allergy/Immunology, Department of Pediatric, King Faisal Specialist Hospital & Research Centre, Kingdom of Saudi Arabia.
Citation : Arnaout R, Sumayli S, Al Gazlan S, et al. Chronic Urticaria Due to Unusual Site and Trigger of Inflammation: A Case Report and Review of Literature. ARC Journal of Clinical Case Reports. 2016;2(2):12–15.
Copyright : © 2016 Arnaout R. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Urticaria is one of the most frequent skin disorders encountered in medical practice and it can significantly impair the quality of life. It is more common to be in its acute form (less than six weeks) than in chronic form (more than six weeks). There is longstanding evidence that infection or inflammation can trigger urticaria. Most of the reported cases are about acute urticaria. The majority of data come from bacteria: H. pylori infection. However, there are a number of reports about different types of infections as causative reasons of urticaria. In this case report we illustrate an usual site of inflammatory reaction as a cause of chronic urticaria in a 48 years female patient.
1.Introduction
Urticaria is one of the most frequent skin disorders encountered in medical practice. Urticaria is defined as acute if the urticarial lesions recur for less than six weeks and as chronic if it persists for longer than six weeks [1]. Chronic urticaria, which can last from several weeks to several years or decades, can significantly impair the quality of life [2-5]. There are many underlying causes for both acute and chronic urticaria. The subject of urticaria triggers has been intensely investigated by clinicians and researchers. Controversy surrounds the role of occult infection in the pathogenesis of different urticarial subtypes. In case of acute urticaria the role of infection is well established but due to the limited duration of acute urticaria this does not result in a specific management. Acute urticaria is considered as a known symptom or consequence of viral infection in general, but especially in children [7-9] . Recent data found infection to be the most commonly identified cause of acute urticaria in one series (37%) [10]. In another series, infection was identified in 57% of acute urticaria cases, benign viral upper respiratory (nasopharnygitis) or gastrointestinal tract infections being the most frequent etiology [11]. A third series found that 20-30% of children with spontaneous acute urticaria were triggered by infection, 91% of these acute cases progressed to chronic form of urticaria[9].
In the field of chronic urticaria randomized controlled trials are scarce, but there is increasing evidence that persistent infections are important triggering factors [6]. Although infection has been identified as one of the possible trigger in urticaria, yet the prevalence of infections; bacterial, viral, parasitic or fungal, appears not to differ in spontaneous chronic urticaria compared to the general population, Yet, there is a very large amount of reports demonstrating benefit after eradication of infectious processes in form of complete resolution of the urticaria [7]. Most reported infections in chronic urticaria are related to the gastrointestinal tract, dental and ENT region.
Occasionally the site of infection/inflammation that might be triggering the chronic urticaria is unusual and/or unapparent which require careful history, thorough physical exam and focused investigations, like the patient in this reported case. We hereby present a case of chronic urticaria in an adult female secondary to cosmetic facial filler inflammation which resolved after three weeks of broad spectrum antibiotics and did not recur after treatment and several months of follow up.
2.Case Report
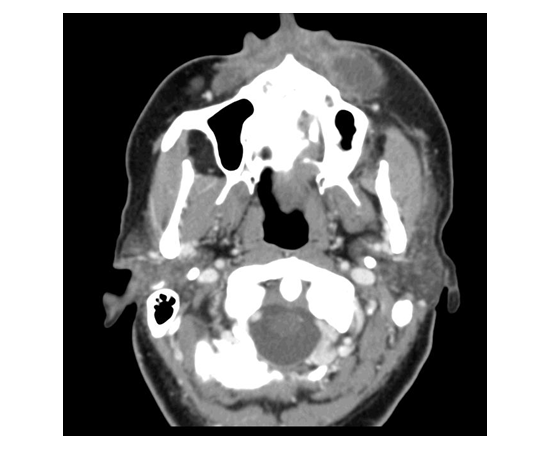
A 48 years old, Saudi lady was referred to our Allergy clinic with 8 weeks history of urticarial lesions in the form of pruritic erythematous wheals and flares all over her body ranging from a few millimeters to several centimeters in diameter, not associated with angioedema or anaphylactic symptoms. Cutaneous manifestations were not related to a specific inducing factor like food or drug. She had no benefit from maximum anti-histamine and steroids given to her from a private clinic. Allergi history was negative. During patient clinic visit and during physical exam, we noticed a mild swelling along the left parotid area which she thought was from dental problem. So, in addition to the usual workup for chronic urticaria which included; complete blood count with differential, erythematous sedimentation rate, complements levels, CH50, free T4, TSH and Antinuclear antibodies, which were all normal, we added parotid ultrasound, worth mentioning that our dental exam was normal. The radiologist who did the ultrasound advised for CT scan for head and neck which was done and revealed that the patient had cosmetic filler of both cheeks, but with significant inflammation around the left side indicating possible infection. The patient did not mention any cosmetic procedures during her interview, when questioned after the Ct results she admitted to the cosmetic filling procedure in one of the small clinics in the city almost one week before the start of her urticarial symptoms. The material that was injected in the filling was not documented.The Patient was started on broad spectrum antibiotics for three weeks after which she came for follow up visit and had complete resolution of the swelling and had no urticaria lesions for past two weeks for the first time in two months. No cultures were obtained from the filler due to sensitivity of the region and patient preference to see the response to antibiotics. In the follow up visit after two months of stopping the antibiotics, patient still had no urticaria and no recurrence of the swelling. Patient was advised to follow with her cosmetic dermatologist for possible recurrence of infection and all her anti-histamines had been stopped for one month with no symptoms.(Figure 1)
3.Discussion
Although by definition all chronic urticaria cases must have started as an acute urticaria, and the acute form can be triggered by infections, there are no clear-cut data to confirm a direct link between infections and chronic urticaria [12]. Various correlations ranging from reasonably convincing to less so, have been published. The best data come from bacterial infection like,H. pylori infection and also from Hepatitis B, Hepatitis C infection [13]. It is no matter of debate that the prevalence of infections in chronic urticaria is similar to control groups; however, patients who develop chronic urticarial their immune response to infections may differ and those may develop infection-induced autoreactivity/ autoimmunity. This led to the employment of epitope mimicry as a possible mechanism for development of chronic urticaria in the context of infection. Clinical data support the involvement of infectious agents in the pathogenesis of urticaria, yet, proving its existence can be quite a clinical challenge especially if the infection resides in an unapparent site and/or inaccessible site.
There are many emerging case reports proving that unusual or unapparent infections should be truly looked for, as a possible cause of chronic urticaria, like Blastocystis hominis infestation in certain parts of the world [14]. Although large number of parasites have been correlated with urticaria, but few data exist regarding Blastocystis hominis infection; however, a series of case reports revealed the great association. In addition,genital herpes simplex infection, Tinea infection in different sites as between toes and Pelvic inflammatory disease had been reported as possible causes of chronic urticaria [15-17]. Therefore, thorough history,physical examination and focused investigations should be performed for any patient present with chronic urticaria.
We believe in case of our patient, the filler infection which was apparent on CT scan as inflammation was triggering her urticaria. Although there was no culture to prove the infection, her symptoms resolution with antibiotics with no recurrence, highly suggests that.
In the era of revolution in cosmetic procedures, there are many dermatological or cosmetic interventions that might be a newer port of infection which could induce urticaria of either acute or chronic form. Reported cases of chronic urticarial after these procedures are limited, in part because of their good safety profile. To our knowledge this is the first case report to document chronic urticaria post cosmetic facial filler. However, there are four cases reported of acute urticaria post laser treatment for hair reduction and another case reported as Mesotherapy-induced acute urticarial [18,19]. In addition, there is one case reported cold-induced urticaria after fractional CO2 laser resurfacing of the face [20].
Although there is published data suggested that there is no detectable allergenicity (immediate Type I or delayed Type IV hypersensitivity) of hyaluronic acid skin filler injection and an absence of immunogenicity in almost all individuals receiving Restylane or Perlane as dermal fillers, there are also contradicting reports of urticarial vasculitis post nonanimal hyaluronic acid skin filler injection and a risk of granuloma formation [21-23].
With any cosmetic procedure there is always a remote but possible risk of infection. In our case the filler was facial and we could detect a small swelling despite the fact that patient did not mention the procedure in the history. These cosmetic fillers can be done in many parts of the body including the breast, the gluteal area and others, which might be less apparent to the physician and more difficult to detect. So we recommend that with the wide-spread practice of cosmetic procedures to keep these procedures in mind when investigating a patient with recently developed urticaria or allergic reaction.
References
- Zuberbier T, Greaves MW, Juhlin L, Kobza-Black A, Maurer D, Stingl G, Henz BM (2001) Definition, classification and routine diagnosis of urticaria – a consensus report. J Journal of Investigative Dermatology Symposium Proceedings 6: 123-127.
- Wedi B, Raap U, Wieczorek D, Kapp A (2009) Urticaria and infections. Allergy Asthma and ClinicalImmunology 5:10.
- Kozel MMA, Mekkes JR, Bossuyt PM, Bos JD (2001) Natural course of physical and chronic urticaria and angioedema in 220 patients. Journal of American Academy of Dermatology 45: 387-391.
- Valk PG, Moret G, Kiemeney LA (2002) The natural history of chronic urticaria and angioedema in patients visiting a tertiary referral center. British Journal of Dermatology 146: 110-113.
- Zuberbier T, Bindslev-Jensen C, Canonica W, Grattan CE, Greaves MW, Henz BM, Kapp A, Kozel MM, Maurer M, Merk HF, Schafer T, Simon D, Vena GA, Wedi B (2006) EAACI/GA2LEN/EDF guideline: definition, classification and diagnosis of urticaria. Allergy 61: 316-320.
- Bettina Wedi, Ulrike Raap, Dorothea Wieczorek and Alexander Kapp. Urticaria and infections. Allergy, Asthma & Clinical Immunology 2009, 5:10.
- Wedi B, Raap U, Kapp A: Chronic urticaria and infections. Current Opinion in Allergy and Clinical Immunology2004, 4:387-96.
- Bilbao A, Garcia JM, Pocheville I, Gutierrez C, Corral JM, Samper A, Rubio G, Benito J, Villas P, Fernandez D, Pijoan JI: Round table: Urticaria in relation to infections. AllergologiaetImmunopathologia1999, 27:73-85.
- Sackesen C, Sekerel BE, Orhan F, Kocabas CN, Tuncer A, Adalioglu G: The etiology of different forms of urticaria in childhood. Pediatric Dermatology2004, 21:102-8.
- Kulthanan K, Chiawsirikajorn Y, Jiamton S: Acute urticaria: etiologies, clinical course and quality of life. Asian Pacific Journal of Allergy and Immunology2008, 26:1-9.
- Liu TH, Lin YR, Yang KC, Chou CC, Chang YJ, Wu HP: First attack of acute urticaria in pediatric emergency department. Pediatrics and Neonatology2008, 49:58-64.
- Wedi, Bettina; Raap, Ulrike; Kapp, Alexander,Chronic urticaria and infections. Current Opinion in Allergy & Clinical Immunology. 4(5):387-396, October 2004.
- Hellmig, S.; Troch, K.; Ott, S. J.; Schwarz, T.; Folsch, U. R. Role of Helicobacter pylori Infection in the Treatment and Outcome of Chronic Urticaria. Helicobacter. 13(5):341-345, October 2008.
- Pasqui AL, Savini E, Saletti M, Guzzo C, Puccetti L, Auteri A, Chronic urticaria and blastocystishominis infection: a case report, European Review Medical and Pharmacological Sciences 2004 May-Jun;8(3):117-20.
- Zawar V, Godse K, Sankalecha S, Chronic urticaria associated with recurrent genital herpes simplex infection and success of antiviral therapy-a report of two cases, International Journal of Infectious Diseases. 2010 Jun;14(6):e514-7. doi: 10.1016/j.ijid.2009.06.008. Epub 2009 Aug 21.
- Godse KV, Zawar V, Chronic urticaria associated with tinea infection and success with antifungal therapy--a report of four cases, International Journal of Infectious Diseases, 10 Sep;14 Suppl 3:e364-5. doi: 10.1016/j.ijid.2009.12.005. Epub 2010 May 6.
- Tachdjian R, Tourangeau L, Schneider JL, Nel A, Urticaria associated with necrotic uterine leiomyomas infected with salmonella, Obstetrics Gynecology. 2010 Aug;116 Suppl 2:491-3.
- Eric F. Bernstein, Severe UrticariaAfter Laser Treatment for Hair Reduction, Dermatologic Surgery 2010;36:147–151.
- Efstathios Rallis, StephanosKintzoglou, Mesotherapy-Induced Urticaria, Dermatologic Surgery 2010;36:1355–1357
- Nancy Habib, NazaninSaedi, Christopher Zachary, Cold-Induced Urticaria After Fractional Carbon Dioxide Laser Resurfacing of the Face, Dermatologic Surgery2011;37:1700–1703.
- Robert G., D.AbMLI, JurStrobos , Franklin Adkinson , Immunogenicity studies of cosmetically administered Nonanimal-Stabilized hyaluronic acid particles, Dermatologic Surgery 2007; 33:S176-S185.
- JaumeAlijotas-Reig, Recurrent Urticarial Vasculitis Related to Nonanimal Hyaluronic Acid Skin Filler Injection, Dermatologic Surgery 2009;35:395–398.
- Seth L. Matarasso, Robert Herwick, Hypersensitivity reaction to nonanimal stabilized hyaluronic acid, Journal of American Academy of Dermatology JULY 2006 55(1):128-131.