Information
Journal Policies
Sustained Remission of a Seronegative Rheumatoid Arthritis after Dental Treatment: A Case Report
Wolff B 1, Berger T 1, Blank N2, Max R2, Lorenz HM2, Wolff D1
2Division of Rheumatology, Department of Medicine V University of Heidelberg, Heidelberg, Germany.
Copyright : © 2016 Wolff B. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Seronegative Rheumatoid Arthritis, Oral Infectious Focus, Dental Treatment , Clinical Remission.
1.Introduction
Both rheumatoid arthritis (RA) and periodontitis (PD) are chronic diseases characterized by inflammation. Untreated, RA and PD result in destruction of bone and extracellular matrix by osteoclast activation. In RA joints and cartilage are degraded. In PD inflammation leads to loss of periodontal attachment and destruction of alveolar bone. Also, proinflammatory cytokines such as tumornecrosis factor alpha (TNF-alpha), interleukins IL-6, IL-1, IL-17 and matrixmetalloproteinases (MMP-3, MMP-8) are elevated in inflamed tissue of RA and PD [1, 2]. Porphyromonas gingivalis the leading oral pathogen in PD was identified as link between both diseases. P. gingivalis is the only bacteria known to produce peptidyl arginine deiminase, which is a potential source of RA specific anti-citrullinated peptide antibodies (ACPAs) [3]. Recently, in a large cohort study a strong association of antibodies against gingipain virulence factor of P. gingivalis was found in patients with RA [4]. In patients with early RA more advanced forms of periodontitis and increased attachment loss were found compared with healthy controls [5]. As PD is one of the most common human diseases globally affecting up to 50% of adults [6] it likely precedes the onset of RA. Infectious oral foci may serve as trigger factor whereas longstanding infection with P. gingivalis breaks down autoimmune tolerance locally in genetically predisposed patients. Periodontal treatment effectively removes P. gingivalis and other oral pathogens. Non-surgical periodontal therapy of patients with RA with periodontitis may provide beneficial effects on local inflammatory control [7]. Here we report a case of sustained clinical remission of an anti-cyclic citrunillated (anti-CCP) peptide antibody negative early RA after dental treatment of oral infectious foci.
2. Presentation of Case
In 2010-06 a 64-year-old Caucasian man was referred to the division of rheumatology at the university of Heidelberg. He reported increasing morning stiffness (> 30 minutes) and pain in fingers, hip and shoulders over the last 6 months. Tendovaginitis stenosans with reported synovial proliferations at digits IV and III on both sides was operated between 2006 and 2008. He was diagnosed with a seronegative, anti-CCP-negative RA. Disease activity was high (Disease Activity Score [DAS28] = 5.73, C-reactive protein 22mg/l) and physical function impaired (Health Assessment Questionnaire score [HAQ] = 1.25). Synovitis and periarticular demineralization were present at the proximal interphalangeal joints and metacarpophalangeal joints II and III on both sides. Oral medication with prednisolone 20mg in the first week and 5mg (every 5 days) in the second week, nonsteroidal-anti-inflammatory-drugs (Diclofenac 50mg once per day) and opioids (Tramadol 100mg once per night) was initiated.
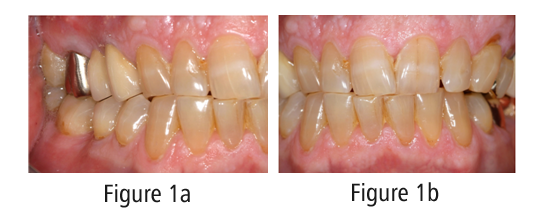
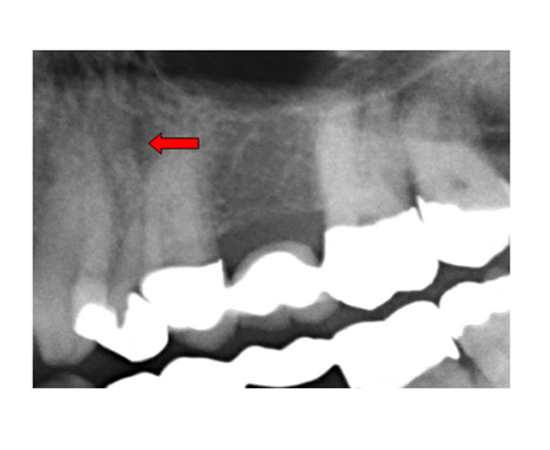
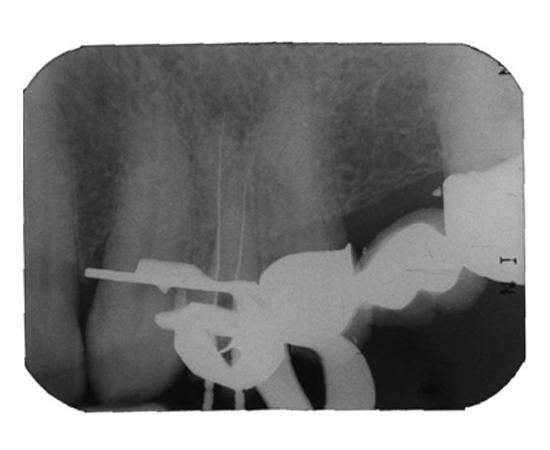
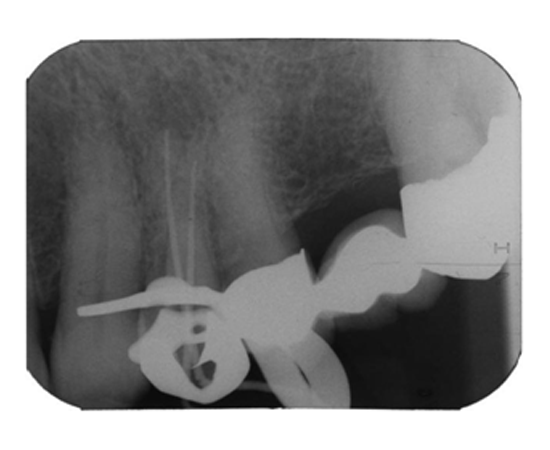
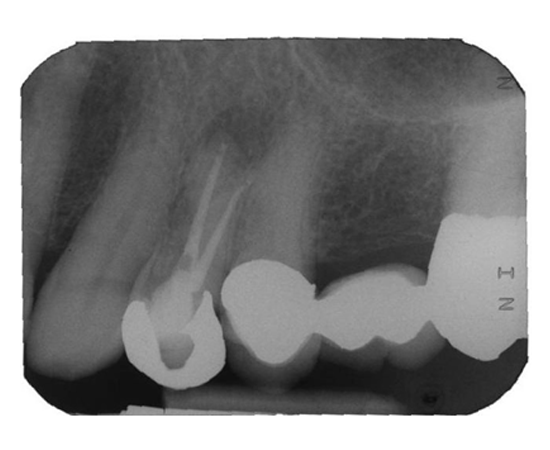
In 2010-07 the patient presented for a dental check-up at the Department of Conservative Dentistry at the University of Heidelberg. All teeth were sensitive except for the maxillary left first premolar (tooth 24). Vestibular palpitation and percussion on 24 were painful. Radiographic examination revealed a distinct apical translucency on 24. Baseline oral hygiene indices were Plaque-ControlRecord (PCR): 52% and Gingival-Bleeding-Index (GBI): 13%. Mean Probing-Pocket-Depth (PPD) was 3.2 mm, mean Clinical-Attachment-Level (CAL) was 3.3mm. The patient was diagnosed a generalized mild, localized moderate chronic periodontitis and pulpal necrosis/apical periodontitis on 24. Patient did not report antibiotic use in the past 3 months or periodontal treatment in the past 6 months. The patient underwent professional tooth cleaning (PTC) and oral hygiene instruction. Tooth 24 was endodontically treated (mechanical instrumentation, irrigation with chlorhexidine (0.2%) and sodium hypochlorite (2.5%), temporary root canal filling with calcium hydroxide). After 2 weeks palpitation and percussion on 24 were not painful anymore. Oral hygiene indices reduced to PCR: 11% and GBI: 0%. HAQ score reduced to 0.0. In 2010-10 disease activity was reduced (DAS28 2.9). In 2010-11 warm guttapercha obturation technique was used for orthograde root canal filling of tooth 24. In 2010-12 a cystectomy combined with an apicoectomy with retrosurgical filling (Mineral Trioxid Aggregate) was performed on tooth 24. Histological examination resulted a radicular cyst. Patient reported that since the dental therapy he was free of pain in the oral cavity and that his signs and symptoms of RA had decreased. Therefore, he had reduced his medication to Diclofenac 50mg weekly and he had stopped the use of Tramadol and corticosteroids. Also, he did not start his prescribed methotrexate (10mg/weekly subcutaneously). In 2011-09 the patient was in drug free clinical remission (DAS28 1.9, CRP < 2mg/l). In a follow-up of almost 3 years (2014-03) patient was free of RA related symptoms.
3. Discussion
In this case report the successful dental treatment of a generalized mild, localized moderate chronic periodontitis and the surgical removal of a radicular cyst at tooth 24 lead to spontaneous reduction of signs and symptoms of an anti-CCP negative, seronegative RA. Anti-rheumatic medication was reduced and a drug free clinical remission achieved and sustained over 3 years of follow-up. A recent review and meta-analysis of five studies supported the hypothesis that control of periodontal infection and gingival inflammation by non-surgical periodontal treatment could reduce the clinical and biochemical markers of active RA although the studies had short follow-up and small sample sizes [8]. In this case a P. gingivalis driven expansion of anti-CCP antibodies cannot explain the onset of RA. Here, a chronic low-grade oral infection and a tendovaginitis stenosans with synovial proliferations may have exacerbated or triggered RA according to two-hit model [9].
This case report supports the effectiveness of dental anti-inflammatory treatment on anti-CCP negative rheumatoid arthritis.
4. Conclusion
Patients with RA and poor oral status or suspected oral infectious foci should be referred directly for intensive dental care by the treating rheumatologist.
5.Figures
Figure 1(a-e): Baseline visit (2010-07). a-c Clinical images of the baseline situation, patient did not receive periodontal treatment during the last 5 years. Plaque and calculus are present especially interproximally. d Radiographic image showing an apical translucency on 24.
Figure 1(f-k). Clinical situation after professional tooth cleaning h-i Endodontic treatment j Root canal filling and apicoectomy - postoperative radiograph k Two-months follow-up radiograph
References
- I. B. McInnes and G. Schett, "The pathogenesis of rheumatoid arthritis," N Engl J Med, vol. 365, pp. 2205-19, Dec 8 2011.
- G. Hajishengallis, "Periodontitis: from microbial immune subversion to systemic inflammation," Nat Rev Immunol, vol. 15, pp. 30-44, Jan 2015.
- W. T. McGraw, J. Potempa, D. Farley, and J. Travis, "Purification, characterization, and sequence analysis of a potential virulence factor from Porphyromonas gingivalis, peptidylarginine deiminase," Infect Immun, vol. 67, pp. 3248-56, Jul 1999.
- N. Kharlamova, X. Jiang, N. Sherina, B. Potempa, L. Israelsson, A. M. Quirke, et al., "Antibodies to Porphyromonas gingivalis indicate interaction between oral infection, smoking and risk genes in rheumatoid arthritis etiology," Arthritis Rheumatol, Nov 10 2015.
- B. Wolff, T. Berger, C. Frese, R. Max, N. Blank, H. M. Lorenz, et al., "Oral status in patients with early rheumatoid arthritis: a prospective, case-control study," Rheumatology (Oxford), vol. 53, pp. 526-31, Mar 2014.
- W. S. Borgnakke, "Does Treatment of Periodontal Disease Influence Systemic Disease?," Dent Clin North Am, vol. 59, pp. 885-917, Oct 2015.
- S. Kurgan, O. Fentoglu, C. Onder, M. Serdar, F. Eser, D. N. Tatakis, et al., "The effects of periodontal therapy on gingival crevicular fluid matrix metalloproteinase-8, interleukin-6 and prostaglandin E levels in patients with rheumatoid arthritis," J Periodontal Res, Nov 17 2015.
- S. Kaur, R. Bright, S. M. Proudman, and P. M. Bartold, "Does periodontal treatment influence clinical and biochemical measures for rheumatoid arthritis? A systematic review and metaanalysis," Semin Arthritis Rheum, vol. 44, pp. 113-22, Oct 2014.
- L. M. Golub, J. B. Payne, R. A. Reinhardt, and G. Nieman, "Can systemic diseases co-induce (not just exacerbate) periodontitis? A hypothetical "two-hit" model," J Dent Res, vol. 85, pp. 102-5, Feb 2006.