Information
Journal Policies
Contribution of Conventional Imaging in the Diagnosis of Cardiac Valvular Fibroelastoma: A Case Report and Literature Review
Lalla Fatima Ezzahra El Hassani1, Salwa Cheraou1, Ilyas El Kassimi2*, Fatima Zahra Mrabet3, Nawal Doghmi1, Mohamed Cherti1
2.Internal Medicine Department, Mohammed V Military teaching Hospital, Rabat, Morocco.
3.Department of Pulmonology, Ibn Sina University Hospital Center, Rabat, Morocco.
Copyright : © 2019 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Papillary fibroelastoma is a rare benign primary cardiac tumor that can lead to severe embolic complications. We report a case of papillary fibroelastoma of the aortic valve revealed by a transient ischemic attack on a 45 years old woman. It was in the context of the etiological assessment of this ischemic accident that transthoracic echocardiography had shown a small, pedunculated mobile and echo dense mass on the aortic valve which was later confirmed by a transesophageal echocardiography of which ultrasound characteristics are in favor of papillary fibroelastoma. In front of the high emboligenic potential, the mass was excised and histologically analyzed and the diagnosis of fibroelastoma was confirmed. The evolution after the intervention was favorable with the absence of signs of tumor recurrence and good functioning of the aortic valve.
Like all tumors, the confirmation of the diagnosis is obtained after a pathological study. However, the interest of this paper is to raise the primordial role of imaging in the positive diagnosis of papillary fibroelastoma by showing very characteristic aspects of this tumor which makes it possible to evoke it in the first intention.
Papillary fibroelastoma; transthoracic echocardiography; transesophageal echocardiography; aortic valve; Surgery.
PFE: Papillary fibroelastoma, BPM: beats per minute, CT: Computed tomography, TIA: transient ischemic attack, TTE: transthoracic echocardiography, TEE: transesophageal echocardiography
1. Introduction
Papillary fibroelastoma is a primary cardiac tumor benign. It accounts for about 7% of heart tumors primitives. Although the prevalence of primary cardiac tumors ranges from 0.0017-0.28% [1, 2], the papillary fibroelastomas (PFE) are the third in order of frequency after the myxoma and lipoma [3].
We report a case of papillary fibroelastoma by insisting on the fundamental place of imaging techniques in diagnosis especially transthoracic echocardiography and transesophageal echocardiography.
2. Case Presentations
A 45-year-old female presented to our hospital for recurrent chest pain with radiation to inter-scapular area. In the interrogation, she had a history of hypertension, palpitation and numbness on the left side of her face, mouth, upper and lower extremities. Symptoms resolved spontaneously in one hour with no sequel. The clinical examination is unremarkable, No breath or noise added, blood pressure were 120/75 mmHg and her temperature were 37°C.
The electrocardiogram fits in sinus rhythm with a heart rate at 85 BPM, without cavitary overload. The Chest X-ray was normal, blood cultures as well as the inflammatory balance (sedimentation rate, fibrinogen and procalcitonin) were negative ruling out a diagnosis of endocarditis. The measure of troponin and D-Dimers was also negative.
Computed tomography scan of the head and CT angiography of cerebral and carotid arteries were unremarkable.
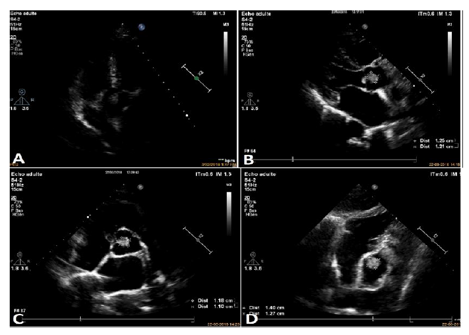
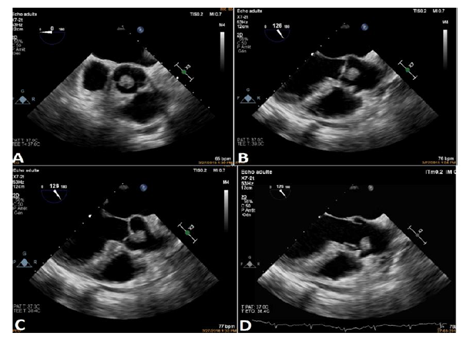
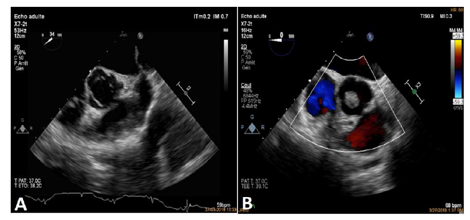
Based on these findings, the diagnosis retained was a transient ischemic attack (TIA). In the context of etiological assessment, the transthoracic echocardiography (TTE) showed a mobile and echo dense mass on the aortic valve which was later confirmed by a transesophageal echocardiography. By this last, it was seen a mobile pedunculated round mass 1.40 X 1.27cm maximum on the aortic side of the right-coronary cusp of a tri-leaflet aortic valve. This valvular echogenic mass was found to be moving during each phase of the cardiac cycle and just adjacent to the origin of right coronary artery. This mass was attached to the aortic valve near to the origin of the right coronary artery (Figure 1 and 2). However, the aortic valve and other cardiac structures were normal. There was no regurgitation of the aortic valve. (Figure 3 and 4).
The first diagnosis to evoke in order of frequency was a fibroelastoma, without being able to rule out a tumor of another origin, but it allows to exclude its fibrinocruoric nature. An operative indication was chosen to avoid thromboembolic recurrences because of the pediculated nature of the tumor on the one hand, and its size on the other, and, finally, to know its histological nature. Surgery under extracorporeal circulation was performed with surgical excision of tumor and preservation of the aortic valve, on exploration a 1.21 X 1.20 cm pedunculated mass was found, it was attached to the right coronary cusp very close to the commissure between the right and non-coronary cusp of the aortic valve. The mass was firm, glistening friable and looked filamentous on examination.
The operative follow-up was simple. Pathological examination of the resected tumor revealed a papillary proliferation including few fibroblasts collagen and elastic fibers, covered with hyperplastic endothelial cells which allowed to confirm the diagnosis of papillary fibroelastoma.
3. Discussion
Cardiac papillary fibroelastomas is a primary benign endocardial tumors arising from the normal component of the endocardium like fibrous tissue, elastic fibers or smooth muscle cells. The origin of PFE is unclear and various possible causes have been mentioned in the literature. They have been considered as hamartomas, organized thrombi, iatrogenic (post radiation, surgery) or inflammatory foci due to unusual endocardial responses to infection or hemodynamic trauma [2, 4]. However, some authors believe that PFE’s are true neoplasms [1, 2]. Law and all have found 833 cases published so far with a male preponderance (58%) and mean age of 56 years. The same results have been published by Gowda RM and all [5].
The tumor size ranged from 2 to 70 mm. The most preferred location is aortic (44-52%) followed by mitral valve (25-30%), tricuspid valve (17%) and pulmonary valves (13%) [1]. In majority of the cases, they have a short pedicle and multiple papillary fronds similar to a sea anemone. However PFE arising from semilunar valves are located with equal frequencies on the ventricular and arterial sides of the valves [1, 5]. In addition, non-valvular origin was described in 16% of cases; the tumor can affect the left ventricle, the right ventricle, the atrium, the papillary muscle… [1, 6].
Clinical presentation of PFE’s varies from asymptomatic to severe thromboembolic complications, myocardial ischemia, infarction and stroke [7]. However pulmonary embolism, congestive heart failure, near- syncope ventricular fibrillation and sudden death have also been reported [1, 6, 8, 9]. Embolization may occur from fragments of the fronds of the tumor or from a thrombus that frequently forms on the tumor ‘nidus’ due to platelet or fibrin aggregates. In our patient, the atypical vague chest discomfort and pain could have been due to the partial, intermittent obstruction or limitation of blood flow through the right coronary artery orifice in the aortic root due to the strategic location and variable mobility of the tumor mass during various phases of cardiac cycle. Therefore, this could be considered as angina-like symptom. But the transient ischemic attack (TIA) could have been due to the partial, embolization from fragment of the fronds of tumor.
The diagnosis is usually made by 2-dimentional or transoesophagea echocardiography. Recently, 3-D echocardiography, magnetic resonance imaging and multislice spiral computed tomography have also been used for better delineation of similar tumors [4, 10]. Typical echocardiographic features include a small (1-4 cm), highly mobile mass with a pedicle attached to the valve or endocardial surface and a frond-like appearance with or without multifocal involvement [10]. It appears round, oval, or irregular on echocardiography but it is generally well-demarcated and homogenous in appearance. When image quality is optimal, a “speckled appearance” with “stippling” around the perimeter could be seen. In majority of the cases, single lesions are detected by echocardiography but the tumor can also affect more valve structures, aortic, mitral, tricuspid [11]. The majority of patients have the tumors on valves with normal function. Rarely this tumor could be responsible for valve dysfunction. The echocardiographic aspect found in our patient is similar to the one described in the literature.
Despite the benign nature of this tumor, it carries very high risk of embolic complications including neurological deficit. The fragile nature and frond-like papillary tissues of the tumor itself is prone to thromboembolism [1, 8]. Embolic complications may be favored by the deposit of thrombotic material on the tumor, but no data are available on the possible efficacy of anticoagulant or antiagre-glove treatments. However, the management of such tumors also includes early anticoagulation [12].
Therefore, once diagnosed, urgent surgical management is indicated even in the symptomatic or asymptomatic patients [1, 6, 13] with mobile and voluminous mass at least 10 mm in the left heart. A conservative surgery is possible for at least 90% of the aortic or mitral locations. The indication is more questionable for asymptomatic left-heart fibroelastoma, the fibroelastoma of the right-heart and tumor less than 10 mm, which could be the subject of a simple monitoring [13]. For that, surgery was indicated in our patient.
The PFE’s are usually pedunculated and may be easily removed with associated endocardial tissue. Care should be taken to avoid fragmentation of the tumor tissue. Also, aortic valve should be preserved preferably. In case, if there is resultant valve defect, it should be repaired, otherwise a valve replacement is warranted. The surgical resection is curative, safe and well tolerated [6, 9, 13]. Intraoperative TEE is essential to assess valvular function after tumor resection. Re-growth of the tumor after resection has not been reported, and it requires long-term TEE follow-up studies to confirm.
In our patient, the surgical procedure under extracorporeal circulation was carried out with chirurgical resection of the tumor and conservation of the Aortic valve, the operative sequences were simple and the pathological studies allowed to confirm the diagnosis of the papillary Fibroelastoma.
Conclusion
The fibroelastoma is rare and benign heart valve tumor for which the exact prevalence remains unknown; it is associated with a high embolic risk. Ultrasound imaging makes it easier to access the diagnosis. A strong suspicion, appropriate use of imaging modality, preoperative anticoagulation and urgent resection of the tumor is not only lifesaving but also avoids tumor-related vascular, embolic or neurological complications.
References
- Jha et al. Papillary fibroelastoma of the aortic valve - a case report and literature review. Journal of Cardiothoracic Surgery 2010; 5:84. doi: 10.1186/1749-8090-5-84.
- Bicer M, Cikirikcioglu M, Pektok E, Muller H, Dettwiler S, Kalangos A. Papillary fibroelastoma of the left atrial wall: a case report. Journal of Cardiothoracic Surgery 2009, 4:28.
- Bouferrouk A, Boutamine S. Fibroélastome papillaire de la valve mitrale. Sang Thrombose Vaisseaux 2012; 24 (6): 305-307. doi:10.1684/ stv.2012.0712
- Srilkan Y and All: Cardiac papillary fibroelastoma; The need for a timely diagnosis, World j Clin 2017, January 2016, 5(1): 9-13
- Gowda RM, Khan IA, Nair CK, Mehta NJ, Vasavada BG, Sacchi TJ. Cardiac papillary fibroelastoma: a comprehensive analysis of 725. Am Heart J 2003, 146; 404-410
- E. Prifti et al. Papillary fibroelastoma of the anterior leaflet of the mitral valve mimicking vegetation. International Journal of Surgery Case Reports 14 (2015) 19–22
- Miller et al. Aortic valve papillary fibroelastoma causing embolic strokes: a case report and review. International Medical Case Reports Journal 2017:10
- Marchais H, Rebika S, Bonnin N, Kémény J.L, Paulon C & Chiambaretta F. Tumeur intracardiaque à l’origine d’oblitérations de l’artère centrale de la rétine à répétitions. Journal Français d'Ophtalmologie; November 2017, Vol. 40 Issue: 9 pe353-e355, 3p. doi:10.1 016/j.jfo.2016.10.025
- Yandrapalli S, Mehta B, Mondal P, Gupta T, Khattar P, Fallon J, Goldberg R, Sule S, Aronow WS. Cardiac papillary fibroelastoma: The need for a timely diagnosis. World J Clin Cases 2017; 5(1): 9-13.
- Chia PL. Incidental finding of an aortic valve mass on 64-slice computed tomographic coronary angiography. Annals Academy of Medicine 2009, 38(10):926-927.
- Vittala et all. Multiple papillary fibroelastomas. Circulation. 2012; 126:242-243. DOI: 10.1161/CIRCULATIONAHA.111.049569.
- McCanny A, Imran Hamid U, Carroll S, Jeganathan R ; Fibroelastoma of the aortic valve; J Card Surg. 2017 Nov;32(11):698-699. doi: 10.1111/jocs.13232.
- Sabet A, Haghighiabyaneh M, Tazelaar H, Raisinghani A & DeMaria A. The Clinical Dilemma of Cardiac Fibroelastic Papilloma. Structural Heart, 2(4), 274-280. Doi: 10.1080/ 24748706.2018.1475782.