Information
Journal Policies
Cardiac Surgery in Elderly Obese Patients
Elif Dogan Baki1*, Ozge Okursoy1, Serdar Ozkul1, Remziye Sivaci1, Elif Buyukerkmen1, Ahmet Yuksek1
Copyright : © 2018 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Objective: Obese patients constitute a significant proportion of patients undergoing coronary artery surgery. The aim of this study was to evaluate mortality and morbidity in elderly obese patients undergoing open heart surgery.
Methods: The study included 139 patients aged ≥65 years from a total of 341 patients who underwent open heart surgery in our clinic between January 2014-2017. These were divided into three groups according to body mass index (BMI): Group 1 (BMI < 25), Group 2 (BMI = 25-30) and Group 3 (BMI ≥30). Demographic data, type of surgery, comorbidities, laboratory values, postoperative complications, intensive care and hospital stay, mortality rates were recorded and compared between the groups.
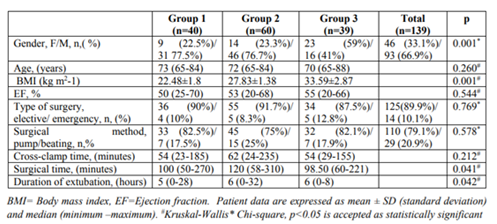
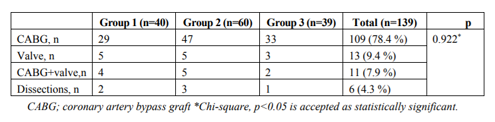
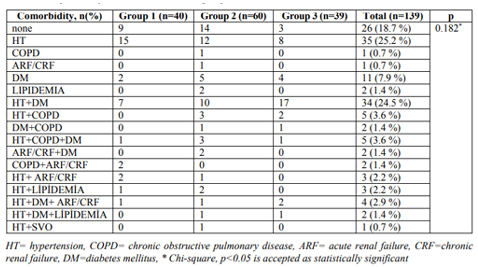
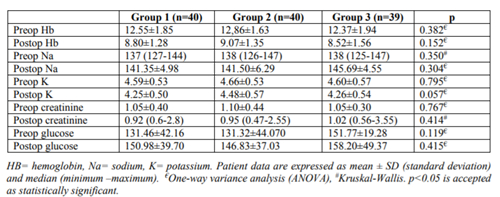
Results: The total group comprised 66.9 % males and 33.1% females (p = 0.001). Group 1 included 40 patients, Group 2, 60 patients, and Group 3, 39 patients. Surgery was elective in 89.9% and 10.1% were emergency, 79.1% of the operations were performed with pump, and 20.9% as beating heart surgery. While 18.7% of patients had no additional disease, hypertension was the most common comorbidity at 25.2%. Cross-clamp times were similar in groups. The duration of extubation was shorter in Group 1 (p = 0.042) compared to the other groups, and the operation times were longest in Group 2 (p= 0.041). There was no difference between the groups in terms of inotropic support / IABP / pacemaker use. No difference was observed between the groups in terms of length of stay in intensive care stay and in hospital (p = 0,472, p = 0.609). There were no significant differences in postoperative complications of rhythm disturbances, renal failure, and SVO, but there was a significant difference in terms of infection (p = 0.041) between the groups. Mortality was seen in 18% of the whole patient group with no difference determined between the sub-groups (p = 0.670).
Conclusion: Contrary to expectations, obesity may not increase mortality in cardiac surgery in elderly patients, but may lead to an increase in extubation times and the development of infection during the recovery period.
obese, elderly, anesthesia, cardiac surgery, Anesthesiology
As the prevalence of obesity increases worldwide, an increasing number of obese surgical patients will require anesthesia. Obesity is typically defined by body mass index (BMI), the ratio of weight (in kilograms) to the square of height (in meters). In adults, the World Health Organization and the National Institute of Health define overweight as a BMI of 25 to 29.9 kg m2 -1, obesity as a BMI of ≥30 kg m2 -1 and severe obesity is defined as a BMI ≥40 kgm2 -1 (or ≥35 kg m2 -1 in the presence of comorbidities)[1].
Obesity is a disease that affects many organ systems, especially the cardiovascular and respiratory system. Cardiovascular diseases are the leading problems in elderly patients.
Due to the increase in the average life expectancy and the higher incidence of cardiovascular disease with advancing age, an increasing number of elderly patients undergo cardiac surgery and the number has gradually increased over the last 10 years [2].
Although there have been studies investigating cardiac surgery and the anesthetic approach in elderly patient populations, there has been no research about obese elderly patients undergoing cardiac surgery.
The aim of this study was to evaluate the mortality and morbidity rates of cardiovascular surgery in elderly, obese patients.
2. Methods
The hospital records and files of patients aged>65 years (n=139) who underwent open heart surgery between January 2014-2017 were retrospectively examined.
Demographic data, types of surgery, comorbidities, laboratory values, postoperative complications, intensive care and hospital stay, and mortality rates were recorded and compared between patients grouped according to body mass index (BMI): Group 1 (BMI <25), Group 2 (BMI = 25-30) and Group 3 (BMI ≥30).
3. Statistical Analysis
IBM SPSS Statistics version 20 software was used for all statistical analyses. Data were expressed as mean±standard deviation. The Mann–Whitney U test and Student’s t-test were applied in the comparisons of quantitative data. The Chi-square test was used to compare categorical variables. A value of p <0.05 was considered statistically significant.
4. Results
The data related to a total of 341 patients who had undergone open heart surgery in the 3-year period of January 2014-2017 were retrieved from the hospital data system. Of these, 139 patients aged 65 years and older were included in the study. These patients were then separated into three groups based on BMI: Group 1 (n= 40, BMI < 25), Group 2 (n=60, BMI = 25-30) and Group 3 (n=39, BMI ≥30).
The mean age of the patients was 73 years in Group 1, 72 years in Group 2 and 70 years in Group 3. No significant difference was determined between the groups in respect of age (p=0.260, Table 1). Male gender (66.9 % of all patients) was significantly higher than female gender (33.1 % of all patients) in the study groups (p=0.001, Table 1).
Surgical procedures were divided into coronary artery bypass graft (CABG), valve operations (V), V+CABG and dissections. Among these procedures, the most common procedure in all the groups was CABG operations (109 patients), and there was no difference in the type of operation between the groups (p=0.922, Table 2). Surgery was elective in 89.9% of cases, whereas 10.1% were under emergency condions (Table 1), 79.1% of the operations were performed with pump and 20.9% as beating heart surgery (Table 1). The duration of surgery was longer in Group 2 than in the other groups, and cross-clamp time was similar in all 3 groups (p= 0.041, p= 0.212, Table1). Extubation times were shorter in Group 1 than in the other groups (p = 0.042, Table 1).
Of the comorbidities observed, hypertension was the most frequently seen comorbidity (25.2 %, Table 3), in 15 patients in Group 1, 12 in Group 2 and 8 in Group 3. The second most common comorbidity was hypertension and diabetes together (24.5 %, Table 3). There was no significant difference between the groups in terms of preoperative and postoperative hemoglobin, potassium, sodium, creatinine and blood glucose levels (Table 4).
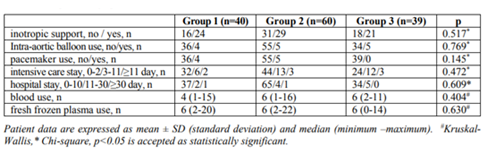
There was no difference between the groups regarding inotropic support / IABP / pacemaker use (Table 5). No significant difference was determined between the groups in terms of length of stay in intensive care unit stay and hospital (p = 0. 472, p = 0.609, Table 5).
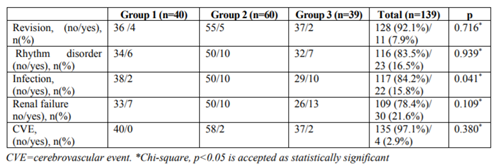
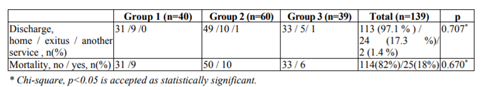
Postoperative complications of rhythm disturbances, renal failure and CVO were similar in all the groups, but there was a significant difference in terms of infection development (p = 0.041, Table 6). Mortality was determined in 18% of all patients, with no difference determined between the groups (p = 0.670) (Table 7).
5. Discussion
According to the data for 2010, the population aged 65 years and older constituted 7% of the total population of Turkey, and this is expected to rise to 12-13% within the next 10 years [3]. Aging is a process in which pathological findings increase together with a decrease in the physiological reserve. Therefore, risk factors that increase perioperative mortality and morbidity should be researched and patients should be prepared for the operation in the best way [4].
Obese individuals appear to be at a higher risk of perioperative complications concerning all organ systems. In a previous study, tobacco use, malnutrition and high body mass were reported to be the most important predisposing factors for ischemic heart disease and diabetes [3]. When the patient profiles in this study are examined, the number of patients with BMI <25 was 40 and the number of patients with BMI >25 was 99, and this may be an indication that obese patients need more cardiac surgery. The number of male patients (66.9 % of all patients) was significantly higher than females (33.1 % of all patients) in the study groups, which was consistent with literature [5].
Obesity may be associated with many diseases such as hypertension, dyslipidemia, ischemic heart disease, diabetes, osteoarthritis, liver diseases, asthma and sleep-apnea syndrome [6]. In obese patients, blood flow, cardiac output, oxygen consumption and production of carbon dioxide are known to be increased, which may lead to systemic and pulmonary hypertension, cor pulmonale and right ventricular failure. Left ventricular dilatation, increased left ventricular wall stress and hypertrophy cause reduced left ventricular compliance resulting in heart failure [6]. Hypertension and tachycardia, which will increase the oxygen consumption of the myocardium, are the most important issues to be considered in cardiac anesthesia in elderly patients. Stable anesthesia induction and maintenance without allowing hypotension must be provided for coronary perfusion. The pharmacodynamic and pharmacokinetic properties of drugs vary with aging. Increasing the dispersion volume and a decrease in total body fluid by increasing the body fat ratio may result in sudden and destructive complications [7]. In the present study, hypertension was the most seen comorbidity, as expected.
An increased risk for surgical complications in patients with obesity has been reported in several studies. These complications include longer operative times [8-10], possibly increased blood loss[8-10], and increased rates of infection [10,11]. Infectious complications are a particular concern in patients with obesity. An analysis of ACS-NSQIP data in 16 major cardiovascular, orthopedic, and oncology surgeries found that BMI of at least 40 kg m2-1 significantly increased the odds for wound complications in all surgeries analyzed except for pneumonectomy [12]. Contrary to literature, the operation times in the current study were shorter in obese patients, whereas the duration of extubation was shorter in non-obese patients. There was no difference in blood usage or labaratory findings between the groups.
Despite evidence of increased medical and surgical complications in the obese surgical population, the effect of obesity on mortality is unclear. Although some surgical literature suggests that any increase in BMI above normal is associated with decreased survival [11,13], other publications have suggested an obesity paradox, where limited increases in BMI (in the 25–40 kg m2-1 range) may provide a survival benefit compared with normal weight patients [12,14-16]. Multivariate analysis of 78,762 Canadian CABG and combined CABG and aortic valve replacement patients found a survival advantage for patients with BMI of 25– 29.9 kg m2-1 and no difference for patients with BMI of 30–34.9 kg m2-1 compared with normal weight patients. Increased mortality was only observed in those with BMI >34.9 kg m2-1 and underweight patients (BMI< 20 kg m2-1) [14]. In a study in which the quality of life and early and mid-term results were evaluated in patients aged 80 years and older, there was no negative effect of age on mortality or morbidity in advanced elderly patients in preoperative ejection fraction, coronary and valvular surgery. Preoperative creatinine values were also shown to provide more meaningful information on mortality and morbidity [17]. In the current study, there was no obesity-related increase in mortality. However, it should be kept in mind that obesity is a part of metabolic syndrome and a comorbidity [11,12,14].
In conclusion, in contrast to expectations, obesity, which is an increasing comorbidity among elderly patients, may not increase mortality in cardiac surgery. Nevertheless, it is important that it is considered and managed by anesthesiologists because of the associated diseases.
References
- uptodate Obesity in adults: Overview of management. Available at: http://0210026l9.y. https.www.uptodate.com.proxy.afyon.deep-knowledge.net/contents/obesity-in-adults-over view-of-management? Accessed Nov 5, 2018.
- Friedrich I, Simm A, Kotting J, Tholen F, Fischer B, Silber RE. Cardiac surgery in the elderly patient. Dtsch Arztebl Int 2009; 106: 416-22.
- T.C. Sağlık Bakanlığı Sağlık İstatistikleri Yıllığı 2015. Ankara: 2016. Available at: http:// www.saglikistatistikleri.gov.tr/dosyalar/SIY_ 2015. pdf. Accessed Nov 10, 2018.
- Frilling B, von Rentein-Kruse W, Riess FC. Prognostic value of geriatric assessment prior to cardiac surgery of the elderly. JACC 2009; 53: A403-18.
- Kaya M, İyigün T, İyigün M, Bakır İ, Yeniterzi M. The results of coronary artery surgery in women and men under the age of 45. Turkish Journal of Cardiovascular and Thoracic Surgery 2013;21(3):581-7. DOI : 10.5606/tgkdc.dergisi. 2013.7564
- Baturay F, Topuz C, Ay A, Gültop F. Obesity and anesthesia. Okmeydanı tıp Dergisi 2014;30:29-33.
- Gümüş F, EralpK, Kayalar N, Alagöl A. Cardiac surgery and anesthesia approach in an elderly patient population. Turkish Journal of Cardiovascular and Thoracic Surgery 2013; 21 (1): 250-5 DOI: 10.5606/tgkdc.dergisi.2013. 6947
- Hede P, Sorensson MA, Polleryd P, Persson K, Hallgren T. Influence of BMI on short-term surgical outcome after colorectal cancer surgery: a study based on the Swedish national quality registry. Int J Colorectal Dis 2015; 30:1201–7. https://doi.org/10.1007/s00384-015 -2280-0.
- Saiganesh H, Stein DE, Poggio JL. Body mass index predicts operative time in elective colorectal procedures. J Surg Res 2015; 197:45–9.
- Tjeertes EEKM, Hoeks SSE, Beks SSBJC,Valentin TM, Hoofwijk AG, Stolker RJ. Obesity: a risk factor for postoperative complications in general surgery? BMC Anesthesiol 2015;15:112. doi: 10.1186/s12871-015-0096-7.
- Ward DT, Metz LN, Horst PK, Kim HT, Kuo AC. Complications of morbid obesity in total joint arthroplasty: risk stratification based on BMI. J Arthroplasty 2015;30:42–46. doi: 10.1016/j.arth.2015. 03.045.
- Sood A, Abdollah F, Sammon JD, Majumder K, Schmid M, Peabody JO, et al. The effect of body mass index on perioperative outcomes after major surgery: results from the National Surgical Quality Improvement Program (ACS-NSQIP) 2005-2011. World J Surg 2015; 39:2376–2385. doi: 10.1007/ s00268-015-3112-7 (PMID:26059407)
- Benedetto U, Danese C, Codispoti M. Obesity paradox in coronary artery bypass grafting: myth or reality? J Thorac Cardiovasc Surg 2014; 147:1517–1523.
- Johnson AP, Parlow JL, Whitehead M, Xu J, Rohland S, Milne B. Body mass index, outcomes, and mortality following cardiac surgery in Ontario, Canada. J Am Heart Assoc 2015; 4: doi: 10.1161/JAHA. 115.002140.
- Valentijn TM, Galal W, Hoeks SE,von Gestel YR, Verhagen HJ, Stolker RJ. Impact of obesity on postoperative and long-term outcomes in a general surgery population: a retrospective cohort study. World J Surg 2013; 37:2561–2568. doi: 10.1007/s00268-013-2162-y.
- Valentijn TM, Galal W, Tjeertes EKM, Hoeks SE, Verhagen HJ, Stolker RJ. The obesity paradox in the surgical population. Surgeon 2013; 11:169–176. doi: 10.1016/j.surge.2013. 02.003
- Kara İ, Ay Y, Köksal C, Aydın C, Yanartaş M, Yıldırım T. The quality of life after cardiac surgery in octogenarians and evaluation of its early and mid-term results. Anadolu Kardiyol Derg 2012; 12: 352-8. (PMID:22484713).