Information
Journal Policies
Comparing the Effects of Spinal Anesthesia and Peripheral Block Applications against Postoperative Stress and Inflammatory Response on Patients Undergoing Total Knee Arthroplasty
Serdar Ozkul1, Elif Dogan Baki1*, Ozal Ozcan2, Halit Bugra Koca3, Remziye Sivaci1
2.Afyon Kocatepe University, Department of Orthopaedics and Traumatology, Turkey.
3.Afyon Kocatepe University, Department of Biochemistry, Turkey.
Copyright : © 2018 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Serious of neuroendocrin, metabolic and inflammatory changes that occur for protection of homeostasis after surgical trauma creates stress and inflamatuary response. The aim of this prospective study is to investigate the effects of spinal and peripheral block anesthesia on the postoperative stress response and inflammation on patients undergoing artroplasthy. Additionally, the role of these methods on intraoperative and postoperative pain control were investigated.
Forty eight patients undergoing elective knee arthroplasty were included in this prospective randomized study. Patients were randomly allocated to receive either spinal anesthesia (group S, n = 24) or peripheral block (group P, n= 24), for maintenance of anesthesia. The blood samples for TNF-α, IL-8, IL-6 ACTH, cortisol, glucose and insulin were taken preoperatively (T0), 1st hours postoperatively (T1) and 24th hours postoperatively (T2).
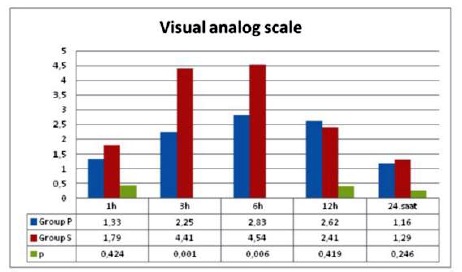
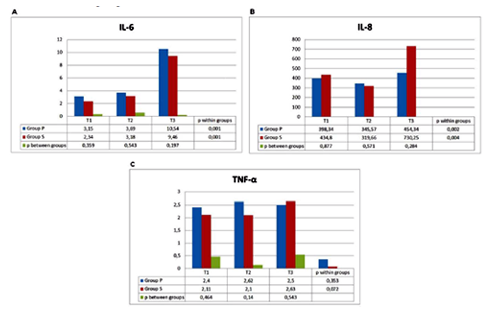
There was no statistical difference in ACTH, insulin and glucose levels between groups whereas postoperative 24 hour cortisol levels were significantly lower in Group P patients than Group S patients. There was no statistically significant difference in TNF-α, IL-6 and IL-8 levels between the groups. IL-6 and IL-8 levels increased significantly postoperatively in both within groups compared to preoperative values, but no significant change was detected in postoperative TNF-α levels. Postoperative VAS levels were significantly lower in the peripheral group than spinal group.
Peripheral block can be preferred in arthroplasty operations because it may have advantages such as providing longer time analgesia in the postoperative period, minimizing postoperative analgesia consumption and less stress response.
Spinal anesthesia; peripheral block; arthroplasty; stress response; inflammatory response.
The hypothalamic-pituatry-adrenal (HPA) axis is a neuroendocrine system that regulates circulating levels of glucocorticoid hormones and has multiple effects on almost all tissues of the body and plays a crucial role in regulating inflammation (Gibbison et al., 2013). Inflammation is important for tissue reconstruction, but excessive can have hazardous effects which lead to postoperative complications, such as postoperative infections, wound healing disturbances, prolonged hospital stay, increased health cost or organ dysfunctions (Milosavljevic et al., 2014; Orosz et al., 2012). Total knee artroplasty (TKA) is one of the most commonly performed orthopedic procedures (Alden et al., 2010). It is a major surgery and might induce an increased inflamatuary response compared to some minor surgeries. Anesthesia was reported to contribute inflamatuary response too (Milosavljevic et al., 2014). Therefore to prevent morbidity, it is important to reduce excessive inflamatuary and stress response induced by TKA and anesthetic methods.
Neuroaxial and other regional anesthetic techniques play a significant role in reducing the incidence of perioperative thromboembolic complications and neuroendocrine stress response to surgery, providing postoperative analgesia, and simplifying early rehabilitation and hospital discharge in patients undergoing orthopedic procedures (Marino, 2013).
To the best of our knowledge, few studies in the literature investigated the effects of anesthesia tecniques on the stress and inflamatuary response induced by TKA (Sağlık et al., 2015; Eroğlu et al., 2016). Therefore in this study, we aimed to compare the stress and inflamatuary response developing after TKA performed under spinal or peripheral block anesthesia.
2. Methods
This study was performed at an Anesthesiology and Reanimation Department of a University hospital between June 2016 and June 2017. Approval was obtained from the local Ethics Board of the Medical School. Preliminary information about the study was provided to the candidate participants who were then provided with the detailed information through an ‘informed voluntary concent form’ and signed the form.
Forty-eight patients aged between 20-80, who were planned to undergo total knee arthroplasty and had an American Society of Anesthesiologists (ASA) score from 1 to 2, were included in this study.
Those patients with hemorrhagic diathesis, who had comorbid diseases such as drug allergy, diabetes mellitus, uncontrolled hypertension, severe arrhythmia; and patients with a history of hepatic or renal failure, local / systemic infections, were excluded from the study.
Before the surgery, patients were randomly assigned to get either peripheral block (Group P, n=24) or spinal anesthesia (Group S, n=24) for the maintenance intraoperatively using a sealed envelope system. The first case of day was included in the study for measurements of endocrine parameters to comply with diurnal rhythm. All patients were operated by the same surgeon using the same surgical method and tourniquet was used during the surgery. The visual analog scale (VAS) and the patient-controlled analgesia (PCA) device were clarified to all patients during preoperative visit.
Patients in both groups received midazolam before surgical procedures. On arrival in the operating room, patients were monitored (Datex-Ohmeda Avance, G Healthcare, Helsinki, Finland) with continuous electrocardiography, pulse oximetry, and non- invasive blood pressure. Ringer’s Lactate was given intravenously (2 mL kg-1 sa-1) and maintained with an infusion of 4 mL kg-1 sa-1.
In group S, spinal block was performed with the patients lateral position and bupivacaine 0.5% (1.5 ml, 7.5 mg) was injected through L3-L4 /L4-L5 intervertebral space using a 25 gauge spinal needle, they were kept in this position until the adequate anesthesia level reached T12 (max. 10 min).
In Group P, a combined sciatic-femoral nerve block was applied with a 40 cc mixture (0.5% bupivacain 1.5 mg kg-1 + Aritmal 2 mg kg-1 + SF) adjusted to the total kilograms of the patients. With the patient positioned supine, the femoral artery pulse is palpated at the level of the inguinal ligament. A short (5-cm) insulated needle is inserted at a 45° angle to the skin in a cephalad direction until a clear quadriceps twitch is elicited at a current below 0.5 mA (look for patella motion), 20 ml of mixture was administered (8). For the blockade of sciatic nerve, the patient is positioned laterally with the side to be blocked in the nondependent position. The patient is asked to bend the knee of the affected leg and tilt the pelvis slightly forward (Sim’s position). The greater trochanter, posterior superior iliac spine (PSIS), and sacral hiatus are then identified. A line is drawn from the greater trochanter to the PSIS, its midpoint identified, and a perpendicular line extended in a caudal direction. Next, a line is drawn from the greater trochanter to the sacral hiatus and the intersection point is marked; this is the initial needle insertion point. A long (10-cm) insulated needle is inserted at an angle perpendicular to all planes to the skin. The needle is advanced through the gluteal muscles (a motor response of these muscles may be encountered) until plantar-flexion is elicited. A local anesthetic volume of 20 mL was administered (Marino, 2013).
When the patient had no pain with the pin-prick test and the Bromage Scores were above 3 in both groups, the surgeon was allowed to start the surgery (Bromage 1 (partial block), can only move the knee and legs, can not lift the leg straight, Bromage 2 (almost full block), the index is perfect, it can only move the leg, Bromage 3 (complete block), cannot move foot joint or bowel movements, has full paralysis).
Patient characteristics and perioperative events (blood usage, duration of anesthesia, and surgery, tourniquet use) were recorded. Hemodynamic parameters including mean arterial pressures (MAP), heart rate (HR) were noted intraoperatively. By an anesthesiologist, 10-cm VAS (0 =no pain, 10= maximal pain) was used for the assessment of pain at the 1th, 3th, 6th, 12th, and 24th hours at rest postoperatively.
At the end of the surgery, 1 g paracetamol and 1 mg/kg tramadol were given to all patients, and tramadol PCA (400 mg tramadol [8 mL] +saline [92 mL]) with 10 mg continuous, 20-mg demand dose and 30-minute lockout time was set for all patients in recovery room and maintained throughout the postoperative period. The total doses of tramadol were recorded from the PCA device’ history 24 hours after the procedure. Routine use of intravenous paracetamol twice a day (intravenous infusion) and nonsteroidal anti-inflammatory drugs twice a day (intramuscular) were given for the rescue treatment when the VAS score was over 4 at rest in both groups. If their analgesia was adequate, rescue analgesics would not be given at their routine given times. When the patient noticed strong pain (VAS was over 4) despite these treatments, intravenous infusion of meperidine 20 mg was given. Additional analgesic requirements were noted.
Venous blood samples for Adrenocorticotropic hormone (ACTH), cortisol, glucose, insulin, tumor necrosis factor alpha (TNF-α), interleukin-6 (IL-6), IL-8 were obtained from all patients before induction to anesthesia (T1), first hours postoperatively (T2), and 24 hours postoperatively (T3).
Venous blood samples were centrified at 5000 rpm for 10 minutes immediately after collection and plasma aliquots were stored at -20 C until assayed. Plasma concentrations of TNF-α, IL-6 and IL-8 were measured using e Bioscience Human Platinum enzyme-linked immunosorbent assay kits (Bender Med Systems GmbH, Vienna Australia). Absorbance detection was performed using ChemWell® 2910 Analyzer (Awareness Technology, Inc. Martin Hwy. Palm City, USA). The results were given as pg mL-1.
Cortisol, ACTH, insulin levels were measured by electrochemiluminescence immunoassay (Roche Modular EVO E-170 hormone autoanalyser) and glucose level by UV test method (Roche Hitachi P 1600 autoanalyser).
Power analysis was conducted using G*Power 3.1.9.2 package program to determine the number of observations. The size of the sample required for the three replicate measurements was determined as 42, with effect size=0.5 (medium), α=0.05, power=80%. However, 48 patients were planned to be included when patients had a 15% dropout rate. %. Statistical analyses of the study data were made using Statistical Package for Social Sciences (SPSS) for Windows 20.0 software. The Shapiro Wilk test was used to verify normal data distribution. Data were expressed as mean±standard deviation (SD), median (min-max) and percentages. Continuous variables were analyzed using the Student’s t test or the Mann-Whitney U test for parametric and non parametric data, respectively. Categorical variables were analyzed using the Chi-Square test or Fisher Exact test. When comparing data within groups, the Friedman test was used as a non-parametric test and the Paired-samples test as a parametric test. The results were evaluated in a confidence interval of 95% and at a significance level of p < 0.05.
3. Results
All 48 patients included in the study completed the study.
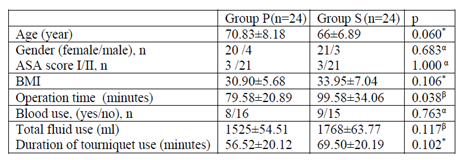
There were no significant differences between the groups with respect to demographic and intraoperative data except the operation time (Table 1). Operation time was statistically shorter in Group P than Group S (p=0.038, Table 1).
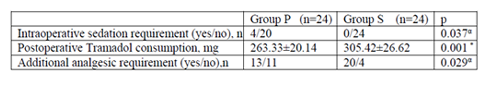
Intraoperative sedation requirement was not needed in Group S while 4 patients were in Group P. This was statistically significant between the groups (p = 0.037, Table 2). Postoperative tramadol use was 263.33 ± 20.14 mg in Group P and 305.42 ± 26.62 mg in Group S and this was statistically significant (p = 0.001, Table 2). When we compared the groups in terms of additional analgesia consumption, the use of additional analgesics in the peripheral group was lower than in the spinal group (p = 0.029, Table 2).
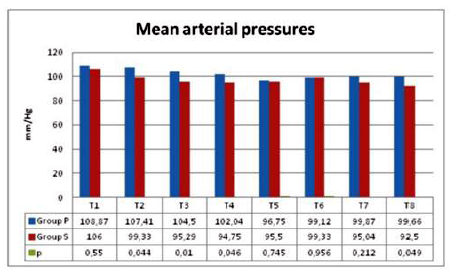
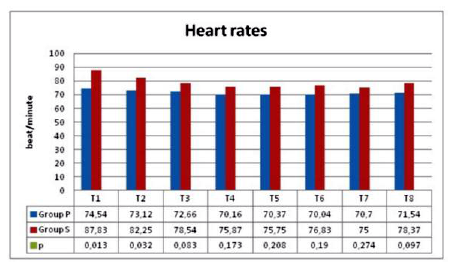
When the mean arterial pressures of the groups were compared in terms of changes in operation, values at T2, T3, T4 and T8 were significantly lower in Group S than Group P (p = 0.044, p = 0.010, p = 0.046, p = 0.049, Figure.1). When we looked at the heart rates compared between the groups, except values measured at T1 and T2, heart rates were not different at other times (p = 0.013, p = 0.032, Figure. 2).
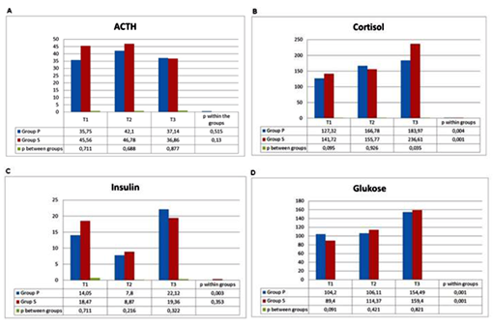
The perioperative ACTH, cortisol, insulin and glucose levels of the patients were shown in Figure. 4a, Figure. 4b, Figure. 4c and Figure. 4d, respectively. ACTH levels increased in postoperative 1st hour in both groups and decreased in postoperative 24th hours. There was no statistically significant difference between the groups and within the groups (Figure. 4a)
Postoperative cortisol levels were significantly higher than the preoperative values within both groups (Figure. 4b). When cortisol levels between groups were examined, cortisol level was significantly lower in Group P compared to Group S at 24 hours postoperatively. (p = 0.035, Figure. 4b).
Postoperative insulin levels were significantly higher than preoperative values in the peripheral group, but no significant differences were found in the spinal group (Figure. 4c). There was no significant difference in postoperative results between both groups (Figure. 4c).
Postoperative glucose levels in both groups were significantly higher than the preoperative values, but no difference was found between the groups (Figure. 4d).
IL-6, IL-8 and TNF- α levels of the patients were shown in Figure. 5a, Figure. 5b and Figure. 5c, respectively. There was no statistically significant difference in IL-6, IL-8 and TNF-α levels between the groups. IL-6 and IL-8 levels increased significantly postoperatively in both groups compared to preoperative values, but no significant change was detected in postoperative TNF-α levels (Figure.5a-b-c).
4. Discussion
A series of neuroendocrine, metabolic and inflammatory changes that occur after surgical trauma and protect homeostasis produce a stress response (Gibbison et al., 2013; Fant et al., 2013). It was previously reported that the changes in inflammatory response were not different in regard to anesthetic method between the groups undergoing minor surgery (Bravo-Cuéllar et al., 2007). However the effect of anesthetic methods on inflammatory response following major surgeries have not been clarified. Decreasing excessive inflammatory response after major surgeries such as artroplasty, by using appropiate anesthetic methods may provide clinical benefits. Although several studies investigated the effect of anesthetic methods on inflammatory response (Schilling et al., 2011; Chloropoulou et al., 2013; Høgevold et al., 2000), to our knowledge, there are no studies that evaluate the effect of spinal and peripheral block anesthesia on inflammatory and stress response following TKA.
Minimal changes were seen from the results of present study in terms of the anesthetic methods; a) postoperative 24 hour cortisol levels were significantly lower in Group P patients than Group S patients, b) no statistically significant difference were seen in TNF-α, IL-6 and IL-8 levels between the groups, c) IL-6 and IL-8 levels increased significantly postoperatively in both groups compared to preoperative values, but no significant change was detected in postoperative TNF-α levels, d) postoperative VAS levels and analgesic consumption were significantly lower in the peripheral group than spinal group.
Cortisol and ACTH secretion are sensitive indicators of stress response (Marana et al., 2010). Surgery is one of the strongest stimulants of ACTH and cortisol secretion, and the plasma levels of these hormones increase within minutes after the surgeon starts. As the level of ACTH normally needs to decrease due to increased levels of cortisol, this control mechanism may deteriorate after surgery and the level of both hormones may increase. In this study, ACTH levels increased in postoperative 1st hour and suppressed at 24th hours postoperatively due to elevated cortisol secretion in both groups Also cortisol levels were significantly higher in Group S than in Group P patients at 24 hour postoperatively.
After surgery, the elevation of catecholamines increases the concentration of glucose by glucogenolysis and gluconeogenesis. Elevation of glucose stimulates the secretion of insulin, insulin is anabolic, provides glucose utilization and glycogen production, reduces lipolysis and protein degradation. During trauma, this mechanism may be inadequate and in the organism, insulin resistance, a functional insulin insufficiency develops (Burton et al., 2004). Studies have shown that insulin sensitivity decreases of up to 50% (Sato et al., 2010). The insulin resistance depends on the size of the surgery. Hip and knee arthroplasties are those with high stress response. Our study showed that both spinal anesthesia and peripheral block applications prevented the increase of insulin level in postoperative first hour but not in postoperative 1st day.
The vascular and cellular responses of inflammation are mediated by chemical factors that arise from plasma cells and that are mediated by an inflammatory stimulus. Such chemical mediators act in combination or in sequence, affecting the formation of an inflammatory response (Mullington et al., 2001).
Inflammation and repair are the inner defense mechanisms of the body. Inflammatory is trying to repair the damaged tissue by destroying the effect, removing it from the environment, limiting inflammation. However, due to hypersensitivity reactions, increased reactive inflammatory response may cause impaired organ function or failure or even sudden death, as a complication of inflammation (Wedel, 2000). The number of chemical mediators that mediate the production of inflammatory tissue responses is increasing. Mediators are a variety of chemical substances that originate from damaged tissue, cells, or plasma. Cytokines are mediators composed of many cell types such as CD4+ T lymphocytes and active macrophages. Cytokines are polypeptide constructs and the most important in inflammation are interleukins (IL) and tumor necrosis factor-alpha (TNF-α) (Kurulay and Çavdar, 2006). Surgical stress and suppression of the inflammatory response may positively affect postoperative outcomes (Marana et al., 2010; Burton et al., 2004). Anesthesia methods are also used to modify the surgical stress response (Marana et al., 2010). Sağlık et al. (2015) investigated the effects of adrenocorticotropic hormone (ACTH), cortisol, glucose, and insulin on blood pressure and hemodynamic effects in studies investigating the effects of epidural anesthesia combined with general anesthesia on stress response in hip and knee arthroplasties. As a result, they concluded that epidural anesthesia combined with general anesthesia could suppress the stress response assessed by ACTH and cortisol levels, but could not prevent the elevation of insulin and glucose levels. In present study, it was found that the level of inflammatuary and stress mediators were high following TKA in both anesthetic method except cortizol levels. This may be due to better analgesia level in peripheral group. But operation times of spinal anesthesia group was significantly longer than peripheral group, this may change the results and this was the restrictive part of our study. In present study, although we kept the patient age group very large, the mean age in both groups was 65 years and over, and the female patients were in the majority and also BMI of the patients were high in both groups. This was the other restricting side of our work.
Regional anesthesia alone or combination with general anesthesia is used to provide satisfactory postoperative analgesia following major surgeries. The most common techniques used in this area are unilateral spinal anesthesia and combined sciatic femoral nerve block (Marino, 2013). Peripheral nerve blocks provide optimal outpatient anesthesia conditions for orthopedic surgery. There are studies showing that the combined sciatic-femoral nerve block and combined lomber plexus-sciatic nerve block have superior postoperative recovery profile compared to general anesthesia in daily knee surgery and reduced frequency of re-admission to the hospital (Williams et al., 2003; Casati et al., 2000). Kurnaz et al. (2014) compared the results of unilateral spinal anesthesia and combined sciatic femoral block on hemodynamics, postoperative analgesia, and recovery in patients undergoing knee arthroscopy. As a result, the combined sciatic-femoral nerve block showed similar anesthetic efficacy with the same clinical profile as the low-dose unilateral spinal anesthesia, and similar to our results they showed that they provided more successful analgesia in terms of VAS values in the post-operative 24-hour period. Likewise Fanelli et al. (1998); in their studies comparing spinal block to combined sciatic-femoral block for foot and ankle surgeon; found that combined sciatic-femoral nerve block application was as safe and effective as spinal anesthesia and provided longer analgesia in the postoperative period.
Peripheral nerve blocks have important advantages over general anesthesia and central blocks, such as; less respiratory and hemodynamic effects (sympathetic block, hypotension, bradycardia), less anesthesia related complications, and shorter recovery period (Fanelli et al., 1998). When comparing the peripheral nerve blocks and spinal anesthesia, similar results were obtained in the literature only Spasiano et al. (1999) reported a significant difference in heart rate changes in studies comparing femoral sciatic block and spinal anesthesia, but opposed to other studies, reported that heart rate changes were higher in the femoral sciatic block group. They suggest that the changes in heart rate in block group was caused by the compensatory hemodynamic response to insignificant hypotension caused by vasodilatation in the operated part while the hemostatic response was partially inhibited in the spinal group. In our study, there was no significant change in the hemodynamic parameters in the peripheral group, while the OAB values and heart rate values in the spinal group were significantly lower than the peripheral group. The lower OAB in the spinal group was considered as a consequence of the better suppression of the surgical stress response by the inhibition of nociceptive stimuli with vasodilatation caused by spinal anesthesia.
Tourniquet use may result in skeletal muscle ischemia-reperfusion injury, and this increase the inflammatory response to surgery (Hughes et al., 2007; Clementsen and Reikeras, 2008). However the mean time for tourniquet use were similar between the groups in this study.
5. Conclusion
In conclusion, it is considered that peripheral nerve block application may be safer and advantageous because it provides postoperative long-term analgesia, less consumption of additional analgesia, less postoperative stress response in orthopedic lower extremity surgery.
References
- Alden, K.J., Duncan, W.H., Trousdale, R.T., et al., 2010. Intraoperative fracture during primary total knee arthroplasty. Clin. Orthop. Relat. Res. 468, 90-95.
- Bravo-Cuéllar, A., Romero-Ramos, J.E., Hernández-Flores, G., et al., 2007. Comparison of two types of anesthesia on plasma levels of inflammatory markers. Cir. Cir. 75, 99-105.
- Burton, D., Nicholson, G., Hall, G., 2004. Endocrine and metabolic response to surgery. Continuing education in anaesthesia. Critical Care and Pain. 4, 144-147
- Casati, A., Cappelleri, G., Fanelli, G., et al., 2000. Regional anaesthesia for outpatient knee arthroscopy: a randomized clinical comparison of two different anaesthetic techniques. Acta Anaesthesiol. Scand. 44, 543-547.
- Chloropoulou, P., Iatrou, C., Vogiatzaki, T., et al., 2013. Epidural anesthesia followed by epidural analgesia produces less inflammatory response than spinal anesthesia followed by intravenous morphine analgesia in patientswith total knee arthroplasty. Med. Sci. Monit.19, 73-80.
- Clementsen, T., Reikerås, O., 2008. Cytokine patterns after tourniquet induced skeletal muscle ischaemia reperfusion in total knee replacement. Scand. J. Clin. Lab. Invest. 68, 154-159.
- Eroğlu, M., Kokulu, S., Koca, H.B., et al., 2016. The effects of general and spinal anesthesia on systemic inflammatory response in patients undergoing total knee arthroplasty. Joint Diseases and Related Surgery. 27, 153-159.
- Fanelli, A., Casati, G., Aldegheri, P., et al., 1998. Cardiovascular effects of two different regional anaesthetic techniques for unilateral leg surgery. Acta. Anaesthesiol. Scand. 42, 80– 84.
- Fant, F., Tina, E., Sandblom, D., et al., 2013. Thoracic epidural analgesia inhibits the neuro-hormonal but not the acute inflamatory stress responcse after radical retropubic prostatectoy. Br. J. Anaesth . 110, 747-757.
- Gibbison, B., Angelini, G.D., Lightman S.L., 2013. Dynamic output and control of the hypothalamic-pituitary-adrenal axis in critical illness and major surgery. Br. J. Anaesth. 111, 347-360.
- Høgevold, H.E., Lyberg, T., Kähler, H., et al., 2000. Changes in plasma IL-1beta, TNF-alpha and IL-6 after total hip replacement surgeryin general or regional anaesthesia. Cytokine.12, 1156-1159.
- Hughes, S.F., Hendricks, B.D., Edwards, D.R., et al., 2007. Mild episodes of tourniquet induced forearm ischaemia-usion injury results in leukocyte activation and changes in inflammatory and coagulation markers. J. Inflamm. 4, 12.
- Kurnaz, M.M, Ersoy, A., Altan, A., et al., 2014. Comparison of hemodynamics, recovery profile and postoperative analgesia of unilateral spinal anaesthesia with combined sciatic-femoral nerve block in knee arthroscopy. Ağrı. 26,171-178.
- Kurulay, F., Çavdar, Z., 2006. A global view to inflammatory mediators. Genel Tıp Derg. 16, 143-152.
- Marana, E., Colicci, S., Meo, F., et al., 2010. Neuroendocrin stress response in gynecological laparoscopy: TIVA with propofol versuss sevoflurane anesthesia. J. Clin. Anesth. 22, 250-255.
- Marino, E.R., 2013. Anesthesia for orthopedic surgery, In: Butterworth, J.F., Mackey, D.C., Wasnick, J.D. (Eds). Morgan& Mikhail’s Clinical Anesthesiology, 5th edition, Lange, Mc Graw Hill, USA, pp. 789-801.
- Marino, E.R., 2013. Spinal, epidural&caudal blocks, peripheral nerve blocks. In: Morgan& Mikhail’s Clinical Anesthesiology, Butterworth, J.F., Mackey, D.C., Wasnick, J.D. (eds)., 5th edition, Lange, Mc Graw Hill, USA, pp. 937-1023.
- Milosavljevic, S.B., Pavlovic, A.P., Trpkovic, S.V., et al., 2014. Influence of spinal and general anesthesia on the metabolic, hormonal, and hemodynamic response in elective surgical patients. Med. Sci. Monit. 20, 1833-1840.
- Mullington, J.M., Hinze-Selch, D., Pollmavher, T., 2001. Mediators of inflammation. Ann. N. Y. Acad. Sci. 933, 201-210.
- Orosz, J.E., Braz, M.G., Golim, M.A., et al., 2012. Cytokine profile in patients undergoing minimally invasive surgery with balanced anesthesia. Inflammation. 35, 1807-1813.
- Sağlık, Y., Yazıcıoğlu, D., Çiçekler, O., et al., 2015. Investigation of effects of epidural anaesthesia combined with general anesthesia on the stress response in patients undergoing hip and knee artroplasty. Türk. J. Anaesth. Reanim. 43,154-161.
- Sansone VDe Ponti, A., Fanelli, G., Agostoni, M., 1999. Combined sciatic and femoral nerve block for knee arthroscopy: 4 years' experience. Arch. Orthop. Trauma Surg. 119, 163-167.
- Sato, H., Carvalho, G., Sato, T., et al., 2010. The association of preoperative glycemic control, intraoperative insulin sensitivity, and outcomes after cardiac surgery. J. Clin. Endocrinol. Metab. 95, 4338-4344.
- Schilling, T., Kozian, A., Senturk, M., et al., 2011. Effects of volatile and intravenous anesthesia on the alveolar and systemic inflammatory response in thoracic surgical patients. Anesthesiology.115, 65-74.
- Wedel, J.D., 2000. Nerve blocks. In: Miller RD, ed. Anesthesia 4th edition, Philadelphia, pp. 1520-1548.
- Williams, B.A., Kentor, M.L., Vogt, M.T., et al., 2003. Femoral-sciatic nerve blocks for complex outpatient knee surgery are associated with less postoperative pain before same-day discharge: a review of 1,200 consecutive cases from the period 1996-1999. Anesthesiology.98, 1206-1213.