Information
Journal Policies
Intraoral Finger Stabilization of Proseal LMA for Adequate Rescue in cannot Ventilate, cannot Intubate and cannot be Tracheostomized Situation
Sanjay Kumar1,Habib Md Reazaul Karim2,Anilkumar Narayan3,Kriti Chaudhary4
2.Associate Professor, Department of Anaesthesiology, Andaman & Nicobar Islands Institute of Medical Sciences, Port Blair, India.
3.Ex-Senior Resident, Department of Anaesthesiology, Andaman & Nicobar Islands Institute of Medical Sciences, Port Blair, India.
Copyright : © 2017 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Airway management of an infant is challenging. Neck swelling or neck space infection also poses difficulty in airway management by distorting the anatomy and an anaesthesiologist faces one of the toughest situations while securing the airway. We present here a case which landed up in to cannot ventilate, cannot intubate and cannot be tracheostomized situation. The airway was somehow managed using proseal laryngeal mask airway only after supported with intraoral finger insertion and pressure on the bowl part and the young life was saved. The case highlights the importance as well as limitation of laryngeal mask airway (LMA) in deformed anatomy with a point to ponder, how to deal with such situation preemptively in a resource limited setups?
Airway obstruction, airway devices, neck mass, emergency care, general anesthesia,Anesthesiology
1. Introduction
Airway of infant and pediatric age group differs significantly from an adult and poses unique challenges. [1] The challenge further increases when an infant presents with a neck swelling compromising the airway. Cervical lymphadenopathy in children is mostly due to inflammatory reasons, which can be bacterial, viral or reactive in origin. [2] If not treated properly and timely it becomes a serious threat to the airway and life. We present here a case which was posted for emergency incision and drainage (I&D) for a neck swelling crossing the midline. Airway management landed up in to cannot ventilate, cannot intubate and cannot be tracheostomized situation. The life was saved somehow using proseal laryngeal mask airway (LMA) supported with intraoral finger insertion and pressure on the bowl part. The case highlights the importance as well as limitation of LMA. It also leaves us with a pondering point ‘how to deal with such situation preemptively?
2.Case
An 11 month old infant, weighing 10 kilogram, presented to the emergency department with 15 day old neck swelling and fever. The swelling started in the left side and gradually increased in size extending to other side of neck crossing midline. The swelling had grown and worsened in last two days, covering entire left neck, angel of mandible and pretracheal region. The baby was toxic, heart rate 154 per min, respiratory rate 44 per minute and comfortable in mother lap in slight head-up position. There was mild stridor in the lying down and even in right lateral position. The swelling was tense, immobile and warm. Total leukocyte count 40,000/mm3 with 81% neutrophils and increased C - reactive protein. Chest X-ray excluded intra thoracic extension. Ultrasound neck showed multiple bilateral level I, II and III necrotic lymph nodes. The case was taken for emergency I&D. Thorough airway assessment was not possible due to swelling, oedema, age related limitations. Equipments for difficult airway, cricothyrotomy and emergency tracheostomy were kept ready. Experts for rescue tracheostomy were readily available.
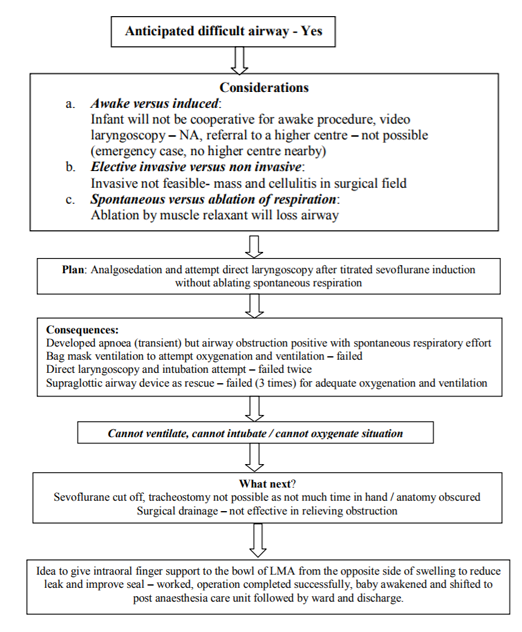
Intravenous (IV) line was secured with 22-Gauge cannula and connected to ringers lactate. Injection paracetamol 150 mg, midazolam 0.5 mg, atropine 0.2 mg, ondansetron 1 mg was given and baby shifted to operating table. Heart rate, oxygen saturation (SpO2), respiratory rate, temperature and electrocardiogram (ECG) were monitored. IV fentanyl 10 µg was given. Preoxygenation was done for 3 minutes, and general anaesthesia was induced by incremental sevoflurane with oxygen, but infant became apnoeic (transient) even in subanesthetic dose. Bag mask ventilation was inadequate and somehow maintaining oxygen saturation (SpO2) by 82%. Sevoflurane was cut off, respiratory effort came back but obstructive feature was evident. Despite an attempt to ventilate with 100% oxygen, with maximal extension, jaw thrust and two hand technique; the SpO2 started falling rapidly. Considering the limitation of time taken for tracheostomy and possible pus at incision site, it was decided to attempt once for tracheal intubation which was unsuccessful in the hand of two experienced anaesthesiologist. In a desperate attempt proseal LMA was placed (three times) but ventilation was grossly inadequate with failed oxygenation (evidences by capnography and improving SpO2 up to 85% with 100% oxygen). The surgeon was requested to give urgent nick and release the pressure. Meanwhile, LMA fixation was attempted but every attempt lead to compromised ventilation and fall in SpO2. Leak and malposition was evident. Only 5-6 ml of pus was drained and there was no improvement in swelling. Fixation removed and anaesthesiologists’ index finger was inserted from the opposite side of the prominent swelling and a pressure over the semi-inflated cuff and bowl of the LMA was tried to keep it over the glottic region and was found to be successful (figure 1). SpO2 improved to 100%, capnography showed acceptable carbon-di-oxide tracings (figure 2) and sevoflurane was re-started to complete the procedure without any further adverse events. The sequences of events are presented in the flow chart.
3. Discussion
The bag and mask ventilation is the fundamental skill in airway management. In children lateral position when combined with chin lift and jaw thrust improves airway patency. This has been demonstrated in children with adenotonsillary hypertrophy. [3] However, in the present case, lateral position, jaw thrust, head extension and even two hand techniques were not effective. Nasopharyngeal airways may be used to relive upper airway obstruction during mask ventilation.[4] In this case the obstruction was at the periglottic region which was unlikely to be relieved by airway. As per the guidelines recommendation the baby was supposed to be awakened. [5] In this case, it was not fruitful as the SpO2 started falling very rapidly and even spontaneous respiration was ineffective due to obstruction.
Patients with neck space infections often need tracheostomy; awake fibreoptic and even video laryngoscopy with preserved respiration for securing airway. Elective fiberoptic was not possible due to restless very young baby as well fear of losing airway with sedation. The present baby also developed transient apnoea which was probably because of Fentanyl and midazolam combination. Moreover, transient apnoea is also common in infants with intravenous as well as inhaled anaesthetics. Postponing the surgery was not an option at all and surgical airway was also not a good and easy method in this case due to distorted anatomy, infection at the site and time constraints. To provide adequate oxygenation needle cricothyrotomy is often a recommended procedure however it is not recommended in children under age 5 due to more complications. [8] Moreover, landmarks were obscured too in the present case.
Laryngeal mask airways are popular supraglottic devices; have proven safety and efficacy in pediatric population. [9]The classic LMA has a 95%-98% success rate in achieving adequate ventilation in children. [10] LMA has also been recommended as a rescue for cannot ventilate and cannot intubate situation. [5] We tried the LMA as a rescue and which was found to ineffective to ventilate optimally even after successful insertion for three times. The failure of the LMA was because of the distorted internal perilaryngeal anatomy which was evident by the postion of airway tube visible externally and evident suprasternal and intercostals space retractions. Despite being proseal LMA semi-rigid, its position was changed by the distortive forces and thus putting the finger in the opposite side served the purpose to be abled to ventilate and oxygenate better.
It is well known that LMA is helpful even in a situation of cannot ventilate cannot intubate situation. However, the relative flexible nature makes them prone to displacement and leaks. This case highlights this practical limitation in a situation where there is external growth pressing over the perilaryngeal area.
4. Conclusion
LMA, although is helpful in a cannot ventilate, cannot intubate and cannot be tracheostomized situation; it may not be adequate rescue in patients with neck swellings leading to distortion of perilaryngeal area. Putting a finger and pressing over the LMA bowl from the opposite side may be effective in proper placement of displaced LMA in life saving situation in such cases.
References
- Harless J, Ramaiah R, Bhananker SM. Pediatric airway management. Int J Crit Illn Inj Sci 2014; 4:65-70.
- Lang S, Kansy B. Cervical lymph node diseases in children. GMS Curr Top Otorhinolaryngol Head Neck Surg 2014; 13:Doc08. doi:10.3205/cto000111
- Arai YC, Fukunaga K, Hirota S, Fujimoto S. The effects of chin lift and jaw thrust while in the lateral position on stridor score in anesthetized children with adenotonsillar hypertrophy. Anesth Analg 2004; 99:1638-41.
- Holm-Knudsen R, Eriksen K, Rasmussen LS. Using a nasopharyngeal airway durin fiberoptic intubation in small children with a difficult airway. Paediatric Anaesth 2005; 15:839-45.
- Apfelbaum JL, Hagberg CA, Caplan RA, Blitt CD, Connis RT, Nickinovich DG, et al. Practice Guidelines for Management of the Difficult Airway: An Updated Report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology 2013; 118:251-70.
- Laskar HA, Karim HMR, Jamil M, Yunus M, Shunyu NB. Diversified and Unusual Presentations of Neck Space Infections: Still a Big Concern for Physicians. J Maxillofac Oral Surg 2015; 14:935-42.
- Sujatha MP, Madhusudhana R, Amrutha KS, Nupoor N. Anaesthetic management of Ludwig's angina with comorbidities. Indian J Anaesth 2015; 59:679-81.
- Weiss M, Engelhardt T. Proposal for the management of the unexpected difficult pediatric airway. Paediatric Anaesth 2010; 20:454-64.
- White MC, Cook TM, Stoddart PA. A critique of elective pediatric supraglottic airway devices. Paediatric Anaesth 2009; 19 (Suppl 1): 55-65.
- Mason DG, Bingham RM. The laryngeal mask airway in children. Anaesthesia 1990 45:760-3.