Information
Journal Policies
Inadvertent Dura Mater Puncture and Posterior Reversible
Encephalopathy Syndrome (P.R.E.S)
M. L. Lo Magno1,2*, G. Scarpinati3, F. Le Pira1,2, M. Zappia4, V.Carnemolla1,2,M. Astuto1,2
2.Scuola di Specializzazione in Neurologia, Università degli Studi di Catania, Italy.
3.U.O.C.Anestesia e Rianimazione 2, A.O.U. “Policlinico-Vittorio Emanuele”, Catania, Italy.
4.U.O.C. Neurologia, A.O.U. “Policlinico-Vittorio Emanuele”, Catania, Italy.
ARC Journal of Anesthesiology. 2017;2(1):4-6.
Copyright : © 2017 . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Posterior reversible encephalopaty syndrome (PRES) is a clinical entity with acute onset, which is characterized by a constellation of non-specific signs and symptoms, whose severity can vary. It is commonly related to headache and the risk factors include malignant hypertension, preeclampsia or eclampsia. The headache following the inadvertent dura mater puncture can delay the PRES diagnosis. We describe the case report of a primigravida woman who initially showed the typical signs of headache following the inadvertent dura mater puncture, which was done during the childbirth analgesia, and after 62 hours she had convulsive crises.
In the future, we deem to investigate repeated convulsive events within peri-partum with specific diagnostic assessments (RM) since they may represent a PRES that, if it is not accurately treated, it can progressively result in permanent and/or fatal neurologic consequences.
Keywords: Cerebrovascular, Vasogenic edema, Posterior reversible encephalopaty syndrome.
1. Introduction
Posterior reversible encephalopaty syndrome (PRES) is a clinical entity with acute onset, which is characterized by a constellation of non-specific signs and symptoms, whose severity can vary. It is commonly related to an acute blood pressure increase, headache, altered state of consciousness, convulsions and vision loss. Other less commonly observed symptoms include nausea, vomiting and deficit of the brain stem. Risk factors include: malignant hypertension, preeclampsia or eclampsia, immunosuppressive drugs (including tacrolimus and cyclosporin), chemotherapy, biotherapy and renal failure. Although Hinchey et al. have significantly recognized it since its initial description in 1996, the mentioned clinical entity is still poorly defined due to its wide clinical spectrum and its underlying pathophysiology. In addition to the presence of signs and symptoms described, a PRES clinical diagnosis foresees radiological findings of focal reversible vasogenic edema, visible on brain MRI. The edema affects the white matter in the posterior sides of the cerebral hemispheres,specifically, on the bilateral parietal-occipital regions. Usually, it is a reversible phenomenon, as the name suggests, but if it is not promptly identified and treated, the edema can cause permanent brain damages. The differential diagnosis must be carried out taking into account additional medical conditions such as cerebrovascular event, sinus thrombosis, demyelination, vasculitis and encephalitis.
2. PRES in Pregnancy
The PRES can be caused by agents that damage the endothelium of the blood-brain barrier (immunosuppressant, cytotoxic agents, endothelial toxins circulating in case of uremia, hemolytic uremic syndrome and thrombotic thrombocytopenic purpura) or by the hypertensive encephalopathy; however, also patients with sub-acute increase of pressure and/or with hyperactivity of the vascular bed may suffer from it. During pregnancy, eclampsia is the most common cause , however, it is still unclear whether there is a causal relationship between the two clinical conditions or if they only are two different processes with overlapping clinical features. According to some authors, pressure increase and endothelial dysfunction, which characterize the preeclampitc syndrome, might explain this association. Two different pathogenetic theories for the PRES are documented in literature. The oldest one suggests that the cerebral vessels react to the pressure increase with a reversible vasospasm, which causes ischemia, also reversible. The new theory regards hyperpefusion as the primary cause that follows the dilation of cerebral arterioles, due to a severe rise in systemic pressure that exceeds the limits of autoregulation of cerebral blood flow, which causes the leakage of fluid, red blood cells, and macromolecules from the vascular bed and the development of a vasogenic edema. In pregnancy, seizure disorders have an incidence of 0.5-2% and they are the leading cause of mortality and morbidity, both in developed and developing countries. Eclampsia is considered as the original cause until other causes are identified, being it characterized by seizures and /or coma, which occur in the third trimester of pregnancy, in labor or within seven days since the birth. However, other causes such as epilepsy, encephalitis, and tumors must be taken into account, especially when specific signs of preeclampsia cannot be detected.
3. Case Report
A 27-year-old Caucasian woman (82 kg), primipara at the thirty-eighth week of her pregnancy, was admitted to our emergency rescue unit at the labor already commenced. Her medical history was negative, with no history of hypertension, except for an episode of childhood febrile seizures at the age of 17 months. Following the maternal request and after obtaining the informed consent, labor analgesia was carried out following the CSEA (Combined Spinal Epidural Anaesthesia) technique using the spindle water technique to search for the space. During the positioning, inadvertent dura mater puncture occurred. In accordance with our procedures, it has been decided to insert anyway the epidural catheter into the spinal space for the duration of 48 hours to alleviate the symptoms of PPDH (Post Puncture Dural Headache). The treatment of pain during the labor continued with adequate doses injected into the spinal space: 2.5 mg Chirocaine (0.75%). During the procedure, the blood pressure remained stable and the patient showed no signs of cortical irritation. After five hours, upon indication of the gynecologist, a caesarean section was performed due to the diagnosis of interruption in the dilation phase; hyperbaric bupivacaine (15mg) and morphine (70 γ) were administered in the intrarachidea cavity. The birth had no complications and, after a period of observation in the Recovery Room, the patient was transferred to the ward, she was painless with 117/85 mmHg blood pressure, FC 74b/m’, FR12a/m’, regular diuresis and Bromage score 0. It was requested not to remove the catheter for 48 hours and an antibiotic therapy with ampicillin 2gr. And analgesic therapy with Diclofenac 75 mg. and Paracetamol 1gr were started.
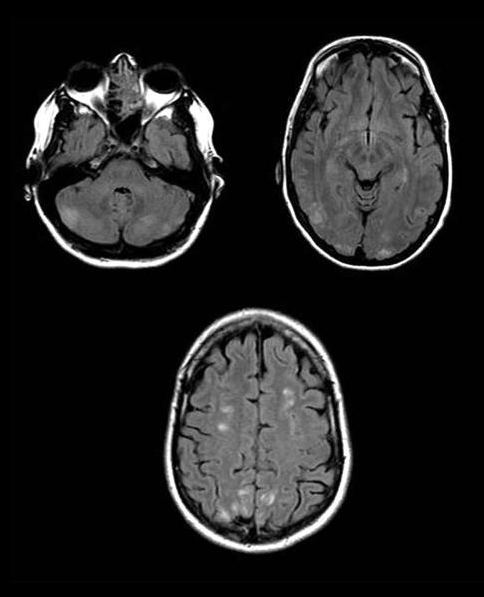
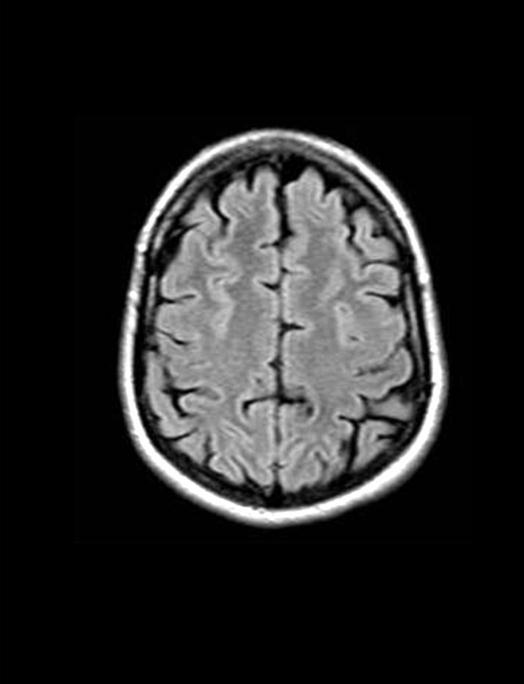
At the 48th hr, the patient developed a mild headache with no sign of nape contracture, which is typically exacerbated in an upright position with the occipital and frontal location accompanied by general malaise. The conditions remained stable up to 62nd hr after the birth; during the night the patient presented an episode of generalized seizure with loss of consciousness of a short duration which was treated and solved with midazolam (1mg) and propofol (50 mg). An episode of seizure disorder recurred after two hours, which was treated and solved in the same way, followed by another episode after a short time period; given the persistence of seizures, it was decided to perform a CT scan; the CT scan without contrast did not highlight significant findings, but the 48-hour reassessment is suggested; for that reason, the patient was admitted to the ICU. During the hospitalization occasional increases in blood pressure with maximum peaks equal to 140/90 mmHg, which are of ambiguous interpretation, occurred in conjunction with the laboratory investigations, which show liver enzyme abnormalities (GOT 80, GPT 100).The therapy administered was Gardenale 100mg, Magnesium Sulfate and Methyldopa, considering the clinical picture as a consequence of post-partum gestosis. The consulted Neurologist asked for a MRI scan to be performed, which showed significant PRES pathognomonic findings (figure.1) The patient is therefore moved to the acute cerebrovascular diseases to continue the treatment; after eight days, during which the patient had stable pressure values and the haematochemical tests were again within the standard values, the patient is reassessed with a new RMI scan, which shows a total remission of the aforementioned locus (figure.2)
4. Conclusion
The complication of the accidental puncture of the dura mater, the resultant observation and its treatment allow us to make a differential diagnosis highlighting a PRES clinical picture rarely detected during the pregnancy; otherwise, the pathology would be classified and treated as eclampsia post partum. In the future, we deem to investigate repeated convulsive events within peri-partum with specific diagnostic assessments (RM) since they may represent a PRES that, if it is not accurately treated, it can progress resulting in permanent and/or fatal neurologic consequences.
References
- Hinchey et al: A reversible posterior leukoencephalopathy Syndrome. N ENGL J MED 1996;
- K.M.Kuczkowski:Post-duralpuncture headache in the obstetric patient: An old problem. New Solutions minerva Anestesiol 2004;70:823-30;
- H. Doherty et al: Post dural puncture headache and Posterior Reversible Encephalopathy Syndrome: a misdiagnosis or co-presentation? International Journal of Obstetric Anesthesia 2014