Information
Journal Policies
Effects of HIV Infection and its Association with Male Infertility
Keerthana.S1, Ramakrishnan .V2*
2.Genetics Lab, Faculty of Allied Health Sciences, Chettinad Academy of Research and Education, Kelambakkam-603103, Tamil Nadu, India.
Copyright : © 2018 . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
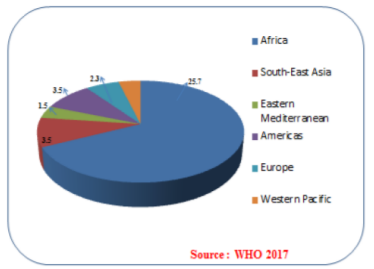
HIV endures to be a major worldwide public health issue has claimed over 35 million people living with HIV positive so far by the World Health Organization. In 2017, 940 000 people died because of HIV-related causes globally. There is no cure for HIV till now, but antiviral therapies have been carried out to reduce the viral transmission. HIV infection is classified under sexually transmitted diseases that colonize and replicate in the male and female reproductive tract and they are mainly transmitted through sexual intercourse. The sexually transmitted diseases have known to cause complications in female fertility, but the association with male infertility remains in debate. This review highlights the HIV infection that alters the semen parameters in Male reproductive system which may be one of the factors that causing Male infertility.
HIV virus, Male infertility, sexually transmitted infections, Semenial cells,AIDS
1. Introduction
Infertility is a defined as the problem that is seen in both male and female populations equally (Figure 1). It is a disease of the reproductive system which leads to the failure in achieving the clinical pregnancy after one year of regular unprotected sexual practices. Infertility occurs to a single cause because of one partner, or it could result from a combination of both the partners. This usually affects 15–20% of couples in which 50% accounts for the malefactor that was considered too because of this problem (WHO). The main symptom of infertility is an inability to reproduce an infertile man experience a hormonal problem like changes in hair growth or sexual problems[1]. The term "Male infertility" does not make up a defined clinical syndrome but rather the collection of different conditions exhibiting a variety of etiologies and varying diagnosis. Normally male fertility relies on the production and transports of sperm which is the highly complex process[2,3]. Sexually transmitted infections (STIs) cause problems in pregnancy and are associated with infertility complications in females, but the association with male fertility is still controversial. Many studies have been recently reported that sexually transmitted infections remain one of the major factors that cause male infertility. In STIs, the HIV virus attributes infections in the Male Genital Tract, where the semen remains the main vector in the transmission and the further infection leads to replication of viral load that affects the semen and sperm parameters which may cause Male infertility.
The microorganism is the primary source for Sexually transmitted diseases (STDs) that colonize the female and male genital tracts; during their early stage of infections they often show mild symptoms. STDs not only affect health it also causes many social and economic problems worldwide [2,3]. In spite of the advanced development of antibiotics and vaccines and the existence of disease prevention and control programs, these pathogens remain as the major cause for the acute and chronic disease. In 1993 the World Health Organization (WHO) reported the role of genital tract infections in human infertility (WHO, 1993). They have stated that most male genital tract infections are inducing infertility and previous studies related to male infertility have also reported that 15–20% of infertile subjects are affected by semen infection [4]. The semen has been associated with poor sperm quality, [5] decreases in sperm concentration and mortality on detecting by pathological, clinical tests it shows various STD-causing microorganisms [6,7]. The changes in other semen parameters relevant to fertility, including sperm velocity, morphology, and viability, and a seminal volume, pH, viscosity and biochemical composition have also been associated with STD-related infections.
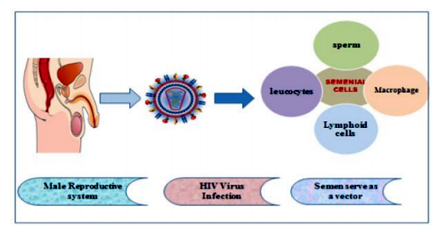
Semen, the male reproductive organ which consists of spermatozoa in suspension is considered to be an important vector for the spreading of viral diseases. Several viruses have also been detected in cell-free semen and in seminal cells, macrophages, and lymphocytes . Various types of viruses can infect the male reproductive tract tissues and semen, and the significance of these viral infections was important in terms of organ integrity, they involved in the progression of diseases and that would eventually change the reproductive and endocrine system's functions (Figure 2). Seminal leukocytes used as an indicator of male genital tract infection, but they were completely lacking because of the high load of infectious agents present. These viral infections seen in germ cells not only result in changing the testicular function, but also involved in the transmission of virus-induced mutations to the succeeding generations[8,9].
The two types of HIV 1 and HIV 2 are retrovirus which is closely related but differ in their pathogenicity, natural history and susceptibility to therapy. HIV 1, when compared to HIV-2, is more easily transmitted, and consequently is responsible for the vast majority of HIV infections globally. During sexual intercourse, blood-to-blood contact and perinatal transmission from mother to the child are the typical routes of HIV-1 transmission. It was found that semen shortly after primary infections. The infectious virus consists of three major modes of entry in semen, which is: free virions, spermatozoa-associated virions and infected leukocytes [11,12]. In leukocyte cell types such as primarily lymphocytes, monocytes and macrophages, and leukocytes were detected with HIV-1 provirus DNA and it was considered to be the main seminal source of HIV 1 infection. The possibility of viral replication rises within the seminal tract when there is a presence of virus in semen [13]. The mechanisms by which the HIV-1 viral population in the semen arise includes the direct import of virus, oligoclonal amplification within the seminal tract or compartmentalization [13,14]. There are seven types of cytokines and chemokine's (IL-1b, IL 4, IL 6, IL 7, IL 8, GM CSF and MCP 1)ratio in the semen blood were significantly increased in HIV-infected men compared with uninfected men, this shows that both innate and adaptive immune responses were influenced by the seminal environment[15,16].
At present, over 40 million people are infected with the human immunodeficiency virus type-1 (HIV-1). Most HIV-1-infected men and women are of reproductive age. The reproductive efficacy in HIV/AIDS can impact Male infertility. An HIV-1 infected man possesses certain sperm parameters that reflect fertility is significantly impaired. Semen parameters are within the normal range in asymptomatic HIV-positive men [17], while normal sperm morphology and motility are reduced with the progression of the disease [18]. Semen parameters associate positively with CD4 account [19], which suggests that patients with the complete stretch of AIDS are less fertile than recovering HIV-1 infected males. The Measurements include the semen volume, sperm motility, concentration and morphology that are adversely affected[19,20]. Semen parameters correlate positively with a CD4 count [19]that suggests that patients with a stretch of complete AIDS are less fertile than recovering HIV-1 infected males. The low sperm concentration was associated with a high percentage of sperm with abnormal morphologies and DNA damage in HIV- positive men, suggesting impairment of spermatogenesis [21,22]. Furthermore orchitis, hypogonadism, and leukospermia which could account for oligospermia and teratozoospermia arise during HIV-1 infection. When these alterations and dysfunction occurs in the Male reproductive system, this would eventually lead to cause male infertility. HIV can be suppressed by ART and certain anti-viral therapies that could reduce the infertility problem in the male community.
2. Conclusion
In the current scenario, it is important to emphasize the risk of the HIV virus that tends to be one of the factors which cause male infertility. This review summarizes current knowledge relating to the effects of HIV virus infection considered to have a potential negative effect on male reproductive function and the dangerous infections can be transmitted to partners and newborns moreover the infections seen in semen which alters the sperm parameters will induces male infertility through multiple pathophysiology mechanisms.
References
- Esteves, Sandro C., and Peter Chan. "A systematic review of recent clinical practice guidelines and best practice statements for the evaluation of the infertile male." International urology and nephrology 47.9 (2015): 1441-1456.
- Eisenberg, Michael L., et al. "Frequency of the male infertility evaluation: data from the national survey of family growth." The Journal of urology 189.3 (2013): 1030-1034.
- Jungwirth, Andreas, et al. "European Association of Urology guidelines on Male Infertility: the 2012 update." European urology 62.2 (2012): 324-332.
- Weidner, W., W. Krause, and M. Ludwig. "Relevance of male accessory gland infection for subsequent fertility with special focus on prostatitis." Human reproduction update 5.5 (1999): 421-432.
- Al-Daghistani, Hala I., et al. "Evaluation of serum testosterone, progesterone, seminal antisperm antibody, and fructose levels among Jordanian males with a history of infertility." Biochemistry research international 2010 (2010).
- Lee, Joong Shik, et al. "Concordance of Ureaplasma urealyticum and Mycoplasma hominis in infertile couples: impact on semen parameters." Urology 81.6 (2013): 1219-1224.
- Pekler, Vyacheslav A., et al. "Use of versant™ TMA and bDNA 3.0 assays to detect and quantify hepatitis C virus in semen." Journal of clinical laboratory analysis 17.6 (2003): 264-270.
- Dejucq, Nathalie, and Bernard Jégou. "Viruses in the mammalian male genital tract and their effects on the reproductive system." Microbiology and molecular biology reviews 65.2 (2001): 208-231.
- Kalichman, Seth C., Giorgio Di Berto, and Lisa Eaton. "Human immunodeficiency virus viral load in blood plasma and semen: review and implications of empirical findings." Sexually transmitted diseases 35.1 (2008): 55-60.
- Englert, Yvon, et al. "Medically assisted reproduction in the presence of chronic viral diseases." Human reproduction update 10.2 (2004): 149-162.
- Shattock, Robin J., and John P. Moore. "Inhibiting sexual transmission of HIV-1 infection." Nature Reviews Microbiology1.1 (2003): 25.
- Lederman, Michael M., Robin E. Offord, and Oliver Hartley. "Microbicides and other topical strategies to prevent vaginal transmission of HIV." Nature Reviews Immunology 6.5 (2006): 371.
- Anderson, Jeffrey A., et al. "HIV-1 populations in semen arise through multiple mechanisms. " PLoS pathogens 6.8 (2010): e1001053.
- Berlier, Willy, et al. "Amount of seminal IL-1β positively correlates to HIV-1 load in the semen of infected patients." Journal of Clinical Virology 36.3 (2006): 204-207.
- Dejucq, Nathalie, and Bernard Jégou. "Viruses in the mammalian male genital tract and their effects on the reproductive system." Microbiology and molecular biology reviews 65.2 (2001): 208-231.
- Cardona-Maya, Walter, et al. "In vitro human immunodeficiency virus and sperm cell interaction mediated by the mannose receptor." Journal of reproductive immunology 92.1-2 (2011): 1-7.
- van Leeuwen, Elisabeth, et al. "Semen quality remains stable during 96 weeks of untreated human immunodeficiency virus-1 infection. " Fertility and sterility 90.3 (2008): 63 6-641.
- Dondero, Franco, et al. "Semen analysis in HTV seropositive men and in subjects at high risk for HTV infection." Human reproduction 11.4 (1996): 765-768.
- Vandermaelen, Aline, and Yvon Englert. "Human immunodeficiency virus serodiscordant couples on highly active antiretroviral therapies with undetectable viral load: conception by unprotected sexual intercourse or by assisted reproduction techniques?." Human reproduction 25.2 (2009):374-379.
- Dulioust, E., et al. "Semen alterations in HIV-1 infected men." Human Reproduction 17.8 (2002): 2112-2118.
- Leruez-Ville, Marianne, et al. "Decrease in HIV-1 seminal shedding in men receiving highly active antiretroviral therapy: an 18 month longitudinal study (ANRS EP012). " Aids 16.3 (2002): 486-488.
- Gringhuis, Sonja I., et al. "C-type lectin DC-SIGN modulates Toll-like receptor signaling via Raf-1 kinase-dependent acetylation of transcription factor NF-κB." Immunity 26.5 (2007): 605-616.