Information
Journal Policies
Seizures in Human Immunodeficiency Virus (HIV) Patients: What is the Etiology?
Paddy Ssentongo MD MPH1*, Anna Ssentongo MPH2
2.Department of Public Health Sciences, Penn State College of Medicine, Hershey, PA, USA.
Copyright : © 2018 . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
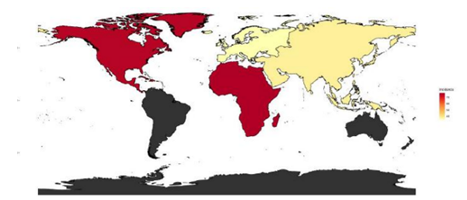
The prevalence and incidence of seizures and epilepsy is substantially higher in HIV patients compared to the general population and is associated with higher mortality rates. Although the prevalence of epilepsy in the general population is between 0.4% and 1.0%,[1] and the incidence rate is 0.05%,[2] the prevalence of seizures or epilepsy in the HIV population ranges between 3% -12%[3,4] See Figure1.
Over 2/3 of seizures in HIV patients are caused by metabolic disturbances,[5] CNS lymphoma or opportunistic infections of the central nervous system (CNS) such as toxoplasmosis, cryptococcal meningitis, tuberculous meningitis and progressive multifocal leukoencephalopathy[6-13]. In the remaining 1/3 of patients, seizures are not associated with any identifiable focal brain lesions but it has been suggested that HIV infection alone could be the sole cause these seizures[4]. In line with this hypothesis, the vast majority of seizures observed in HIV patients are generalized in nature. Therefore, it has been suggested that HIV-infected brain may have diffuse cortical irritability or an impaired mechanism of seizure termination[4].
The association between seizures and HIV is more pronounced in those with an advanced stage of HIV also known as acquired immunodeficiency syndrome (AIDS) and in those with low CD4 T-cell counts. AIDS is characterized by opportunistic infections such as disseminated Mycobacterium aviumcomplex, cytomegalovirus, Cryptococcal infections and toxoplasmosis,[14] all which are known to induce seizures. Furthermore, HIV viral load is at a higher concentration in patients with advanced stages of the disease, and HIV often leads to neuronal loss from discrete areas of the neocortex and subcortical regions[15]. In a study by Gelbard and colleagues, children with HIV-1 displayed neurons with apoptotic cells in the basal ganglia and cerebral cortex[16]. The principal pathway for HIV entry into the CNS is through infected monocytes (macrophages and microglia). Therefore, neuronal injury caused by HIV is predominantly indirect through the release of macrophages, microglial and astrocyte toxins, although direct injury by the virus is also possible[17]. These toxins over stimulate neurons, resulting in the formation of free radicals and excitotoxicity, which potentially lead to seizure generation and propagation. This information has led to the push for early initiation of highly active antiretroviral therapy (HAART) to reduce the viral load and increase functional CD4 T-cell counts. However, HAART use comes with the cost of the possibility of inducing seizures. The interactions between HAART and antiepileptic drugs are frequent as many members of the 2 classes of medications are metabolized by the cytochrome P450 system[18]. Carbamazepine, phenytoin, and phenobarbital, which are routinely used to control seizures in HIV populations, are metabolized by the cytochrome P450 system. There is risk of reduced antiretroviral levels and antiepileptic drug toxicity.
HIV/AIDS is a chronic systematic disease that induces focal and generalized CNS lesions that prime the brain to seizure initiation and propagation. Early initiation of HAART and vigilant use of electroencephalogram to detect non-clinical seizures are potentially effective strategies to prevent the high incidence of seizures in the HIV population. Furthermore, HIV individuals that are diagnosed with seizures should scrupulously be investigated for opportunistic infections. In addition to treatment of causative lesions or organisms, long-term use of antiepileptic drugs with frequent follow-up by both seizure and infectious disease specialist s key in the effective management of these patients.
Mimicking other CNS infection animal models such as murine models of cerebral malaria,[19,20] future efforts should be devoted to the development of animal models of HIV induced seizures to study mechanisms, of neuronal and glial pathology, signaling pathways, and to provide a platform for effective seizure prevention and control.
References
- Holden EW, Thanh Nguyen H, Grossman E, Robinson S, Nelson LS, Gunter MJ, Von Worley A, Thurman DJ. Estimating prevalence, incidence, and disease‐related mortality for patients with epilepsy in managed care organizations. Epilepsia 2005;46: 311-319.
- Kotsopoulos IAW, Van Merode T, Kessels FGH, De Krom MCTFM, Knottnerus JA. Systematic Review and Meta-analysis of Incidence Studies of Epilepsy and Unprovoked Seizures. Epilepsia 2002;43: 1402-1409.
- Pascual-Sedano B, Iranzo A, Martí-Fàbregas J, et al. Prospective study of new-onset seizures in patients with human immunodeficiency virus infection: Etiologic and clinical aspects. Archives of Neurology 1999;56: 609-612.
- Wong MC, Suite NA, Labar DR. Seizures in human immunodeficiency virus infection. Archives of Neurology 1990;47: 640-642.
- Van Paesschen W, Bodian C, Maker H. Metabolic Abnormalities and New-Onset Seizures in Human Immunodeficiency Virus-Seropositive Patients. Epilepsia 1995;36: 146-150.
- Chadha DS, Handa A, Sharma SK, Varadarajulu P, Singh AP. Seizures in patients with human immunodeficiency virus infection. The Journal of the Association of Physicians of India 2000;48: 573-576.
- Dore GJ, Law MG, Brew BJ. Prospective Analysis of Seizures Occurring in Human Immunodeficiency Virus Type-1 Infection. Journal of Neuro-AIDS 1997;1: 59-69.
- Bearden D, Steenhoff AP, Dlugos DJ, Kolson D, Mehta P, Kessler S, Lowenthal E, Monokwane B, Anabwani G, Bisson GP. Early antiretroviral therapy is protective against epilepsy in children with human immunodeficiency virus infection in botswana. Journal of acquired immune deficiency syndromes (1999) 2015;69: 193-199.
- Kellinghaus C, Engbring C, Kovac S, Möddel G, Boesebeck F, Fischera M, Anneken K, Klönne K, Reichelt D, Evers S, Husstedt IW. Frequency of seizures and epilepsy in neurological HIV-infected patients. Seizure 2008;17: 27-33.
- Bartolomei F, Pellegrino P, Dhiver C, Quilichini R, Gastaut JA, Gastaut JL. [Epilepsy seizures in HIV infection. 52 cases]. Presse medicale (Paris, France: 1983) 1991;20: 2135-2138.
- Kim HK, Chin BS, Shin H-S. Clinical Features of Seizures in Patients with Human Immunodeficiency Virus Infection. J Korean Med Sci 2015;30: 694-699.
- Pesola GR, Westfal RE. New-onset Generalized Seizures in Patients with AIDS Presenting to an Emergency Department. Academic Emergency Medicine 1998;5: 905-911.
- Holtzman DM, Kaku DA, So YT. New-onset seizures associated with human immunodeficiency virus infection: causation and clinical features in 100 cases. The American Journal of Medicine 1989;87: 173-177.
- Chang KH, Kim JM. Characteristics of HIV infection/AIDS in Korea. The Korean journal of internal medicine 2001;16: 1.
- Ellis R, Langford D, Masliah E. HIV and antiretroviral therapy in the brain: neuronal injury and repair. Nature Reviews Neuroscience 2007;8: 33.
- Gelbard H, James H, Sharer L, Perry S, Saito Y, Kazee A, Blumberg S, Epstein L. Apoptotic neurons in brains from paediatric patients with HIV‐I encephalitis and progressive encephalopathy. Neuropathology and applied neurobiology 1995;21: 208-217.
- Kaul M, Garden GA, Lipton SA. Pathways to neuronal injury and apoptosis in HIV-associated dementia. Nature 2001;410: 988.
- Okulicz JF, Grandits GA, French JA, George JM, Simpson DM, Birbeck GL, Ganesan A, Weintrob AC, Crum-Cianflone N, Lalani T. Virologic outcomes of HAART with concurrent use of cytochrome P450 enzyme-inducing antiepileptics: a retrospective case control study. AIDS research and therapy 2011;8: 18.
- Ssentongo P, Robuccio AE, Thuku G, Sim DG, Nabi A, Bahari F, Shanmugasundaram B, Billard MW, Geronimo A, Short KW, Drew PJ, Baccon J, Weinstein SL, Gilliam FG, Stoute JA, Chinchilli VM, Read AF, Gluckman BJ, Schiff SJ. A Murine Model to Study Epilepsy and SUDEP Induced by Malaria Infection. Sci Rep 2017;7: 43652.
- Bahari F, Ssentongo P, Schiff SJ, Gluckman BJ. A Brain–Heart Biomarker for Epileptogenesis. The Journal of Neuroscience 2018;38: 8473.