Information
Journal Policies
Socio-Cultural Factors Influencing Adherence to Antiretroviral Therapy among People Living with HIV/AIDS in Obafemi Awolowo University Teaching Hospitals, Ile-Ife, Nigeria
O. A Okunola1*, C.O Muoghalu2, A.I Irinoye3
2.Senior lecturer, Obafemi Awolowo Univesity, Department of Sociology and anthropology, Nigeria
3.Medical doctor, Obafemi Awolowo University Health Center, Ile-Ife, Nigeria
Copyright : © 2018 . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
The objectives are to investigate the influence of socio-cultural factors on adherence to treatment regimen and assess the prevalence of adherence to antiretroviral therapy (ART) among People living with HIV/AIDS (PLWHA) in Obafemi Awolowo University Teaching Hospitals, Ile-Ife, Nigeria.
A cross-sectional study design where both qualitative and quantitative research methods were adopted. Participants were HIV diagnosed patients attending clinic at the Hospitals Complex in Ile-Ife between the ages of 18 to 60 years. Three healthcare delivery personnel working in the clinic were interviewed. Using Fischer’s formula 336 patients living with HIV were selected for the study. Participants had been on antiretroviral drugs for more than six months prior to the study. Two focus group discussion sessions comprising of 10 male and 10 female living with HIV and currently on ART were conducted. These groups were purposively selected based on their being on ART for more than one year. In-depth interviews were conducted among three purposively selected healthcare givers (an experienced nurse, a doctor and a pharmacist) working in this clinic. Data were collected using a structured questionnaire, an interview guide and tape-recorder. Quantitative data were analyzed with descriptive and inferential statistics. Content analysis was used to analyze responses from IDI and FGD.
The study revealed high the level of adherence to ART was 89.0%. A strong relationship exists between family supports and the degree of adherence to ART. Nutrition, polygamy, and religion were highlighted as socio-cultural factors influencing adherence to ART. Age, level of education, occupation, ethnicity and whom they live with were reported to facilitate adherence to ART.
It was concluded that to achieve optimal outcome in the management of HIV various social and cultural contexts should be taken into consideration. This study was able to ascertain the influence of these various factors influencing adherence to ART.
ART, PLWHA, HIV/AIDS, Adherence,AIDS
1. Introduction
The scourge of Human Immunodeficiency Virus /Acquired Immunodeficiency Diseases (HIV/AIDS) with the development of antiretroviral drugs in its management has gone a long way to make it a chronic manageable disease. However, strict adherence is required to achieve therapeutic success in HIV management. Sub-Saharan Africa remains most heavily affected by Human Immunodeficiency virus (HIV) accounting for 65% of new infections globally, and 70% of People living with HIV/AIDS (PLWHA) (UNAIDS, 2017).
At an estimated 191 million, Nigeria is the most populated country in Africa (Population Reference Bureau) and with an estimated 3.2million PLWHA; has the second highest HIV burden globally after South Africa (UNAIDS,2017). Only 30% of PLWH in Nigeria had access to antiretroviral therapy (ART) (UNAIDS, 2017).An estimate of about 36.7 million people are living with HIV worldwide and AIDS-related death in 2016 was about 1.0 million. About 5000 new HIV infections daily in 2016 of which about 64% are in sub-Saharan Africa. In West-Africa about 6.1 million adults and children are living with HIV while death-related to HIV in this region was about 310,000 (UNAIDS, 2017).
The HIV prevalence in Nigeria is 3.4% in 2016 among people who inject drugs, 14.4% among sex workers and 23% among gay-men and other men who have sex with men (UNAIDS, 2017).
There is therefore the need for concerted efforts toward tackling this menace. The development and widespread use of antiretroviral therapy (ART) as the treatment of choice in HIV has improved significantly the health conditions of HIV positive individuals who could have untimely death. The ART however, has transformed the perception of HIV/AIDS from a fatal incurable disease to a manageable chronic illness (Deeks, Lewin, & Havlir, 2013). The treatment causes improvement in immunologic status and reduction in the viral load (Erb, Battegay, Zimmerli, Rickenbach, & Egger, 2000)which consequently reduces the incidence of hospitalization and mortality (Paterson, Swindells, & Mohr, 2000).
However, incomplete medication adherence is the most important factor in treatment failure and the development of resistance. Adherence is the term used to describe the patient’s behaviour of taking drugs correctly in the right dose, with the right frequency and at the right time. Antiretroviral treatment success depends on sustainable high rates of adherence to medication regimen of ART (Mills, Nachega, Buchan, & Orbinski, 2015). On the other hand, ART regimens are habitually complicated with variable dosage schedules, dietary requirements and adverse effects (Ferguson et al., 2002). Treatment success can be precarious with missing of few doses of antiretroviral medication which leads to drug resistant strains of HIV (Bangsberg et al., 2000). An adherent patient is defined as one who takes 95% of the prescribed doses on time and in the correct way, either with or without food. Adherence is a major predictor of the survival of individuals living with HIV/AIDS (Mills et al., 2015) and poor adherence to treatment remains a major obstacle in the fight against HIV/AIDS worldwide. Low or incomplete medication adherence has been associated with detectable viral load (> 500 viral RNA copies/ ml of plasma) (Rathbun, Id, Farmer, Stephens, & Loci, 2005) with the development of cross resistance to other antiretroviral of the same class (Tchetgen, Kaplan, & Friedland, 2001). Although, more potent antiretroviral regimens can allow for effective viral suppression at moderate levels of adherence (Knafl, Bova, Fennie, Malley, Dieckhaus, & Williams, 2008), none or partial adherence can lead to the development of drug-resistant strains of the virus. Cross-resistance however can potentially interfere with future therapeutic regimens for HIV- infected patients undergoing treatment and for those who subsequently become infected with resistant strains of HIV (Peltzer, Preez, Ramlagan, & Anderson, 2010).
Several studies on ART adherence (Nwauche et al., 2006; Chesney, 2000; Mukhtar-yola, Adeleke, Gwarzo, & Ladan, 2009; Oku, Owoaje, Ige, & Oyo-ita, 2013) had largely focused on the extent of adherence, knowledge and attitude, little attention was paid to associated socio-cultural factors that could pre-suppose adherence. The existence of various studies on the barriers to drug adherence among PLWHA notwithstanding; identifying the social and cultural factors influencing non-adherence to drug among PLWHA as stringent compliance to medication remains a very strong determinant of patients’ management outcome have not been given adequate attention. Several researchers have tried to look at those factors ranging from socio-economic issues, environmental factors, and patient-doctor’s interaction among PLWHA affecting their adherence, but not much attention have been paid to the influence of social and cultural factors simultaneously on this issue. This is the gap that this research intends to fill. As such adherence level of ART and socio-cultural factors will be addressed.
2. Objectives
The general objective of this study is to examine the various social and cultural factors hindering adherence to antiretroviral drugs of PLWHA in Obafemi Awolowo University Teaching Hospitals Complex (OAUTHC), Ile-Ife. The specific objectives are to:
1. Assess the prevalence of adherence to antiretroviral therapy among PLWHA in Obafemi Awolowo University Teaching Hospitals Complex (OAUTHC), Ile-Ife and
2. Investigate the influence of socio- cultural factors on adherence to treatment regimen in Obafemi Awolowo University Teaching Hospitals Complex (OAUTHC), Ile-Ife
3. Theoretical Framework
The other theoretical framework this study intends using is the Information Motivation and Behavioural Skills Model. The Information motivation, behaviour skills models will be reviewed to discuss adherence to antiretroviral treatment. According to (Fisher, Fisher, Amico, & Harman, 2006), Information-Motivation– Behavioural Skills-Model of adherence assumes that adherence related information, motivation and behavioural skills are critical determinants of adherence to antiretroviral treatment.
The model states that adherence–related information, motivation work through adherence-related behavioural skills to affect adherence to antiretroviral treatment. The implication of this model translates therefore to the extent that HIV patients are well informed, motivated to take action and possess the required behavioural skills to act effectively. Substantial health benefit of the treatment. Conversely, poor or non-adherence will occur and health benefit lost when HIV positive patients are poorly informed, motivated to take action and lack the required behavioural skills to act effectively, they will be more likely to adhere to medication regimens over time and in turn derive/experience. This model is of very significant value as a wide range of health related behaviours is linked to the profound influence of three key elements of information, motivation and behavioural skills (Fisher et al., 2006).
4. Methodology
The study is on socio-cultural factors influencing adherence to antiretroviral therapy among PLWHA in Obafemi Awolowo University Teaching Hospitals Complex in Ile-Ife. It was conducted in the Institute of Human Virology of Nigeria which is situated inside the premises of the teaching hospital in Ile-Ife. The study was conducted among the clients currently receiving ART there. This institution has catchment of patients from Ondo, Osun, and Ekiti states. The choice of the study location is as a result of the center been a referral center and at the same time the only place where ART is being carried out according to the national guideline on management of HIV AIDS patients in Ile-Ife and its environs. This center is selected as patients diagnosed of HIV from various neighboring communities are referred to this center for management hence having a wide distribution of clients from various zones.
Obafemi Awolowo University Teaching Hospitals Complex is a tertiary health Institution located in Ile-Ife with catchment of patients from Ondo, Osun and Ekiti states. The Obafemi Awolowo University Teaching Hospitals Complex is one of first generation of Teaching Hospitals established by the Federal Government to provide qualitative health care delivery to its people. The philosophy focuses on an integrated healthcare delivery system approach with emphasis on comprehensive healthcare service based on a pyramidal structure comprising primary care at the base, and secondary and tertiary services at hospital settings, designed to secure improvement in the physical, mental and socio-economic wellbeing of Nigerians through preventive, promotive, diagnostic, restorative and rehabilitative services. The philosophy allows for a unique experiment in health care delivery and health professional training in Nigeria. Primary healthcare is provided to the community in its three health centers-two urban and one rural in its catchments areas at Ife, Ilesa and Imesi –Ile respectively. Secondary and tertiary level cares are provided at its three major hospital facilities, in Wesley Guild Hospital Unit Ilesa, Ife State Hospital unit Ile -Ife and Dental Hospital located at Obafemi Awolowo University, Ile-Ife. By its recognition and establishment of Primary Health Care as an integral part of the country’s health care as close as possible to the people. While the Teaching Hospitals Complex, as a dynamic institution, had undergone various changes in its government, administration, management, physical resources and services load during its 25 years of existence, its founding philosophy to concept of provision of comprehensive health care based on integrated, primary, secondary and tertiary health care delivery has remained constant.
By virtue of its location and the scarcity of health care facilities in neighboring areas, the catchment area of the Obafemi Awolowo University Teaching Hospitals Complex is extremely large, including the whole of Osun Ekiti and Ondo State and some parts of Oyo, Kwara, Kogi, Lagos and Edo state. While the primary base is the Ife/Ijesa Senatorial District, the institution provides tertiary, secondary and primary health care services to the area mentioned above.
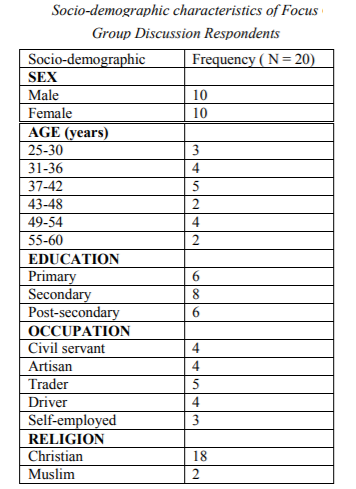
The study design was cross-sectional using both qualitative and quantitative methods of data collection. Semi-structured questionnaire was used to collect information for the objective which was to assess the prevalence and to determine the level of adherence to antiretroviral therapy (ART). Also the qualitative method was employed in order to gain the understanding of the respondents on the social and cultural factors influencing their adherence to ART. Thiswas done by conducting two focus group discussions (FGD) comprised of ten respondents, the first FGD comprised of 5males and 5 females while the second FGD comprised same. The FGD was conducted on two separate days of the clinic. The respondents were simple randomly selected by the nurses chosen every 10th client that registered for the clinic. This was done on two separate days of two weeks and the respondents were duely informed of the study. Also verbal consents were obtained before embarking on the FGD in which all the respondents were favourably disposed to voluntarily. Interview guide was used to conduct the FGD as the first session group lasted for 95 minutes and the second session group was done within 75 minutes. Study participants were clients who have been confirmed to be HIV positive and currently on treatment at the clinic for more than six months prior to the conduct of the study. The FGD was done on two separate days after the consultation hours as the respondents have been selected during clinic hours and then organised for the discussion sessions.
Adherence was determined based on assessment of six sets of questions on patients taking their medication without missing any drug within the last one week and non-adherence was based upon inconsistency or default in taking the drugs within the last one week.
The study populations were 3007 patients (male and female) between the ages of 18 and 60 years who have been receiving ARV drugs for over six months before the commencement of this study. Pregnant women, children and any other patients with other morbidities were not included in the study.
Sampling size was determined using the formula
Hence the sample size calculated is 336. As such 336 copies of questionnaire were administered on respondents. Also three in-depth interviews were conducted with a nurse, a doctor, and a pharmacist.
The sample for the study comprised of male and female clients who have been on ART for more than six months and between the ages of 18 to 60 years. One out of every tenth patients was systematically selected as they presented on each clinic days and were recruited until the desired sample size was achieved. These constituted the patients that were administered questionnaires. Patients aged between18 and 60 years on HAART for more than 6 months were eligible for inclusion.
The research instruments for this study were comprised of structured questionnaire. Each questionnaire comprised five sections namely, Sections A, B, C, D and E. Section A contained socio-demographic variables. This section was designed to provide information on respondent’s socio-demographic variables such as age, sex, marital status among others. Section B contained questions on HIV status and knowledge. Section C contained questions on client’s perception of ART. Section D contained questions on support network and various socio-cultural factors affecting ART while section assessed adherence to ART. Also interview guide was used to collect with seven sets of questions to assess various socio-cultural factors which are occupation, age, religion, norms and values, beliefs and shared practices affecting adherence to ART. Focus group discussion guide was also used to collect information from the respondents. Section A collected information on demographic variables, section was used to assess individual factors affecting ART and section C collected information on socio-cultural variables. The questionnaires were administered to the respondents at the clinic waiting room before they are called into the consulting room on their clinic days in the hospital while the interview and focus discussion groups were conducted in the consulting room after the end of the clinic for the day.
Several visits to the clinic and interaction with health workers and PLWHA indicated that there were about 3,000 PLWHA. Staff and patients were favourably disposed to participating in the study. Data were collected at the clinic by the researcher and a research assistant. Before the commencement of the study, the purpose of the study was explained to the respondents, assuring them of the confidentiality of their responses and identities. They were also assured that they would not come to any harm as a result of participating in the study. Also their consent was sought verbally and obtained prior to participation. Also, Ethical permission for the study was obtained from the Ethics and Research committee of OAUTHC, Ile-Ife with protocol number ERC/2015/08/29 to be conducted between 01/09/2015 to 31/09/2015.
Structured questionnaire was administered to the respondents. Interviews were conducted with the aid of an interview guide and included probes for further questioning, covering questions on how ART fitted into their daily routines and what the key barriers (social, personal and cultural factors) to adherence to ART were. Also two focus group discussion sessions were conducted with the aid of the focus group discussion guide. The interviews were conducted and audio-taped by the researcher and two research assistants that were trained postgraduate students in the department of sociology. Data were collected between May and September 2015
5. Data Analysis
The analysis of quantitative data was done in three stages. Firstly, the information obtained from the field was edited; the copies of questionnaire were thoroughly checked to correct all inconsistencies in responses by the respondents. This was done in form of field editing, that is, checking for mistakes and omissions in recording of information while on the field. Secondly, data analysis was preceded by data-coding and data-entry and analysed using Statistical package for social sciences version 20. Data were analysed using descriptive statistics and inferential statistics. The descriptive data were presented in the form of frequency distribution and percentages for inferential statistics, cross-tabulation of some variables and hypotheses, chi-square and regression analysis were employed to test the strength of relationship among the variables. The level of significance was set at p < 0.05. Information elicited through qualitative data was analysed using content analysis. The data were analysed in themes as each objective formed a theme. The audio responses were transcribedand verbatim quotations were utilized to describe the responses from the qualitative method.
6. Ethical Consideration
Before the commencement of the study, the purpose of the study was explained to the respondents, assuring them of the confidentiality of their responses and identities. They were also assured that they would not come to any harm as a result of participating in the study. Also their consent was sought verbally and obtained prior to participation. Also, Ethical permission for the study was obtained from the Ethics and Research committee of OAUTHC, Ile-Ife with protocol number ERC/2015/08/29 to be conducted between 01/09/2015 to 31/09/2015.
7. Results
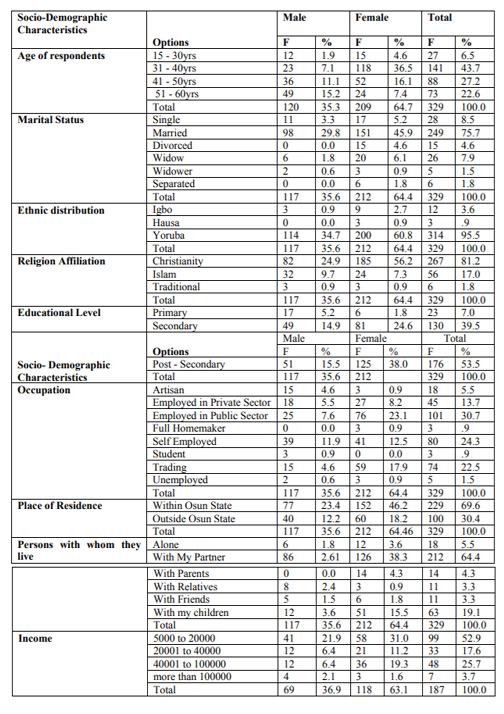
Firstly, univariate analyses presented the socio-demographic characteristics of the respondents using frequency distribution and percentages. The variables presented are sex, age, marital status, ethnic affiliation, religion, level of education, occupation, average monthly income, place of residence and people whom they are residing with. In all, three hundred and thirty-six (336) copies of questionnaire were administered in the clinic but three hundred and twenty-nine (329) were retrieved for analysis as the remaining questionnaires were not valid for analysis. The response rate is about 98%.
Table 1 presents the distribution of the socio-demographic characteristics of the respondents such as sex, age, marital status, ethnic affiliation, religion, level of education, occupation, average monthly income, place of residence and people whom they are residing with. This gives a comprehensive picture of the respondents for this study. Considering the sex distribution of the respondents from table 1, it was observed that female respondents constitute a larger percentage (64.4%) than the male (35.6%). On the basis of age, almost half (50.2%) of the respondents fall within the reproductive age of 30 to 40years, while 27.2% fall within 41 to 50 years and 22.6% are of more than 50 years. Data on marital status showed that 75.7% are married while 8.5% are single with 1.8% being separated. From the table it could be observed that 95.5% are of the Yoruba ethnicity, this is probably due to the location of the health facility which is domiciled in the southwestern part of the country where the Yoruba ethnic dominate. Only 0.9% are of the Hausa tribe and 3.6% belong to the Igbo ethnic distribution. As for the religious affiliation, majority (81.2%) were Christians and 17.0% were Muslims while only 1.8% identified with the traditional religion. It can also be seen that religion permeates all aspects of human life and experience since every respondent indicated being attached to one religious faith or another.
As for the educational level, the result revealed that 53.5% of them had post-secondary qualification level while 39.5% attained secondary education and 7.0% had primary level of education. As regards the type of occupation, those employed in the public sector were 30.7% and self-employed respondents were 24.3%. Also employed in the private sector were 13.7% and only 1.5% accounted for the unemployed cadre. The study revealed that 69.6% of the respondents receiving treatment in this facility
were residing within the state (Osun) while 30.4% of them were living outside the state. It was gathered that 5.5% of the PLWHA are living alone and 94.5% are residing with their partner, relative, children, parents and friends, this could be attributed to a very strong family support been rendered to them. Lastly from the table, the average monthly income distribution showed that 52.5% earned between five thousand to twenty thousand naira, 17.6% earned between twenty thousand to forty thousand naira while only 3.7% earned above hundred thousand naira.
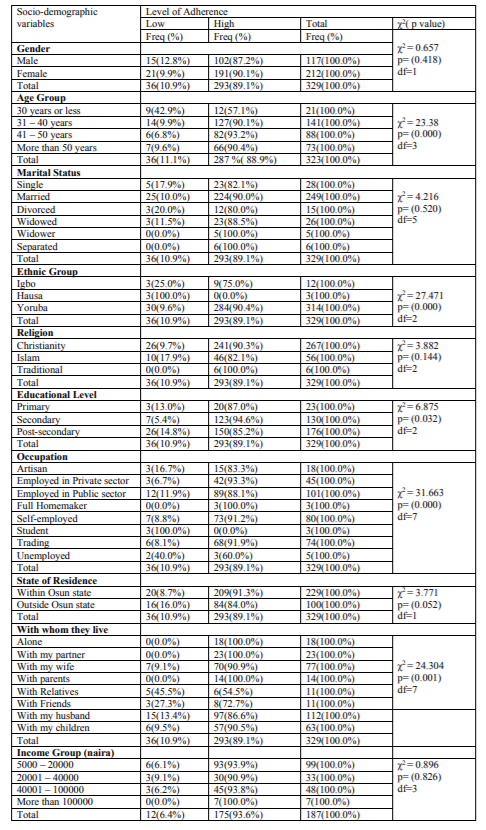
Table 2 presents the relationship between level of adherence to ART and socio-demographic variables.
It can be seen from the table that a significant relationship exists between adherence and respondents’ age. (χ2= 23.38, p < 0.05). Also the data showed that the older the respondents the higher their level of adherence to ART. Majority (90.1%) of the respondents in the 31 to 40 years age range were found to possess high level (90.1%) of adherence to ART than other groups (e.g. 57% for ages less than 30years). At high level of adherence, more (93.2%) of the older respondents (41 to 50yrs of age) feature than younger ones (57.1% among ages less than 30 years). However, at low level of adherence more of the younger respondents (less than 30 years) featured very prominently (42.9%) compared with the other age categories (e.g. 9.9% among 31 to 40 years’ age group and 6.8% for those in the 41 to 50yrs age bracket). This difference could be attributable to the reproductive and active adolescents that falls within this age bracket and are most vulnerable to HIV. Also it could be due to good awareness level among the age group.
Also, the data indicate that the level of adherence is significantly related to the ethnic group of the respondents (χ2= 27.471, p < 0.05). Yoruba demonstrated high level of adherence (90.4%), while the Igbo constitute 75 percent and none of those at high level of adherence from the Hausa ethnic group. All the Hausa in the study were found at the low level of adherence. This may be due to ethnic distribution because the Yoruba ethnicity dominates the study population and study area.
However, the respondents’ religion is insignificantly related to their level of adherence to ART (χ2= 3.882, p > 0.05). The traditional religion practitioners featured less prominently (0%) compared with other religious groups. At a low level of adherence, adherents of the Islam feature more prominently (17.9%) than the Christian (9.7%). In the overall Christianity (90.3%) religion exhibits a high level of adherence. Reason for this is not far-fetched as this religion is the most practiced in the study area.
When the relationship between educational level and adherence to ART was explored, a significant relationship was found to exist (χ2=6.875, p < 0.05). Adherence increases with the level of education. At a high level of adherence response 20 respondents attained primary education while 123 respondents were of secondary school educational attainments and
150 participants achieved post-secondary level of education. From the responses, it can be deduced that the knowledge and awareness about HIV in educational institutions impact on the level of adherence.
Further, a significant relationship exists between adherence with ART and occupation (χ2= 31.663, p < 0.05). Those who were employed in the private sector featured most (93.3%) in the category of those who possess high level of adherence and are closely followed by self-employed (91.2%). Public sector workers and artisans featured most prominently among those with low level of adherence with ART.
Finally, adherence with ART is also significantly related to whom the respondents live with. Among the respondents with high level of adherence group, those who live alone and those that lived with their partners featured most prominently (100.0%) closely followed by those who live with their children (90.5%). Those who live with relative featured very prominently among those with low level of adherence as well as those who live with their friends too possessed low level of adherence to ART. This is most likely to be as a result of support or encouragement from family support that gives rise to high adherence to ART.
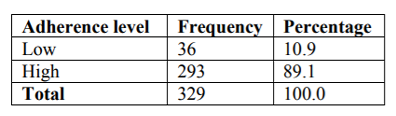
Table 3 below presents the distribution of the respondent’s level of adherence to ART, itwas indicated that 89.0% of the PLWHA have overall high adherence level to their ART. To measure the respondent’s level of adherence as presented in section E of the questionnaire, the questions were scored such that a ‘yes’ response was allocated 1 and a ‘no’ response was scored 0, negative items were transposed and then the scores were cumulated to constitute a measure of adherence to ART. The scores were categorized in such a way that any score of 3 or less were regarded as ‘very low’, any score greater than 3 and up to 4 were regarded as ‘low’, any score greater than 4 and up to 5 were regarded as ‘high’ and any score greater than 5 and up to 6 were regarded as ‘very high’. When asked during the focus group discussions on how many of their doses did they miss in the last one week, a 28 year female PLWHA revealed: not at all, I use it every night, while another 60 year female PLWHA said: I don’t miss at all.
However only 10.9% have relatively low adherence level. Among them was a 46 year female PLWHA who explained that: I missed it, twice and same with a 41 year female PLWHA: I‘ve not missed, I only take it few minutes after the scheduled time.
In determining the level of adherence to ART among PLWHA, from the study majority, 89.0% showed overall high adherence level while only few 10.9% were not well adhered to ART
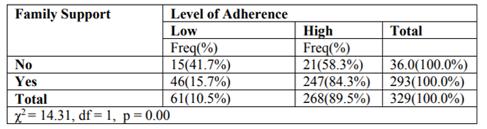
Table 4 below shows the relationship between family support and level of adherence to ART along with its significance. It revealed that among respondents with no family support, little above half of them have high level of adherence to ART, while about 58.3% percent and 41.7 percent of them have high and level of adherence respectively. Among respondents with high family support, expectedly, 84.3 percent have high level of adherence to ART with very minute proportion having low level of adherence to ART.
The Pearson’s chi-square value was 22.14. The probability associated with the chi-square statistic of 14.31 was .000 indicating a strong association between family support and level of adherence to ART. Among people with low level of adherence, 41.7% had no family support while 15.7% had family support.
This study engaged in interview with the health workers in the clinic on ‘what do you see as social barriers to antiretroviral therapy treatment among your clients’? A 43-year female nurse explained: Some people do have problem with nutrition and if they are not feeding well it’s not good enough for them maybe because of the economic situation of the country, if there is anything we can do to support them nutritionally adherence will be better. The perception from a doctor response to the same question was that good nutrition is needed by the individual for most drugs to be efficacious to the body. This is evident in his response: we found out in the clinic that some of them are not well fed as they require adequate and good food has the drugs they take requires them to be eating very well for the good efficacy of the ARV they are taking. The present state of economy in the country may be mostly contributing to the food insecurity which in turn affects patients on ART to have low adherence. However, as the drugs are free to these clients, response from a 42-year female during the FGD revealed that she feels comfortable with the free treatment but has difficult with food: my problem is with food as it is a bit difficult to get food for me, and I thank God the drugs are free.
The culture of having more than one wife is a common phenomenon in the Ile-Ife community hence it was highlighted by the interviewees as one of the barriers to ART among PLWHA.
Non-adherence to ART arising from couples in polygamous settings in order to avoid stigmatization was noted by 43 year female nurse when asked ‘What do you See as Social Barriers to Antiretroviral Therapy Treatment among your Clients’?.: THERE ARE SOME WOMEN IN THE POLYGAMOUS SETTINGS THAT WON’T disclose to their husband because they don’t want the other wives to know and because of that when the man is around they will not use their medication so that the man will not ask why are you using these drugs, what is it for, so with that they are not really adherent and at the end of the day problem will come.In fact, there’s a particular woman that refused to disclose to the husband, the first husband died, she married another one and this one discovered after so many years of living together and he just picked the medication and took it away and the drugs are not within her reach, somebody like that cannot use it because the drugs are out of her reach, somebody like that cannot come back to collect, so eventually decided to stay away.
However, in other climes polygyny enhances adherent to ART as partners disclose to each other and they take their medications together as explained by the doctor in the clinic: Polygyny is a very good example, but some of them it can be husband that’s first diagnose or later the wife and they do disclose to each other later so as to take the drugs together.
Most of the respondents interviewed have a strong belief in their faith but despite that, they drew a very sharp line between taking their medication and their religion. Some of them also said that observing fast is no more possible for them so as to adhere very well to the drugs.
A 42-year-old female PLWHA during the FGD, when asked ‘what is your religion belief about taken ART medication? ‘revealed: it doesn’t stop me from taking my drugs and after all I didn’t tell my pastor that I am having HIV and my faith cure it through my drugs because it’s God that can help make the drugs to work o. Furthermore, a strong faith in the ART with high adherence regardless of religion was identified from a 52 year female PLWHA, here is her excerpt: as a Baptists we know that HIV is real and we have medical personnel that come to the church for awareness on regular basis. And once you know how to go about it, it cannot kill you so we do sensitized people on it. We belief there is no other thing apart from the medication we are using and with god all things are possible, but one should not tempt god, once you take your medicine and u keep praying to god, it will work together, but that doesn’t mean one should leave its medication without taking it. The two work together but finally concentrate on your medicine. Another view was that been religious does not stop her from taking her medication as the two acts are different, this was reported by a 39 year male PLWHA: it doesn’t antagonize taken this ARV at all and one cannot use religion to cure diseases as HIV is a disease and its only drug that can be used to manage it.
However, few respondents were of the strong belief in their religion more than the ARV drugs. As explained by a male 50 year PLWHA: we are just praying that God will put a full stop to it, the final cure/medicine that we cure it, before I was told malaria was like this and later they find cure to it and I belief because, I didn’t die when the illness hold me to the extent that I cannot drink water, immediately I eat I will vomit it then.
Also excerpt from a 43-year nurse informed on the influence of the faith leaders in their adherence: in this environment we are so religious and little things like this we will run to our faith leaders so when they go there, maybe the faith leader is not well informed, some we tell them if they can pray and fast their HIV will go but whereas there are some faith leaders that will interact too here and we encourage them here and support them there are some of them that only disclose their status to their pastors and their pastors have been supportive. We counsel faith leaders here we even invite them and have meetings with them.
8. Discussion Of Findings
The focus of this study was to contribute to the knowledge in the area of socio-cultural factors that influence adherence to antiretroviral therapy among PLWHA attending clinic at OAUTHC, Ile-Ife. It has been pointed out by researchers that for PLWHA to live a long healthy life there must be a very high level of adherence or compliant to the antiretroviral therapy. This is because these classes of drugs are the only form of management for HIV presently as there has been no cure for this ailment. The prevalence of adherence to ART in this study was 89.0%.
However, (Onyeonoro, Ebenebe, Ibeh, Nwamoh, Ukegbu & Emelumadu, 2013) revealed higher prevalence 97.8% which was more than what this study reported. This probably was attributable to a fairly good knowledge and perception of ART among the respondents. Contrary to (Erah & Arute, 2008), the prevalence was low 58.1% as the adherence was dependent on adverse drug effects and educational level of patients. Poor financial status, medication adverse effects, lack of confidentiality, occupational factors and stigmatization were the major reasons given for non-adherence. The higher prevalence in this present study was attributed to age, ethnicity, educational level, occupation and whom they are living with as affirmed by Edwards, 2006 Our findings from the study using qualitative method offer an understanding of social and cultural factors that may influence patients’ adherence to ART in OAUTHC, Ile-Ife. We believe our results may be valid for other similar settings that have the same socio-cultural background. Although socio-cultural factors vary in different climes. It was highlighted from this study that nutrition, religion and polygyny influence adherence to ART among the respondents.
Adequate intake of good food has been reported by PLWHA as one of social factors militating against adherence to ARV drugs among them. It revealed the impact of food security in the area of nutrition as a militating factor to ART adherence among PLWHA in OAUTHC, Ile-Ife. Thiswas corroborated in a study among HIV infected students conducted by Steenkamp, Goosen, Venter, & Beeforth, (2016) where food insecurity was identified as one of the factors contributing to non-adherence of ART. Also, Sanjobo, Lukwesa, Kaziya, Tepa, & Puta, (2016) reported lack of nutrition support as one of the barriers to ART adherence among patients on ARV in Zimbabwe. Provision of food or nutritional support during the clinics if made free like the antiretroviral drugs may increase adherence to ART among clients in this setting.
Besides the nutrition problem, religion was affirmed as one of the cultural factors that play a double-edged sword in adherence to ART because it both militates and promotes the adherence to ART depending on the context. Among the respondents who are of the Christian religion, adherence to ART was high possibly as a result of the information and awareness by the faith leaders which they hold in very high esteem. However, among the Islamic faithful, adherence to ART was low, this could be attributed to Islamic religion which emphasize on destiny while Christian focus more on faith healing. Tocco, (2017) affirmed that patients’ medication adherence was affected by the desire to fulfill religious fasting obligations and to avoid question from family and friends unaware of the HIV positive status. It was also revealed that despite been a traditionalist, none availability of ritual practices or atonement against HIV disease made them to adhere fully to ART as there is no alternative to the antiretroviral drugs.
Furthermore, polygyny identified as a cultural practice was noticed to influence ART adherence among the respondents. Arising from the practice is most likely a non-disclosure of status among partners which in turn militates against adherence. Where as in another partners, this practice enables them to adhere very well because the partners disclose to one another their status. In a similar vein, study among PLWHA in a teaching hospital in Kenya revealed ART adherence was significantly associated with marital status as monogamous married and polygamous married respondents were more likely to have optimal adherence as compared to widowed or widower, (Mugoh, Kabiru & Mwaniki, 2016).
Considering the influence of socio factors on the adherence to ART (Table 4), the study found a very high support from family members of PLWHA and their friends as a very strong indicator for adherence with 84.3.0% have a high support level from them. It shows a significant association between family support and adherence to ART (χ2 = 22.4, p< 0.05). To support the result from our study findings, (Wasti, Simkhada, Randall, Freeman & Van Teijlingen, 2012) affirmed that perceived health benefits, and family support were the most-reported facilitators to adherence on ART.
In table 2, a significant statistically relationship was reported between age, ethnicity, level of education, occupational level, whom they live with and adherence level among the respondents. The age group 31-40 years which are within the reproductive age group adhered strongly to ART. Education attainment and level of adherence to ART exhibited a significant statistical relationship (χ2= 26.04, p < 0.05). Adherence is inversely proportional to educational attainment. At the very high level of adherence response with secondary school educational attainments feature most prominently (45.4%) closely followed by those with post-secondary educational attainment (40.9%). Most of those with low adherence were post-secondary educational attainment. This probably informed them of their awareness and knowledge on their status hence, improved their level of adherence.(Oku et al., 2013)reported that medication adherence was found to be significantly associated with non-use of traditional herbal medicine which was supported by the finding from this study as not seeking alternative treatment contributed positively to adherence in this study.
The respondents’ religion is also significantly related to their level of adherence to ART (χ2= 16.76, p < 0.05). The traditional religion practitioners featured prominently (50%) compared with other religious groups. At the very low level of adherence, adherents of the Islam feature more prominently (12.5%) than the Christian (1.9%). This could be attributedto Islam religion which emphasizes on destiny while Christianity focus more on faith healing.
9. Conclusion
The study concluded that among PLWHA attending clinic in OAUTHC, Ile-Ife, various socio-cultural factors was identified to influence ART adherence. The social factors noted include – age, educational level, occupation, ethnicity and whom they live with- as these have improved their adherence to ART. The cultural factors revealed from the study were religion and polygyny while the social factor elicited using the qualitative methods from the respondents was inadequate nutrition. These three factors explained the non-adherence to ART in this setting.
Further research is needed to be conducted on a large scale study in the region to confirm generalizability.
Our findings can inform the design of intervention to promote adherence to ART using the socio-cultural perspectives highlighted from the study.
Acknowledgement
This research was supported by the Consortium for Advanced Research Training in Africa (CARTA). CARTA is jointly led by the African Population and Health Research Center and the University of the Witwatersrand and funded by the Carnegie Corporation of New York (Grant No--B 8606.R02), Sida (Grant No:54100029), the DELTAS Africa Initiative (Grant No: 107768/Z/15/Z). The DELTAS Africa Initiative is an independent funding scheme of the African Academy of Sciences (AAS)’s Alliance for Accelerating Excellence in Science in Africa (AESA) and supported by the New Partnership for Africa’s Development Planning and Coordinating Agency (NEPAD Agency) with funding from the Welcome Trust (UK) (Grant No: 107768/Z/15/Z) and the UK government, " The statements made and views expressed are solely the responsibility of the fellow.
References
- Bangsberg, D. R., Hecht, F. M., Charlebois, E. D., Zolopa, A. R., Holodniy, M., Sheiner, L., … Moss, A. (2000). Adherence to protease inhibitors , HIV-1 viral load , and development of drug resistance in an indigent population. AIDS, 14, 357–366.
- Chesney, M. A. (2000). Factors Affecting Adherence to Antiretroviral Therapy. Clinical Infectious Diseases, 30(2), 171–176.
- Deeks, S. G., Lewin, S. R., & Havlir, D. V. (2013). The end of AIDS: HIV infection as a chronic disease. The Lancet, 382(9903), 1525-1533.
- Edwards, L. V. (2006). Perceived social support and HIV/AIDS medication adherence among African American women. Qualitative health research, 16(5), 679-691.
- Erah, P. O., & Arute, J. E. (2008). Adherence of HIV / AIDS patients to antiretroviral therapy in a tertiary health facility in Benin City, 2(7), 145–152.
- Erb, P., Battegay, M., Zimmerli, W., Rickenbach, M., & Egger, M. (2000). Effect of Antiretroviral Therapy on Viral Load, CD4 Cell Count, and Progression to Acquired Immunodeficiency Syndrome in a Community Human Immunodeficiency Virus–Infected Cohort. Arch Intern Med., 160, 1134–1140.
- Ferguson, T. F. F., Tewart, K. E. S., Unkhouser, E. F., Olson, J. T., Estfall, A. O. W., & Aag, M. S. S. (2002). Patient-perceived barriers to antiretroviral adherence : associations with race. AIDS CARE, 14(5), 607–617. https://doi.org/10.1080/09540120210 00005434
- Fisher, J. D., Fisher, W. A., Amico, K. R., & Harman, J. J. (2006). An Information – Motivation – Behavioral Skills Model of Adherence to Antiretroviral Therapy. Health Psychology, 25(4), 462–473. https://doi.org/ 10.1037/ 0278-6133.25.4.462
- Joint United Nations Programme on HIV/AIDS (UNAIDS). (2017). Ending AIDS: progress towards the 90-90-90 targets. Global AIDS Update.
- Knafl, G. J., Bova, C. A., Fennie, K. P., O’Malley, J. P., Dieckhaus, K. D., & Williams, A. B. (2010). An analysis of electronically monitored adherence to antiretroviral medications. AIDS and behavior, 14(4), 755-768.
- Kumarasamy, N., Safren, S. A., Raminani, S. R., Pickard, R., James, R., Krishnan, A. S., ... & Mayer, K. H. (2005). Barriers and facilitators to antiretroviral medication adherence among patients with HIV in Chennai, India: a qualitative study. AIDS Patient Care & STDs, 19(8), 526-537.
- Mills, E. J., Nachega, J. B., Buchan, I., & Orbinski, J. (2015). Adherence to Antiretroviral Therapy in Sub-Saharan Africa and North America. JAMA, 296(6), 679–690.
- Mugoh, E. K. N., Kabiru, E. W., & Mwaniki, J. (2016). Patient factors influencing adherence to art treatment among HIV/AIDS patients in Embu teaching and referral hospital comprehensive care clinic.
- Mukhtar-yola, M., Adeleke, S., Gwarzo, D., & Ladan, Z. F. (2009). Preliminary investigation of adherence to antiretroviral therapy among children in Aminu Kano Teaching Hospital , Nigeria. African Journal of AIDS Research, 5(2), 141–144. https://doi.org/10.2989/16085 900609490374
- Nwauche, C. A., Erhabor, O., Ejele, O. A., & Akani, C. I. (2006). Adherence to antiretroviral therapy among HIV-infected subjects in a resource-limited setting in the Niger Delta of Nigeria. African Journal of Health Sciences, 13(3-4), 13-17.
- Oku, A. O., Owoaje, E. T., Ige, O. K., & Oyo-ita, A. (2013). Prevalence and determinants of adherence to HAART amongst PLHIV in a tertiary health facility in south-south Nigeria. BMC Infectious Diseases, 13(1), 1. https:// doi.org/10.1186/1471-2334-13-401
- Onyeonoro, U. U., Ebenebe, U. E., Ibeh, C. C., Nwamoh, U. N., Ukegbu, A. U., & Emelumadu, O. F. (2013). human immuno deficiency virus /acquired immuno deficiency syndrome in a tertiary health facility in South Eastern Nigeria, 1(2), 2–7. https://doi.org/ 10.4103/2321-9157.126631
- Palella, F., Delaney, K., & Moorman, A. (1998). Declining Morbidity and Mortality among Patients with Advanced Human Immunodeficiency Virus Infection. The New England Jiournal of Medicine, 339(6), 405– 412.
- Paterson, G., Swindells, S., & Mohr, J. (2000). Adherence to protease inhibitor therapy and outcome in patients with HIV infection. Ann Intern Med, 133, 21–30.
- Peltzer, K., Preez, N. F., Ramlagan, S., & Anderson, J. (2010). Antiretroviral treatment adherence among HIV patients in KwaZulu-Natal , South Africa. BMC Public Health, 10(111), 1–10.
- Rathbun, R. C., Id, B., Farmer, K. C., Stephens, J. R., & Loci, S. M. (2005). Impact of an Adherence Clinic on Behavioral Outcomes and Virologic Response in the Treatment of HIV Infection : A Prospective, Randomized , Controlled Pilot Study. Clinical Therapeutics, 27(2), 199–209.
- Ritzer, G. (Ed.). (2008). The Blackwell companion to major classical social theorists (Vol. 26). John Wiley & Sons.
- Sanjobo, N., Lukwesa, M., Kaziya, C., Tepa, C., & Puta, B. (2016). Evolution of HIV and AIDS Programmes in an African Institution of Higher Learning: The Case of the Copperbelt University in Zambia. The open AIDS journal, 10, 24.
- Steenkamp, L., Goosen, A., Venter, D., & Beeforth, M. (2016). Food insecurity among students living with HIV: Strengthening safety nets at the Nelson Mandela Metropolitan University, South Africa. SAHARA-J: Journal of Social Aspects of HIV/AIDS, 13(1), 106-112.
- Tchetgen, E., Kaplan, E. H., & Friedland, G. H. (2001). Public Health Consequences of Screening Patients for Adherence to Highly Active Antiretroviral Therapy. Journal of Acquired Immune Deficiency Syndromes, 26(2), 118–129.
- Tocco, J. U. (2017). The Islamification of antiretroviral therapy: Reconciling HIV treatment and religion in northern Nigeria. Social Science & Medicine, 190, 75-82.
- UNAIDS. (2010). UNAIDS: Report on the global. HIV/AIDS epidemic 2010. Geneva Switzerland
- Wasti, S. P., Simkhada, P., Randall, J., Freeman, J. V., & Van Teijlingen, E. (2012). Factors influencing adherence to antiretroviral treatment in Nepal: a mixed-methods study. PloS one, 7(5), e35547