Information
Journal Policies
Injury Risk among Family Members of Medically Identified Substance Abusers
Ted R. Miller¹, Nancy N. Carlson ², Diane Lestina, B.S.³
2.Assistant Professor, Graduate Counseling Program, University of the District of Columbia, Connecticut Avenue, NW,Building 44--Suite 200 Washington,USA.
3.College Station, Texas,USA.
Copyright : © 2016 Ted R M. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Objective: To estimate injury risk and medical payments of adult and child family members of substance abusers.
Design: Retrospective case-control study using 1987-89 medical claims data from Medstat Systems, Inc. Regressions compared injuries, injury hospitalizations, injury costs, and substance abuse incidence of 6,717 family members in employer-insured families where at least one adult was medically identified as an alcohol or drug abuser versus in a demographically-matched random sample of 37,488 control families.
Results: Forty percent of family members of substance abusers sustained an injury compared to 38% of controls (OR = 1.10, 95% CI = 1.02, 1.17). Children ages 15-19 in families with a drug abuser had the highest probability of hospitalized injury (4.3%, OR = 1.5, 95% CI = 1.03, 1.96) and stayed more than 3 times as long in the hospital as injured controls (13 days versus 6 days). Among children ages 0-19, the highest proportion of injury medical payments were in drug abusing families. Children in families with an adult substance abuser were more likely to be substance abusers (3.8% vs. 0.3%).
Conclusions: Family members of medically-identified substance abusers had modestly higher injury rates than members of families with no known abusers.
Keywords: spouse; child; alcohol; drugs; cost.
1.Introduction
Alcohol misuse and abuse clearly causes injury[1-3]. The injured include both drinkers and alcohol-negative people injured or killed in alcohol-attributable incidents [4-6]. Spouses and dependent children of adults with medically-identified alcohol abuse are at high risk. Children are endangered when transported by intoxicated adults, and alcohol misuse and abuse is associated with elevated risk and severity of child maltreatment [7, 8], intimate partner violence [9-12], and injury of family members [13-22] A further contributor to the elevated injury risk is that parental substance abuse (some of it attributable to genetics) raises the substance abuse risk of children [16, 23-27] and presumably the associated injury risk.
Unlike for alcohol abuse, the consequences of adult drug abuse for spouses and dependent children are little-studied. A few studies cited above looked at substance abuse rather than just alcohol abuse [16, 25]. Although drug abuse is implicated in family violence [8, 10, 12, 28, 29], its effects on other injury is largely unmeasured. Moreover, no studies differentiate risks from abusing both drugs and alcohol versus either class of substances alone.
We analyzed injury risks in families insured by any of 70 large U.S. corporations, including both hourly and salaried workers in retail and manufacturing. Drawing from a longitudinal data base of health care claims, we compared injury rates and injury medical payments of adult and child family members of medically identified substance abusers versus controls. The data accessible to us were old, so they primarily capture the risks that marijuana, cocaine, heroin, and amphetamine abuse impose on families. The physiological effects of drug abuse that caused those injuries should not change over time.
2.Methods
In the time period covered by this study, Medstat Systems, Inc. had a longitudinal database of deidentified healthcare claims for 1.5 million people with corporate health insurance, which now is part of the Truven Health Marketscan® data system. Medstat inpatient and outpatient records included diagnostic data, paid charges, age, sex, position in family, and state of residence, but no other demographics. The Medstat data contained up to 5 diagnosis codes from the Clinical Modification of the 9th Revision of the International Classification of Diseases (ICD-9-CM, 1991) per inpatient record and a single ICD-9-CM code per outpatient record.
The Medstat data lacked information on injury cause, which precluded examination of risk by specific causes such as motor vehicle crash or assault. No information was available on whether the injuries occurred on or off the job; but on-the-job injuries generally are paid by Workers’ Compensation (claims that were not in our data) so our study largely excludes occupational injuries. Our analysis excluded people older than age 65 because they had Medicare coverage, so Medstat claims data omitted much of their care. Thus our analysis essentially examines non-occupational injuries to the working population under age 65. Our study uses a case-control design. Its methods closely parallel the methods in Miller, Lestina, & Smith [30], which analyzed injury risk of substance abusers in the Medstat data.
The National Institute on Alcohol Abuse and Alcoholism (NIAAA) obtained complete 3-year family health care claims histories from Medstat for all families where any benefit-eligible adult family member had a definite or possible alcohol-related or drug-related primary or secondary diagnosis (listed in Appendix A) during 1987 to 1989. The alcohol abuse diagnoses were those used by the Alcohol Epidemiologic Data System, Division of Biometry and Epidemiology, NIAAA [31]. This group of substance abuse diagnoses consisted of the traditional chronic alcohol abuse indicators such as liver disease and cirrhosis; subacute indicators such as alcoholic psychoses and alcohol dependence syndrome; and acute toxic effects of ethanol poisoning. Drug-related abuse indicators included drug psychoses, drug dependence, and drug abuse. Some diagnosis codes can result from substance abuse or another cause. We excluded anyone with only these possible substance abuse codes such as unspecified disorder of liver; hepatorenal syndrome; hemorrhage of gastrointestinal tract, unspecified; or barbiturate overdose from abuse or error in therapeutic use.
For this study Medstat created a control group that demographically matched another family to each family with a substance abuser or possible abuser. The control families had to have at least one health care claim during 1987 to 1989, lack substance abuse diagnoses anywhere in their family records, and match by employee age (grouped in 5-year cohorts), employee sex, geographic location, employee relationship (employee vs. dependent), employee status (active vs. retired, COBRA, or other), and employee class (hourly vs. salaried). Two matched control families were selected randomly for each substance abusing family.
Fearful that including the possible abusers in the analysis would misclassify some nonabusers as cases, we dropped 12,027 possible abusers from the abuser group. However, we decided to retain their controls and account statistically for demographic differences between the treatment and control groups.
Family members of substance abusers were categorized into three groups: family members of alcohol and drug abusers, family members of alcohol-only abusers, and family members of drug-only abusers. Also included were children, ages 0-19, of adult substance abusers who were abusers themselves. These children were classified according to the type of adult abuser. For example, if a drug abusing child had an adult family member who abused alcohol, the child would be classified as a family member of an alcohol abuser.
Following Miller, Lestina & Smith [30], injury was defined as any claim with an ICD-9-CM diagnosis code of 800-994 or the following acute injuries covered elsewhere in the ICD-9-CM: amnestic syndrome (294.0); post concussion syndrome (310.2); traumatic cataract (366.2); respiratory poisoning (506, 507.1, 508.0); injury to teeth (521.2, 525.1); displacement of intervertebral disc (722.0 - 722.2); coma (780.0, with no secondary diagnoses--a common coding choice to maximize reimbursement for head injuries in that time period); and asphyxia (799.0).
The diagnosis codes 965.0, 965.1, 967-970, and 977.9 define drug-related poisoning and 980.0 defines ethyl alcohol poisoning. Typically, these diagnoses are considered injuries. Because they describe acute drug and alcohol abuse outcomes, however, we excluded them from the study definition of injury. On inpatient records, some people had primary diagnoses of substance abuse and secondary diagnoses of injury. It was unclear if these cases would have required admission absent the abuse. Therefore, except in sensitivity analysis, we excluded these admissions from the injury counts. Thus, our admitted injury counts are conservative.
We wanted to analyze episodes of care due to injury. However, this claims database records injury visits, so we developed an algorithm, described in detail elsewhere ([32]), to determine injury episodes rather than just any initial or follow-up injury visit. The algorithm is complex because when an injury occurs it can affect several body systems/organs and one person can be injured several times. Claims were separated into body region for purposes of counting injury episodes. An episode started with the first medical claim due to injury. Using linked inpatient and outpatient insurance claims data, by hospital admission status, we established a clear zone—a maximum visit-free period for the duration between injury treatment visits for each body region injured. If a claim date exceeded the clear zone from the previous injury visit, then a new episode was initiated.
We estimated relative risk (odds ratios) and confidence interval bounds for occurrence of medically treated injury for family members of people in each substance abuse group using logistic regression analysis with the following explanatory variables: sex, age group, employee class, geographic region, and age group and sex of the abuser. Statistical analyses were performed with the SAS statistical software, version 6. All regressions excluded cases where the only abuser in the family was an adolescent.
Medstat did not provide medical payments. We modeled them using published national average lifetime medical payments per victim by primary ICD-9-CM diagnosis and hospital admission status [33], inflated to 2015 dollars using the Consumer Price Index-Medical Care. Lifetime medical payments include payments for acute care, hospital readmission, rehabilitation, home health care, nursing home care, prescriptions, medical equipment, and insurance claims processing. Payments for hospitalized injuries were multiplied by the diagnosis-specific ratio of hospitalized length of stay for the Medstat case compared to the national average. The published payment data have been used to cost injuries in other studies [30, 34, 35]. We used log-linear regressions to analyze payment variations between groups controlling for the demographic variables.
3.Results
Of 8,588 families with at least one adult substance abuser; 69% had at least one alcohol abuser, 14% had at least one drug abuser, and 17% had at least one family member who abused both drugs and alcohol (not tabulated). Twenty-eight percent were families where the primary beneficiary was a salaried employee, 61% were hourly, and the rest were unknown. More than 40% lived in Illinois, Indiana, Michigan, Ohio, or Wisconsin.
The probability of a medically-treated injury claim in a 3-year period for family members of medically-identified adult substance abusers was modestly, but significantly higher than for family members in the control group (40% vs. 38%, as shown in Table 1). Of child family members ages 0-4, those in families with adult drug and alcohol abusers had the highest injury risk (31%, OR = 1.22, 95% CI = 1.01,1.44) compared to 26.2% for controls. For children ages 5-14, those in drug-only abusing families had the highest risk (49%, OR = 1.25, 95% CI = 1.08,1.42); children ages 15-19 were most at risk in alcohol-abusing families (52%, OR = 1.16, 95% CI = 1.07,1.25). Among adult family members, those living in families with a drug and alcohol abuser had the highest injury risk (38%, OR > 1.16, 95% CI = 1.05, 1.28).
Odds ratios adjust for sex, geographic region, hourly vs, salary employee, and age group and sex of the abuser.
Hospitalized injuries serve as a proxy for severity. We found little or no increased probability of hospitalized injury among family members except with children ages 15-19 in families that abuse drugs or alcohol (Table 2). Children ages 15-19 of drug abusers had the highest probability of hospitalized injury (OR = 1.50, 95% CI = 1.03,1.96 ) in a 3-year period, followed by those in families with an alcohol abuser (OR = 1.40, 95% CI = 1.15,1.65, not tabulated). Children ages 15-19 in families with drug abuse had two times the mean length of stay when compared to families with no abuse (Table 3). The mean length of stay for children ages 5-14 was three times as long in families of drug abusers (9.1 days) as controls, followed by children in families of alcohol and drug abusers (8.4 days). Hospital admissions at ages 0-4 were too infrequent to analyze.
We also examined the percentage of children with a substance abusing adult family member who were medically identified as abusers themselves. Overall, the percentage of identifiable abusing children was 3.8% in families with an adult abuser, compared to 0.3% in families without an adult abuser. In the 15-19 age group, 17.0 % of children in families where an adult identifiably abused drugs only were medically identified as abusing either drugs, alcohol or both themselves. In total, 8.3% of children of alcohol and drug abusers and 7.1% of children of alcohol-only abusers were identified as drug or alcohol abusers. We compared injury rates for abusing children and non-abusingchildren by type of family abuse. Although a slightly higher percentage of substance-abusing children had medically treated injuries, the difference was not statistically significant (OR = 1.05; 95% CI = 0.95, 1.15, not tabulated). More striking is the percentage of substance-abusing children with hospitalized injuries. Hospitalized injury rates for abusing children of substance abusers are 8.7% compared to 2.3% of non-abusing children of substance abusers (OR = 4.0; 95% CI = 3.66, 4.35).
Overall, 8% of the families had more than one substance abuser. In general, injury rates were similar in families with female abusers when compared to male abusers. The one exception was a higher injury rate for children 5-14 with an alcohol and drug abusing female (OR = 1.6, 95% CI = 1.26-1.95, not tabulated).
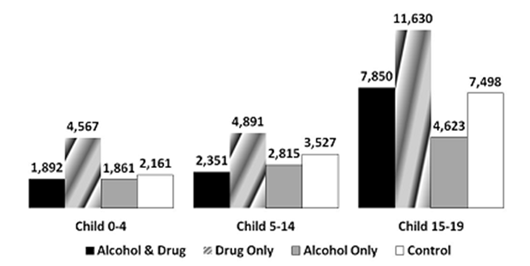
Figure 1 shows modeled mean lifetime medical payments due to injuries of family members during the 3-year period. In all three age groups, children in families with drug abusers had the highest lifetime medical payments ($4,567 (SE = 2,263), $4,891 (SE=1,224) and $11,630 (SE = 3,267)). Among adult family members, those living with an alcohol and drug abuser had the highest payments, ($8,697 (SE = 4,310), not shown).
4.Discussion
This study is the first to separately assess the injury risk to spouses and children of drug-only abusers and of drug and alcohol abusers. It also provides greater insight and a somewhat different interpretation than prior studies assessing the effect of alcohol abuse on family members of abusers.
We found that family members of medically identified substance abusers have slightly higher injury rates when compared to family members of a demographically-matched control group. While well below some injury risk estimates in the literature for alcohol abuse [13, 23], our estimates are consistent with the most recent estimates [16, 25].
Unlike other studies, we used medically-reported alcohol and drug conditions to identify abusers rather than self-identification in surveys. A potential explanation for the reduced intergroup differences we observed in younger households is that heavy drinking is endemic in the male population ages 20 34; however, that drinking seldom leads to a diagnosis being recorded in claims data. In a previous analysis of these data, twice as many alcohol abusers were identified from ages 35-49 as at ages 20-34 [30]. Because medical markers of chronic substance abuse have long latency periods, young abusers are less likely to be medically identified, leading to the misclassification of their family members as control group members. This is the age group with the largest number of young children. Thus, many family members in the control group could be family members of problem drinkers, meaning we overestimate injury risk among the controls relative to alcohol abusers.
We use a narrow definition of medically identifiable abuse so our cases are likely to be only those where there has been treatment or at least recognition of a medical problem related to abuse. Notably studies disagree about whether excess injury and health services utilization rates among dependents revert to the norm when alcoholic abusers receive treatment for their drinking problems [25, 36].
Reversion to the norm might dilute some of the effects of alcohol abuse on injury rates in our study.
By a small margin, injury incidence for child family members of substance abusers usually exceeded that of controls in all groups. However, the mean medical payments per injury of children of alcohol-only and alcohol and drug abusers were lower than for children in non-abusing families. This finding could imply that although more frequent, the severity of injuries sustained by children of substance- abusing families is lower than those in non-abusing families or that substance- abusing families more often seek injury treatment at emergency departments rather than physicians’ offices. The largest difference in costs and hospitalized injuries was to children 15-19 in drug-abusing families; 17% of children in this group are substance abusers themselves.
Studies differed about whether children of alcoholics were more likely to be hospitalized for injury but agreed they were more likely to be diagnosed with and hospitalized for substance abuse [16, 23-25]. Our study found no increase in hospitalized injury for children ages 0-4 or 5-14 in substance abusing families. We did find an increase for children 15-19 in families abusing drugs only or alcohol only. We also found that 7% to 17% of the children ages 15-19 of substance abusers were medically-identified abusers themselves. Furthermore, children of substance abusers who were abusers themselves had an increased risk of hospitalized injury. Since substance abuse raises a person’s injury risk, the elevated child injury risks we observed may be explained by the increased risk of children becoming abusers.
In our study, children had slightly higher injury rates in families with a female abuser than ones with only a male abuser. Bijur et al. [13] also found that maternal alcohol-related problems are strongly associated with serious child injuries, while the father's alcohol consumption and reported drinking appeared to be unrelated to child injury risk.
We counted all injuries in a 3-year period, regardless of when substance abuse was detected. Our objective was to examine the excess injury risk of abusers, including risk associated with their lifestyle, not just their abuse. Substance abuse is not a sudden-onset disease. Rather, it is an ongoing problem that typically matures before being identified in a clinical setting. A snapshot before and after identification seems most appropriate. Indeed, the largest validity threat may be post-identification. For some, identification leads to treatment that reduces substance abuse, changes lifestyles, and thus reduces injuries. Notably, since only 7% of the abusers were detected from secondary diagnoses on hospital records, the identification of substance abusers poses only a minor threat to study validity.
Our study also has several limitations related to the Medstat data. The 1987-1989 data are old. They lack enrollment information, which means we could not calculate family size or accurately classify two-parent families where one parent had no medical claims over three years. Inability to account for those claim-free people will cause an overestimate of injury rates. Although all subjects had at least one medical claim, they might not have been enrolled for the entire 3-year period, which would cause us to underestimate injury rates per year insured by a Medstat employer. It is unclear if substance abusers change employment at higher rates than non-abusers. If they do leave at a higher rate, the effect would be to underestimate the injury rates and subsequent injury risks for this group. Thus our estimates would be conservative as no data are available on injuries after termination.
Another limitation arises because the outpatient claims recorded only one diagnosis. Since substance abuse and injury diagnoses sometimes co-occur, outpatient claims will undercount both types of events (as only one can be recorded). As the methods section indicated, our hospitalized injury counts excluded some cases with only secondary injury diagnoses. We also did not define alcohol and drug poisonings as injuries. Thus our injury counts are conservative.
The Medstat data lack information on injury causation, which precludes examination of risk by specific causes such as motor vehicle, assault or self-inflicted injuries (e.g., suicide attempts). They also largely exclude occupational injuries.
As mentioned earlier, comparisons of substance abusers with an unavoidably impure control group might well obscure actual rate differences between abusers and controls. Our study is unique, however, in that it is able to use readily available claims data to examine the problem. It thus represents a novel cost-effective approach using already collected data.
Our findings suggest that substance abuse prevention and treatment services for children of medically-identified adult substance abusers often are needed. This is especially true when adults abuse drugs. The need for intervention by health professionals to help reduce injury rates in these families, however, is not much different than for other families. Nevertheless, the potential for reducing injury costs in family members is an often overlooked benefit of providing substance abuse treatment.
The bottom line is that much, if not all of the previously observed excess injury risk faced by children of substance abusers apparently results from substance abuse by those children. (Substance abuse, of course, raises injury risk). This finding underlines the need to screen offspring of known substance abusers for abuse problems. Further, it suggests the need to develop brief but effective preventive interventions for those children.
5.Acknowledgement
This work was supported by National Institute on Alcohol Abuse and Alcoholism (NIAAA) Grant No. AA09812-02.
References
- Borges G, Cherpitel CJ, Orozco R, Bond J, Ye Y, Macdonald S, et al. Acute alcohol use and the risk of non-fatal injury in sixteen countries. Addiction 2006;101(7):993-1002.
- Cherpitel CJ, Ye Y, Bond J, Borges G, Monteiro M, Chou P, et al. Alcohol Attributable Fraction for Injury Morbidity from the Dose‐Response Relationship of Acute Alcohol Consumption: Emergency Department Data from 18 Countries. Addiction 2015;110(11):1724-1732.
- Miller TR, Spicer R. Hospital-admitted injury attributable to alcohol. Alcohol Clin Exp Res 2012;36(1):104-112. doi: 10.1111/j.1530-0277.2011.01593.x.
- Cherpitel CJ, Ye Y, Bond J, Room R, Borges G. Attribution of alcohol to violence-related injury: self and other’s drinking in the event. J Stud Alcohol Drugs 2012;73(2):277-284.
- Miller TR, Lestina DC, Spicer RS. Highway crash costs in the United States by driver age, blood alcohol level, victim age, and restraint use. Accid Anal Prev 1998;30(2):137-150.
- Levy DT, Miller TR, Mallonee S, Spicer RS, Romano EO, Fisher DA, et al. Blood alcohol content (BAC)-negative victims in alcohol-involved injury incidents. Addiction 2002;97(7):909-914.
- Walsh C, MacMillan HL, Jamieson E. The relationship between parental substance abuse and child maltreatment: findings from the Ontario Health Supplement. Child Abuse Negl 2003;27(12):1409-1425.
- Magura S, Laudet AB. Parental substance abuse and child maltreatment: Review and implications for intervention. Child Youth Serv Rev 1996;18:193-220.
- Stith SM, Smith DB, Penn CE, Ward DB, Tritt D. Intimate partner physical abuse perpetration and victimization risk factors: A meta-analytic review. Aggress Violent Behav 2004;10(1):65−98.
- Foran HM, O'Leary KD. Alcohol and intimate partner violence: a meta-analytic review. Clin Psychol Rev 2008;28(7):1222-1234.
- Graham K, Bernards S, Wilsnack SC, Gmel G. Alcohol may not cause partner violence but it seems to make it worse: A cross national comparison of the relationship between alcohol and severity of partner violence. J Interpers Violence 2011;26(8):1503-1523.
- Kepple N. Does Parent Substance Use Always Engender Risk for Children? An examination of the relationships between substance use patterns, social support type, and child maltreatment behaviors. In. Los Angeles, CA: Dissertation, Ph.D. in Social Welfare, UCLA; 2015.
- Bijur PE, Kurzon M, Overpeck MD, Scheidt PC. Parental alcohol use, problem drinking, and children's injuries. JAMA 1992;267:3166-3171.
- Damashek A, Williams NA, Sher K, Peterson L. Relation of caregiver alcohol use to unintentional childhood injury. J Pediatr Psychol 2009;34(4):344-53.
- Ray GT, Mertens JR, Weisner C. The excess medical cost and health problems of family members of persons diagnosed with alcohol or drug problems. Medical Care 2007;45(2):116-22.
- Ray GT, Weisner C, Mertens JR. Family members of persons with alcohol or drug dependence: Health problems and medical cost compared to family members of persons with diabetes and asthma. Addiction 2009;104:203–214.
- Reading R, Jones A, Haynes R, Daras K, Emond A. Individual factors explain neighbourhood variations in accidents to children under 5 years of age. Soc Sci Med 2008;67(6):915-27.
- Journal of Community Health NursingRussell KM. Preschool children at risk for repeat injuries. J Community Health Nurs 1998;15(3):179-190.
- Orton E, Kendrick D, West J, Tata LJ. Independent risk factors for injury in pre-school children: three population-based nested case-control studies using routine primary care data. PLoS One 2012;7(4):e35193.
- Putnam S. Parental alcoholism as a risk factor in adolescents’ injury rates: An HMO study. In: American Medical Conference on Unintentional Injuries in Adolescents. Chicago, IL; 1987.
- Tyrrell EG, Orton E, Tata LJ, Kendrick D. Children at risk of medicinal and non-medicinal poisoning: A population-based case-control study in general practice. Br J Gen Pract 2012;62(605):e827-833.
- Baker R, Orton E, Tata LJ, Kendrick D. Risk factors for long-bone fractures in children up to 5 years of age: a nested case-control study. Arch Dis Child 2015;100(5):432-7.
- Woodside M, Coughey K, Cohen R. Medical costs of children of alcoholics--pay now or pay later. J Subst Abuse 1993;5:281-287.
- Lipscomb HJ, Dement JM, Li L. Health care utilization of families of carpenters with alcohol or substance abuse-related diagnoses. Am J Ind Med 2003;43(4):361-8.
- Ray GT, Mertens JR, Weisner C. Comparison of health care needs of child family members of adults with alcohol or drug dependence versus adults with asthma or diabetes. J Dev Behav Pediatr 2014;35(4):282-91.
- Walters GD. The heritability of alcohol abuse and dependence: a meta-analysis of behavior genetic research. Am J Drug Alcohol Abuse 2002;28(3):557-84.
- Agrawal A, Lynskey MT. Are there genetic influences on addiction: Evidence from family, adoption and twin studies. Addiction 2008;103(7):1069-1081.
- Miller TR, Levy DT, Cohen MA, Cox KL. The costs of alcohol and drug-involved crime. Prev Sci 2006;7(4):333-342.
- Walton-Moss BJ, Manganello J, Frye V, Campbell JC. Risk factors for intimate partner violence and associated injury among urban women. J Community Health. 2005;30(5):377-89.
- Miller TR, Lestina DC, Smith GS. Injury risk among medically identified alcohol and drug abusers. Alcohol Clin Exp Res 2001;25(1):54-59.
- Cases MF, Stinson FS, Dufour MC. Surveillance report #32: Trends in alcohol-related morbidity among short-stay community hospital discharges, United States, 1979-92. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism, Division of Biometry and Epidemiology; 1994.
- Lestina DC, Miller TR, Smith GS. Creating episodes of injury using medical claims. J Trauma 1998;45:323-328.
- Miller TR, Pindus NM, Douglass JB, Rossman SB. Nonfatal injury costs and consequences: A data book. Washington, DC: The Urban Institute Press; 1995.
- Miller TR, Spicer RS. How safe are our schools? Am J Public Health 1998;88(3):413-418.
- Miller TR, Cohen MA. Costs of gunshot and cut/stab wounds in the United States, with some Canadian comparisons. Accid Anal Prev 1997;29(3):329-341.
- Lennox RD, Scott-Lennox JA, Holder HD. Substance abuse and family illness: Evidence from health care utilization and cost-offset research. J Mental Health Admin 1992;19(1):83-95.