Information
Journal Policies
Single or Double Site Cannuation for Veno-Venous Ecmo in Severe Obese Patient?
Angela Lappa MDa, Marzia Cottini MDb⃰, Silvia Donfrancesco, MDa, Federico Ranocchi MD b, Giampaolo Luzi MD b, Andrea Montalto MD b, Carlo Contento CCPb, Agrò Bruno CCPb, Patrizia Pisani CCPb, Proietti Antonio CCPb, Vitalini Emiliano CCPb, De Marco Marina CCPb, Petraforte Laura CCPb, Iaiza Alessandra CCPb,Antonio Menichetti, MDa, Francesco Musumeci, MD, FECTSb
b.Department of Heart and Vessels, Cardiac Surgery Unit and Heart Transplantation Center , “S. Camillo-Forlanini” Hospital, Rome, Italy
Copyright : © 2016 Marzia C. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Veno - venous extracorporeal membrane oxygenation (VV-ECMO) is an extracorporeal respiratory support used as therapeutic option in patients affected by severe acute respiratory distress syndrome (ARDS), who are not responding to other medical or mechanical treatment. By providing supplementation of pulmonary gas exchange, VV-ECMO allows the lungs to rest and avoids the use of aggressive mechanical ventilation. Therefore, this support provides the basis for a possible recovery of the pulmonary parenchyma damaged by the underlying respiratory disease. Over the last two years, there has been a widespread increase in the use of the VV-ECMO due to the influenza A-H1N1 pandemic. The VV-ECMO approach could be with single or double site cannulation: the single one is performed to reduce the incidence of bleeding, infection and get better the medical and nursing management of the patient (prone position, mobilization, and so on) but this cannulation is a challenge for the mechanical support because of higher resistances, more shunts, much more modification of the flux with a little bit dislocation (for instance during transfer). We reported a case of the first experience of unsuccessful use of single cannulation with VV-ECMO, thus requiring a conversion to dual cannulation with a successful outcome.
Keywords: Acute respiratory distress syndrome (ARDS); ECMO (extracorporeal membrane oxygenation); hypoxia; lung pathology; lung infection.
Abbreviations: VV-ECMO-Veno-venous Extracorporeal Membrane Oxygenation, ARDS- Acute Respiratory Distress Syndrome, BMI-Body Mass Index, CT-Computed Tomography, ABG-Arterial blood gases, WBC-White Blood Count, CRP-C-Reactive Protein, TEE-Transesophageal Echocardiographic, APTT-Activated Partial Thromboplastin Time, SIMV-Synchronized,Intermittent Mandatory Ventilation, PS-Pressure Support, PEEP- Positive end-expiratory pressure, RR-Respiratory Rate
1.Introduction
A 49-year-old male affected by severe obesity (BMI 40.1 Kg/m2 ), sleep apnea syndrome and type II diabetes mellitus, developed severe ARDS by influenza A, which was not responsive to maximal ventilatory support and to cycles of prone positioning in a secondary hospital. After 48 hours, the patient was recovered to our Cardiovascular Intensive Care Unit to perform VV-ECMO treatment.
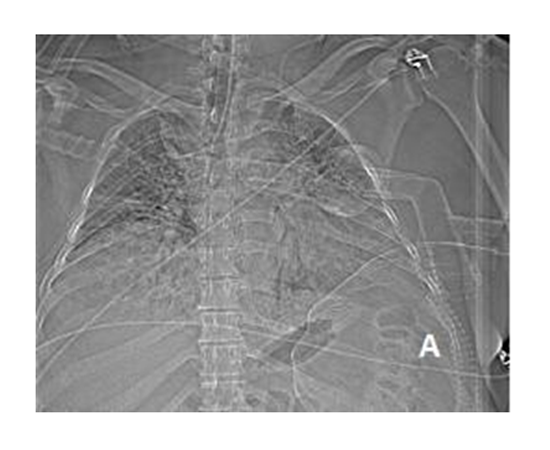
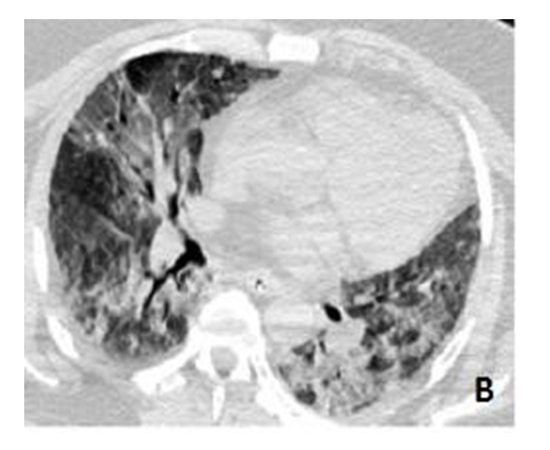
Upon admission, the chest Computed Tomography (CT) scan showed an extensive case of ARDS with pulmonary infiltrates affecting all lung fields (Figure 1). The Murray Score (1) was 3.5 and arterial blood gases (ABG) showed: pH 7.33, pO2 40 mmHg, pCO2 51 mmHg, HCO3 25 mmol/L, pO2/FiO2 ratio 172 and evidence of mild tissue hypoxia (Lactate 3.4, SVO2 74.7, Table 1). Laboratory values revealed white blood count (WBC) 4.420 x 109 /l,C-Reactive Protein (CRP) 8,45 mg/dl, the cultural samples were collected and both the tracheal aspirate and the nasal swab tested were positive to Influenza A (not type H1N1). The patient had no other sign of systemic failure (PA 165/50 mmHg, HR 95 beats/min, diuresis 70 ml/h).
VV-ECMO was set-up using single cannulation with an Avalon Elite Bicaval Dual Lumen Catheter 31Fr (Avalon laboratories, LLC 2610 E. Homestead Place Rancho Dominguez, CA 90220,USA) percutaneously positioned in the right internal jugular vein and connected to an ECMO circuit (Maquet® Cardiopulmonary AG Hechinger Strabe 38 72145 Hirrlingen, Germany). Using transesophageal echocardiographic (TEE), the cannula was placed and documented into the inferior vena cava with the outflow orifice pointed 280° towards the tricuspid valve ( Figure 3). The correct positioning of the cannula was also confirmed by a chest X-ray. The ECMO flow rate was 51.4 ml∙Kg-1 ∙min-1 (set up on Height 180 cm and weight 130 Kg), air flow 8 lt/min and FiO2 0.9. The perfusionists checked pressure drop and gas exchanges of the oxygenator every 12 hours. The Gases after VV-ECMO were get better (pH 7.41, PCO2 35.3, PO2 41.4, SVO2 73.3, Hb 11.8).
Synchronized intermittent mandatory ventilation (SIMV) was employed with the following setting: tidal volume 6ml/Kg, PS 22 cmH20, PEEP (Positive end-expiratory pressure) 12cmH2O, RR (respiratory rate) 10/min, FiO2 0.6.
Three unexpected episodes of decreased pump flow rate occurred 48 hours after VV-ECMO implantation. Each time, the arterial blood gas values worsened significantly, with the following mean values: pH 7.48, pCO2 31.4 mmHg, pO2 41.7 mmHg, even if the oxygenator performance appeared normal. A TEE was performed each time to control cannulae good setting but it showed a displacement of the cannulae, which required repositioning.
Considering the severity of the patient's clinical status, the estimated long recovery time of the lungs, and the unstable flow of blood due to frequent dislocation episodes of the Avalon cannulae, a double venous cannulation was set-up.
On the 5th day, a new Medtronic 21Fr (Minneapolis MN) cannulae was positioned in the right femoral vein. Under TEE guidance, the pre-existing Avalon Elite DLC was pulled back from the inferior vena cava until the right atrium to avoid recirculation.
With the conversion from single to dual cannulation, the venous blood was drawn from the inferior vena cava through the new femoral cannulae and oxygenated blood returned to the right atrium through the pre-existing Avalon Elite DLC (Figure 4).
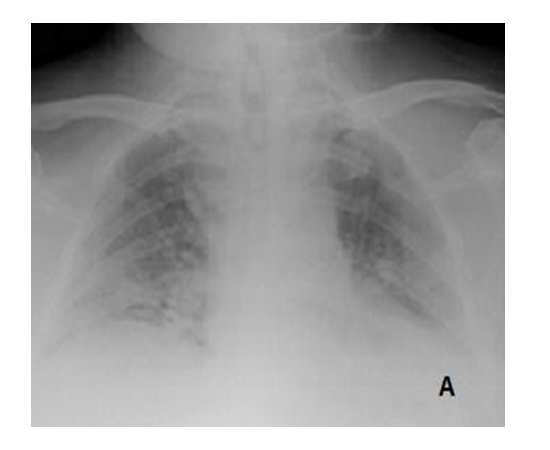
Two weeks after the dual cannulation of VV-ECMO, a chest X-ray revealed significant improvement (Figure5). Gradual weaning from ECMO support was started during the third week. The tracheostomy was not performed in order to decrease bleeding, infection and cruel maneuver in complex patient.
ECMO support lasted 21 days, at which time the patient's ABG evidenced satisfactory values: pH 7.41,pO2 135 mmHg,pCO2 34 mmHg with minimal ECMO support:FiO2 0.21,Air 0.5 lt/min and blood flow 2 L/min. The blood gas at outflow from the oxygenator was pH 7.37, pO2 36 mmHg, pCO238mmHg.The ventilator support was SIMV, RR9/min, PEEP 10cmH2O, PS 20cmH2O, and ECMO was removed.
The patient was extubated after 7 days and underwent non-invasive ventilation cycles, three times a day, until his complete mobilization. He was then transferred to a postoperative rehabilitation clinic in a good condition (Figure 6a and b).
2. Discussion
VV-ECMO is a valid support for severe and refractory respiratory failure as a bridge to lung transplant or pulmonary recovery. Historically, VV-ECMO has been performed with dual peripheral cannulation, usually inserted into jugular and femoral veins.
For many years VV-ECMO has been used in children through single cannulation in the right internal jugular vein. The catheter has two lumens: one lumen draws blood from both the inferior and the superior vena cava, while the oxygenated blood flows through the second lumen into the right atrium
In 2009, the U.S. Food and Drug Administration approved the Avalon Elite Bicaval Dual Lumen Catheter to perform VV-ECMO with single cannulation in adult patients. This cannulae is characterized by two lumens, separated by a flexible membrane that divides the oxygenated blood from venous drainage. The distal opening should be placed into the inferior vena cava, while the proximal tip should be in the right atrium facing the tricuspid valve. The correct positioning should be verified through fluoroscopy, transthoracic echocardiogram or TEE which is strong recommended (3, 4, 5).
Compared to dual cannulation, the advantages of single site cannulation consist in a reduction of cannulae-site infection risk and time-consuming nursing care. Because of the reduction of "plastic" surface in contact with blood, a decrease in the activation of inflammatory cascade is also observed. An additional advantage is the possibility to mobilize the patient, enabling him to participate in physical therapy when required.
In our experience, the most significant complication which can occur is the single cannula displacement, which should be suspected in the presence of acute patient oxygen desaturation, despite proper functioning of the ECMO oxygenator. In this reported case, the minimal movement of patient in daily manoeuvres caused a little bit modification in resistance and flow even if we made secure the cannula. This could be due to the contact of tricuspid valve. During the first four days of VV-ECMO support, three episodes of cannulae displacements occurred. A malrotation of the proximal tip, which was not facing the tricuspid valve, was observed by TEE in all three episodes. It should be highlighted that the dual lumen catheter was secured to the skin with several sutures and a bandage around the forehead which fixed the cannulae to the right side of the face.
In one case, the malrotation occurred after a coughing fit, whilst in two cases it occurred after patient mobilization, despite nursing manoeuvres were performed by a dedicated team, including perfusionist specialists who helped in monitoring and handling catheter and ECMO tubing. The cannula was always repositioned by using ultrasound guidance.
Some cases of single cannulation with Avalon Elite DLC for obese patients are reported in literature, but with lower BMI (about 30 kg/m2 ) and for a shorter ECMO support period; in fact the median duration described is between 9 and 11 days.(3,4). In our experience, the patient had greater BMI (40.1 Kg/m2 ) and the VV-ECMO was performed for 21 days and in addition our patient confirmed that the obesity decreases the sensitivity of peripheral tissues to leptin signals and can compromise the immune system as reported in literature.(6,7,8).
3. Conclusion
According to our experience, the Avalon Elite DLC offers many advantages for Veno-venous extracorporeal membrane oxygenation support in patients affected by severe acute respiratory distress syndrome, who are not responding to other medical or mechanical treatment. In particularly, in severe obese patient (BMI more than 35 Kg/m2 ), the performing of VV-ECMO with single cannulation needs a daily control of cannulae position ( we recommend transthoracic echocardiogram or chest X-rays) and a gently management of patient to reduce the dislocation of the cannulae.
Human rights statements and informed consent: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later revisions. Informed consent was obtained from the patient for being included in the image report.
References
- Peek GJ, Elbourne D, Mugford M, Tiruvoipati R, Wilson A, Allen E et al. Randomised controlled trial and parallel economic evaluation of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR). Health Technol Assess. 2010 Jul;14(35):1-46.
- Meduri U, Golden E, Freire AX, Taylor E, Zaman M, Carspn SJ et al. Methylprednisolone infusion in early severe ARDS: results of a randomised controlled trial. Chest 2007; 131: 954-963.
- Bermudez CA, Rocha RV, Sappington PL, Toyoda Y, Murray HN, Boujoukos AJ. Initial experience with single cannulation for veno-venous extracorporeal oxygenation in adults. Ann Thorac Surg 2010; 90: 991-5.
- Javidfar J, Brodie D, Wang D , Ibrahimiye AN, Yang J, Zwischenberger JB et al. Use of Bicaval Dual – Lumen Catheter for adult venovenous Extracorporeal Membrane Oxygenation. Ann Thorac Surg 2011; 91: 1763-8.
- Dolch ME, Frey L, Buerkle MA, Weig T, Wassilowsky D, Irlbeck M. Transesophageal Echocardiography-Guided technique for Extracorporeal Membrane Oxygenation dual-lumen catheter placement. ASAIO Journal 2011; 57 (4): 341-3.
- Nave H, Beutel G, Kielstein JT. Obesity – related immunodeficiency in patients with pandemic influenza H1N1. Lancet Infec Dis 2011; 11(1): 14-15
- Huttunen R, Syryãnen J. Obesity and the outcome of infection. Lancet Infect Dis 2010; 10: 442-43.
- Falagas ME, Kompoti M. Obesity and infection. Lancet Infect Dis 2006; 6: 438-46.