Information
Journal Policies
The Prevalence of Adverse Childhood Experiences and their Associations with Engagement in Risky Behaviors for HIV Infection among Adults in the United States
Gemechu B. Gerbi1,2*, Hilton Mozee2, Elaine Archie-Booker1,2, Mechelle D. Claridy2, Stephanie Miles-Richardson1,2
2.Department of Community Health and Preventative Medicine, Morehouse School of Med icine, Atlanta, USA.
Copyright : © 2018 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Background: Adverse Childhood Experiences (ACEs), including psychological, physical, and sexual abuse, as well as family dysfunction, have been shown to be associated with HIV related risky behaviors or HIV acquisition.
Objective: The objective of this study is to assess the prevalence of ACEs and their associations with engagement in HIV-related risky behaviors among persons aged 18 years and over in the US.
Methods: Data were analyzed from the 2012 Behavioral Risk Factor Surveillance System. The sample consisted of 451,656 adults. A multivariable logistic regression analysis was used to estimate adjusted odds ratios (AORs) and 95% confidence intervals (95% CIs) to assess the associations between ACEs and engagement in HIV-related risky behaviors. All analyses were conducted using SAS version 9.4.
Results: After adjusting for gender, age, race or ethnicity, level of education, and level of income and comparing to those who did not report a history of ACEs, having lived with someone who was depressed, mentally ill, or suicidal (AOR= 1.84; 95% CI=1.45, 2.31; p< .0001), having lived with someone who was a problem drinker or alcoholic (AOR= 1.59; 95% CI=1.26, 1.98; p< .0001), and having lived with someone who served time in jail or prison (AOR= 1.49; 95% CI=1.13, 1.96; p=.0044) were significantly associated with engagement in HIV-related risky behaviors.
Conclusion: The results indicate that ACEs increase the likelihood of engagement in HIV-related risky behaviors among adults in the US, underscoring the need for efforts to prevent ACEs and strengthen parents' ability to guard against their child's exposure to ACEs.
HIV, adverse childhood, risky behaviors, sex, United States,Public Health and Community Medicine
1. Introduction
In the United States (US), approximately 1.2 million people are living with HIV/ AIDS, while 50,000 individuals are being infected each year [1]. Risky behaviors that put people at higher risk for HIV infection and transmission include sharing needles or syringes, condom less sex, the exchange of sex for drugs or money, and the contraction of other sexually transmitted diseases [2]. The HIV epidemic in the US has impacted some groups more than others. These key affected populations can be grouped by transmission category but also by race and ethnicity, with African Americans having significantly higher rates of HIV infection over white Americans [3]. For example, African Americans accounted for 44% of all new HIV infections in 2014 despite comprising only 12% of the population [7]. At the end of 2014, an estimated 471,500 African Americans were living with HIV, which accounted for 43% of the total number of people living with HIV [8]. HIV also disproportionately affects the Hispanic/Latino community. In 2015, Hispanic/Latino people accounted for 24% of new diagnoses of HIV in the US, despite only representing approximately 18% of the population [9]. This disparity is influenced by a complex set of economic and socioeconomic factors, including discrimination, stigma, poverty and a lack of access to care [3].
Adverse childhood experiences (ACEs) including psychological, physical, and sexual abuse, as well as family dysfunction, have been shown to be associated with HIV related risky behaviors or HIV acquisition [10,11]. Studies have shown that ACEs are associated with disrupted neurodevelopment in early childhood which then leads to emotional, cognitive, and social mpairment [10,12]. These impairments have been associated with various psychological issues in adulthood such as anxiety, depression, difficulty forming social ties, increased likelihood of engaging in tobacco, alcohol, illicit drug use, sexual risky behaviors (e.g., multiple partners, not using protection) [11,12] unintended pregnancy and sexually transmitted disease infection [13].
The negative effects of ACEs are a growing public health concern given the prevalence of ACEs within populations. Previous studies demonstrate that the majority of the general populations (52%–74%) has experienced at least one form of ACEs before they reached 18 years [10,14-17]. A study by Felitti et al. (1998) shows that over half of respondents (52.1%) from an initial ACEs study reported having had at least one ACE [12]; however, a follow-up study revealed that over 65% of the sample had experienced at least one ACE [11,18].
The lingering effects of ACEs can influence many of the factors that have been used to explain risky behaviors associated with HIV acquisition, including substance use, depression, denial, low self-efficacy, and low self-esteem. However, little is known about ACEs and their direct link to engagement in HIV related risky behaviors or HIV acquisition. Moreover, studies have often focused on a single type of adverse experience and very few utilized a nationally representative population-based sample in the US. It is important to explore the impact of ACEs on risky behaviors associated with HIV acquisition such that the cycle of early adversity across generations is interrupted and to improve HIV prevention strategies. This study assessed the prevalence of ACEs and their associations with engagement in HIV-related risky behaviors among persons aged ≥18 in the US.
2. Methods
Data were analyzed from the 2012 Behavioral Risk Factor Surveillance System (BRFSS), a collaborative project between all of the 50 states in the US., the District of Columbia, three US territories (Puerto Rico, Guam, and the US Virgin Islands) and the Centers for Disease Control and Prevention (CDC) [19]. The BRFSS is a nationally representative, cross- sectional, random-digit dial telephone (both landline and cellular) survey that collects uniform, state-specific data regarding health practices and risk behaviors that are linked to chronic diseases, injuries, and preventable infectious diseases that affect noninstitutionalized aged ≥ 18 years who reside in the US and its territories [19].
The BRFSS standardized questionnaires are developed by CDC and state public health departments to include a standard core, optional modules, and state-added questions [19,20]. Detailed information about the study design and methodology is available from the CDC's website:http://www.cdc.gov/brfss/.Since BRFSS data files are publicly available via the website: http://www.cdc.gov/brfss/annual_data/ annual_data.htm, data use agreements were not required for this study. Moreover, as the BRFSS data do not contain personally identifiable information, this study is exempt from the Institutional Review Board review.
3. Measures
All measures in this study were based on self-reported data obtained from the 2012 BRFSS.
Survey participants responded to the following questions to indicate their engagement in HIV-related risky behaviors:
• Have you used intravenous drugs in the past year?
• Have you been treated for a sexually transmitted or venereal disease in the past year?
• Have you given or received money or drugs in exchange for sex in the past year?
• Have you had anal sex without a condom in the past year?
Possible responses were “yes”, “no”, “don’t know/not sure”, or “refused. However, we included only records with “yes” or “no” responses. Records with “unknown” or “refused” responses or missing data were excluded from the analysis to minimize underestimation.
We assessed four ACEs that happened before the participants were 18 years old. They included: 1) living with someone who was depressed, mentally ill, or suicidal, (“Did you live with anyone who was depressed, mentally ill, or suicidal?”); 2) living with someone who was a problem drinker or alcoholic, (“Did you live with anyone who was a problem drinker or alcoholic?”); 3) living with someone who served time or was sentenced to serve time in a prison, jail, or other correctional facility (“Did you live with anyone who served time or was sentenced to serve time in a prison, jail, or other correctional facility?”); and 4) parents separated or divorced (“Were your parents separated or divorced?”). Only those responses with “yes” or “no” were included in the analysis. Records with “unknown” or “refused” responses or missing data were excluded from the analysis to minimize underestimation.
Control variables included were socio- demographic characteristics including gender, race or ethnicity, age, education, income, and region of residence. Gender was dichotomized as female and male. Race or ethnicity was categorized as Caucasian, African American, American Indian Alaskan Native, Asian, Hispanic/Latino, Hispanic, Native American or Pacific Islander and mixed. Age was categorized as 18–34, 35–44, 45–64, 65–74 and ≥ 75 years. Gender was dichotomized. Education was categorized as high school or less, some college, and college graduate. Income was categorized as ≤$24,999, $25,000–$49,999, $50,000–$74,999, and ≥ $75,000.
Initially, we performed a bivariate analysis to assess the association between each of four ACEs as a primary independent variable and engagement in HIV related risky behaviors. We included all variables that had achieved p ≤ 0.05 in the bivariate analysis in our final multivariable logistic regression model, and obtained the Adjusted Odds Ratios (AORs) and 95% Confidence Intervals (95% CIs). A 2-sided p value of ≤ 0.05 was used to assess statistical significance. A multivariable logistic regression analysis was employed to adjust for the potential confounding effects of gender, race or ethnicity, age, education, and income on the associations between ACEs and engagement in HIV related risky sexual behaviors. Analyses were conducted using SAS version 9.4[21].
4. Results
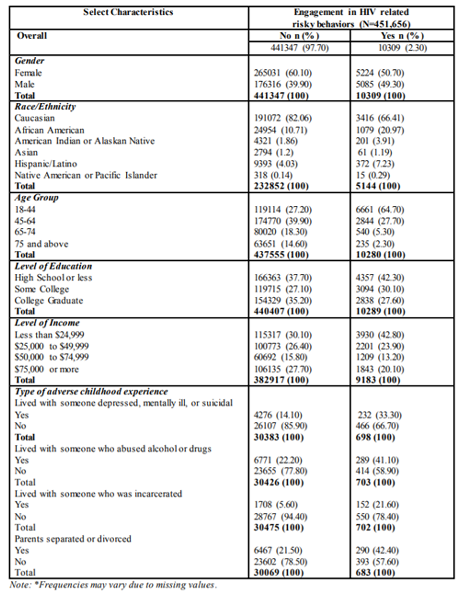
The distribution of engagement in HIV-related risky behaviors by sample sociodemographic characteristics and ACEs is reported in Table1.
Of the 451, 656 participants who responded to the HIV-related risk behaviors question, 10,309 (2.30%) reported engagement in HIV risky behaviors and 441,347 (97.70%) reported not engaging in HIV-related risky behaviors (Table 1). Of the 10,309 respondents who reported engagement in HIV-related risky behaviors, 50.7% were female; 66.41% were Caucasian; 64.7% were between the ages of 18-44 years; 42.3% had high school or less level of education; 42.8% had annual household incomes less than $25,000. Table 1 also shows that one third (33.3%) of the participants who reported engagement in HIV-related risky behaviors lived with someone who was depressed, mentally ill, or suicidal; 41.1% lived with someone who was a problem drinker or alcoholic; 21.6% lived with someone who served time or was sentenced to serve time in a prison, jail, or other correctional facility;
and 42.4% lived with separated or divorced parents.
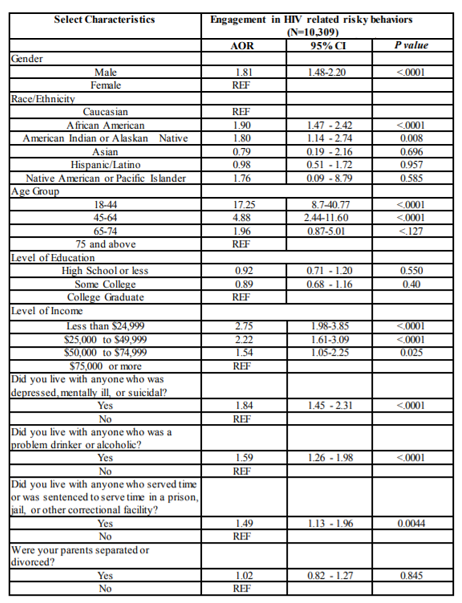
Table 2 presents the results of multivariable logistic regression analysis for sociodemographic characteristics (gender, race or ethnicity, age, education, and income) and ACEs variables regressed on self- reported engagement in HIV related risky behaviors. After adjusting for the aforementioned sociodemographic variables, the following were associated with higher odds of reporting engagement in HIV related risky behaviors: being male (AOR=1.81; 95% CI=1.48-2.20; p< .0001), African American (AOR= 1.90; 95% CI=1.47-2.42; p< .0001), American Indian or Alaskan Native (AOR= 1.80; 95% CI= 1.14-2.74; p=.008), those in the age group 18-44 years (AOR=17.25; 95% CI=8.70-40.77; p< .0001); those in the age group 45-64 years (AOR=4.88; 95% CI=2.44-11.60; p< .0001); having an annual household income≤ $24,999 (AOR=2.75; 95% CI=1.98-3.85; p< .0001), having an income between $25,000 to $49,999 (AOR=2.22; 95% CI= 1.61-3.09; p< .0001), having an income between $50,000 to $74,999 (AOR=1.54; 95% CI= 1.05-2.25; p=025) having lived with anyone who was depressed, mentally ill, or suicidal (AOR=1.84; 95% CI= 1.45-2.31; p< .0001)), having lived with anyone who abused alcohol or drugs, (AOR=1.59; 95% CI= 1.26-1.98; p< .0001), and having lived with anyone who served time or was sentenced to serve time in a prison, jail, or other correctional facility (AOR=1.49; 95% CI= 1.13-1.96; p=.0044)[Table 2].
5. Discussion
The current study is among few studies to provide estimates of the prevalence of ACEs and their associations with engagement in HIV- related risky behaviors using anationally representative population-based sample in the US. Contrary to the findings of previous studies [13,22-24] which report that females have significantly greater odds of engaging in HIV risk behaviors when they experienced three or more ACEs, our findings show that males were 69% more likely to report having engaged in HIV-related risky behaviors than their female counterparts. Two potential explanations are offered for the gender differences observed in engagement in HIV-related risky behaviors in our study. First, perception of risk differs between males and females, with males less likely to perceive risk of HIV infection though certain encounters resulting in increased risky behaviors [25]. Second, there may be differential coping strategies between males and females during adverse events that come into play. Previous research has shown that stress coping is associated with traditional gender roles [26,27]. Traditional gender perspectives prescribe females as dependent and emotional, and males as independent and rational [28]. For these coping strategies, females use emotion-focused strategies more than males to cope with stressful family events, while males focus on rational and detachment strategies to tackle stressful family events. The differential coping strategies between males and females may mediate the relationships between childhood exposure to adverse events and adult HIV-related risky behaviors where emotion-focused coping results are a more positive adaptation over time than the detachment strategy [28]. More research should be conducted to tease out a possible gender effect on HIV-related risky behaviors.
Contrary to other studies which report that African Americans were less likely to report engagement in HIV-related risky behaviors when compared to their Caucasian counterparts [33,34], our study found that African Americans were 82% more likely to report having engaged in HIV-related risky behaviors. A highly plausible explanation for this finding is related to specific behaviors that create risk within ethnic groups. For example, a previous study showed that the use of certain drugs (i.e., marijuana and crack) used more often among Caucasians, contributed significantly to the prediction of some risky sexual behavioral practices (i.e., anal intercourse, sexual experiences with a prostitute, and having a history of STDs) among Caucasians, while African Americans experienced a significantly greater angry reaction during the negotiation and use of condoms than did whites [35]. The intensity of anger surrounding the use of condoms in the African-American population may interfere with the rational decision to protect oneself from the consequences of risky sex [35,36]. In our study, risky behaviors associated with HIV infection were determined if the respondents reported that they used intravenous drugs, had been treated for a sexually transmitted or venereal disease, had given or received drugs or money in exchange for sexual favors, or had anal intercourse without a condom during the past year. It is likely that differences between African Americans and Caucasians in HIV- related risky behaviors may be due to lack of attention to specific behaviors that create risk within ethnic groups. Further research is needed to assess the differential effect of individual HIV-related risky behaviors within and between racial and ethnic groups.
Results from this study also show that American Indian or Alaska Natives are 84% more likely to participate in HIV-related risky behaviors than Caucasians. For this specific population, there are limited studies assessing this association. A possible explanation for this finding is related to oppression, prejudice and racism [37]. Historical trauma and current social processes experienced by American Indians/Alaska Natives has led to physical, cultural, and psychological genocide and complex feelings of internalized shame, negative self-image, depression, and powerlessness [38]. These negative experiences are the primary reasons for the suffering and chronic sorrow that confront many Native people. These experiences render indigenous people vulnerable to behaviors associated with HIV acquisition[39]. Thus, while race and ethnicity themselves are not health-risk factors, they equate with determinants that perpetuate risky behaviors among American Indians/Alaska Natives. A study by Vernon (2002) indicates that people are susceptible to HIV infection when they lack self-respect and experience physical, psychological, and sexual abuse or rape. A sense of powerlessness limits their ability to remain safe in domestic settings and to insist on a monogamous relationship or condom use [39].
The findings of this study show that multiple ACEs including having lived with someone who was depressed, mentally ill, or suicidal, having lived with someone who was a problem drinker or alcoholic, having lived with smeone who served time in jail or prison, and having lived with separated or divorced parents were associated with higher odds of engagement in HIV related risky behaviors in adulthood after controlling for relevant sociodemographic factors. These findings are concerning and are similar to the findings reported from previous studies [11-13,18]. Previous studies have demonstrated that individuals who reported experiencing one of the ACE such as parental incarceration during childhood had greater odds of having multiple sex partners during adolescence (OR =1.40), and adulthood (OR = 1.20) [40]. There was also an increased risk of contracting a sexually transmitted infection during adulthood (OR = 1.76) among individuals who had been affected by parental incarceration [40]. Previous studies provided a mechanism by which ACEs might impact HIV-related risk behaviors in later life. Some researchers have found that self-efficacy [41-43], balanced power relationship [42,43] and risky romantic relationships [44] can mediate the relationship between ACEs and HIV-related risky behaviors.
An interpretation of the present findings must consider some limitations. First, the BRFSS is a telephone based survey and is administered to civilian, noninstitutionalized adults. Therefore, the BRFSS excludes individuals without telephone service, those on military bases, and individuals in institutions. For this reason, generalizability to the entire US population is limited. Second, the data on ACEs and HIV related risky behaviors rely on retrospective self-reported data. It is possible that participants had difficulty recalling important information, and/or they provided socially desirable responses to sensitive questions. As a result, participants' self-reported behaviors could be conservative estimates of their actual behavior. Despite these limitations, the findings of the current research have several important implications for future research and intervention. First, future studies on the impacts of protective and potential risk factors associated with engagement in HIV-related risky behaviors are needed. For example, future studies should focus on how different levels of social support, as well as functions and sources of social support impact the prevalence of HIV-related risky behaviors among individuals who experienced ACEs.
6. Conclusion
In summary, findings of this study indicate that ACEs increase the likelihood of engagement in HIV-related risky behaviors among persons aged 18 years and over in the US. These findings highlight the need for HIV prevention strategies specifically for adults who experienced ACEs. Our findings suggest that ACEs may predispose individuals to HIV-related risky behaviors in adulthood. Given the cumulative impact of ACEs on health outcomes in adulthood, targeted behavioral, psychosocial, and policy interventions that involve various key disciplines including medicine, social work, public health, and the educational system are needed to improve recognition, treatment, and prevention of ACEs and their adverse consequences in adulthood, especially as it pertains to HIV-related risky behaviors.
References
- Centers for Disease Control and Prevention, monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas—2012. HIV Surveillance Supplemental Report 2014 2014; 19(3).
- Patrick, M.E., et al., HIV/AIDS risk behaviors and substance use by young adults in the United States. Prev Sci, 2012. 13(5): p. 532-8.
- Centers for Disease Control and Prevention (March, Today's HIV/AIDS Epidemic. Accessed from https://www.cdc.gov/nchhstp/newsroom/d ocs/factsheets/todaysepidemic-508.pdf. Accessed date: May, 17, 2018.
- Centers for Disease Control and Prevention (September, HIV among Gay and Bisexual Men. Accessed from https://www.cdc.gov/hiv/pdf/group/msm/c dc-hiv-msm.pdf. Accessed date, May 17, 2018.
- Centers for Disease Control and Prevention, HIV Surveillance Report, Diagnoses of HIV Infection in the United States and Dependent Areas, 2016, Vol. 28; November 2017. HIV diagnosis data are estimates from 50 states, the District of Columbia, and 6 U.S. dependent areas. Estimates for 2016 are preliminary and are not included in trend calculations.
- Centers for Disease Control and Prevention, HIV Surveillance—Epidemiology of HIV Infection (through 2016); November 2017.
- Centers for Disease control and prevention (2015), Diagnoses of HIV Infection in the United States and Dependent Areas, 2014. HIV Surveillance Report, Volume 26. Accessed from: https://www.cdc.gov/hiv/pdf/library/repor ts/surveillance/cdc-hiv-surveillance-report-us.pdf. Accessed date May 16, 2018.
- Centers for Disease Control and Prevention (January2018), HIV and African Americans. Accessedfrom: https://www.cdc.gov/hiv/pdf/gro up/racialethnic/africanamericans/cdc-hiv-africa namericans.pdf. Accessed date: May 16, 2018.
- Centers for Disease Control and Prevention, HIV among Hispanics/Latinos. Accessed from: https://www.cdc.gov/hiv/group/ racialethnic/hispaniclatinos/index.html (Access ed May 17, 2018).
- Anda, R.F., et al., The enduring effects of abuse and related adverse experiences in childhood. A convergence of evidence from neurobiology and epidemiology. Eur Arch Psychiatry Clin Neurosci, 2006. 256(3): p. 174-86.
- Dube, S.R., et al., Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: the adverse childhood experiences study. Pediatrics, 2003. 111(3): p. 564-72.
- Felitti, V.J., et al., Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med, 1998. 14(4): p. 245-58.
- Hillis,S.D.,etal., Adverse childhood experiences and sexually transmitted diseases in men and women: a retrospective study. Pediatrics, 2000. 106(1): p. E11.
- Haatainen, K.M., et al., Gender differences in the association of adult hopelessness with adverse childhood experiences. Soc Psychiatry Psychiatr Epidemiol, 2003. 38(1): p. 12-7.
- Ramiro, L.S., B.J. Madrid, and D.W. Brown, Adverse childhood experiences (ACE) and health-risk behaviors among adults in a developing country setting. Child Abuse Negl, 2010. 34(11): p. 842-55.
- Schussler-Fiorenza Rose, S.M., et al., Adverse Childhood Experiences, Support, and the Perception of Ability to Work in Adults with Disability. PLoS One, 2016. 11(7): p. e0157726.
- Schussler-Fiorenza Rose, S.M., D. Xie, and M. Stineman, Adverse childhood experiences and disability in U.S. adults. PM R, 2014. 6(8): p. 670-80.
- Dube, S.R., et al., Adverse childhood experiences and the association with ever using alcohol and initiating alcohol use during adolescence. J Adolesc Health, 2006. 38(4): p. 444 e1-10.
- Centers for Disease control and prevention (2013a), Behavioral risk factor surveillance system. Overview: BRFSS 2012. website: http://www.cdc.gov/brfss/.
- Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Child maltreatment: Facts at a glance.2014 www.cdc.gov/violencepr evention/pdf/childmaltreatment-facts-at-a-gla nce.pdf.
- SAS Institute Cary NC USA.
- Aidala, A.A., et al., Sexual behaviors and sexual risk in a prospective cohort of HIV-positive men and women in New York City, 1994-2002: implications for prevention. AIDS Educ Prev, 2006. 18(1): p. 12-32.
- Golin, C., et al., Psychosocial characteristics and sexual behaviors of people in care for HIV infection: an examination of men who have sex with men, heterosexual men and women. AIDS Behav, 2009. 13(6): p. 1129-42.
- Donenberg, G.R., et al., Holding the line with a watchful eye: the impact of perceived parental permissiveness and parental monitoring on risky sexual behavior among adolescents in psychiatric care. AIDS Educ Prev, 2002. 14(2): p. 138-57.
- Mitchell, M.M. and W.W. Latimer, Gender differences in high risk sexual behaviors and injection practices associated with perceived HIV risk among injection drug users. AIDS Educ Prev, 2009. 21(4): p. 384-94.
- Al-Bahrani, M., et al., Age and gender differences in coping style across various problems: Omani adolescents' perspective. J Adolesc, 2013. 36(2): p. 303-9.
- Matud, M.P., J.M. Bethencourt, and I. Ibanez, Gender differences in psychological distress in Spain. Int J Soc Psychiatry, 2015. 61(6): p. 560-8.
- Green, D.L. and N. Diaz, Gender differences in coping with victimization. Brief. Treat. Crisis Interv. 8 (2), 195–203. 2008.
- Risser, J., et al., Gender differences in social support and depression among injection drug users in Houston, Texas. Am J Drug Alcohol Abuse, 2010. 36(1): p. 18-24.
- Ramiro, M.T., Teva, I., Bermúdez, M.P., and G. Buela-Casal, Social support, self-esteem and depression: relationship with risk for sexually transmitted infections/HIV transmission. Int. J. Clin. Health Psychol. 13 (3), 181–188. 2013.
- Dalgard, O.S., et al., Negative life events, social support and gender difference in depression: a multinational community survey with data from the ODIN study. Soc Psychiatry Psychiatr Epidemiol, 2006. 41(6): p. 444-51.
- Qiao, S., X. Li, and B. Stanton, Social support and HIV-related risk behaviors: a systematic review of the global literature. AIDS Behav, 2014. 18(2): p. 419-41.
- Brooks, A.J., et al., Racial/ethnic differences in the rates and correlates of HIV risk behaviors among drug abusers. Am J Addict, 2013. 22(2): p. 136-47.
- Semple, S.J., et al., Ethnic differences in substance use, sexual risk behaviors, and psychosocial factors in a sample of heterosexual methamphetamine users. Subst Use Misuse, 2009. 44(8): p. 1101-20.
- Johnson, E.H., et al., What is the significance of black -white differences in risky sexual behavior? J Natl Med Assoc, 1994. 86(10): p. 745-59.
- Diamond, C., et al., HIV-infected American Indians/Alaska natives in the Western United States. Ethn Dis, 2001. 11(4): p. 633-44.
- Sileo, T., HIV/AIDS Prevention in American Indian and Alaska Native Communities. Volume 14, No. 4 - Summer 2003
- Hunt, D.,E.,M. Gooden, and C. Barkdul1, Walking in moccasins: Indian child welfare in the 21st century. In A. L. Sallee, H. A. Lawson, & K. Briar-Lawson (Eds.). Innovative practices with vulnerable children and families (pp. 165 - 187). Dubuque, IA: Eddie Bowers Publishing Co., Inc. 2001.
- Vernon, I.S., Violence, HIV/AIDS, and Native American women in the twenty-first century. The American Indian Culture and Research Journal, 26(2), 115-133. 2002.
- Khan, M.R., et al., Early age at childhood parental incarceration and STI/HIV-related drug use and sex risk across the young adult lifecourse in the US: Heightened vulnerability of black and Hispanic youth. Drug Alcohol Depend, 2018. 183: p. 231-239.
- Sales, J.M., et al., The mediating role of partner communication skills on HIV/STD-associated risk behaviors in young African American females with a history of sexual violence. Arch Pediatr Adolesc Med, 2008. 162(5): p. 432-8.
- Raiford, J.L., G.M. Wingood, and R.J. DiClemente, Correlates of consistent condom use among HIV-positive African American women. Women Health, 2007. 46(2-3): p. 41-58.
- Brown, J.L., et al., Impact of Abuse History on Adolescent African-American Women's Current HIV/STD-associated Behaviors and Psychosocial Mediators of HIV/STD Risk . J Aggress Maltreat Trauma, 2014. 23(2): p. 151-167.
- Wilson, H.W. and C.S. Widom, Pathways from childhood abuse and neglect to HIV-risk sexual behavior in middle adulthood. J Consult Clin Psychol, 2011. 79(2): p. 236-46.