Information
Journal Policies
ARC Journal of Clinical Case Reports
Volume-2 Issue-1, 2016, Page No: 14-18
Warthin’s Tumor of the Parotid Gland: A Case Report
Dr. Sumit Goel1, Dr. Sangeeta Malik1, Dr. Swati Gupta1, Dr. Ravi Prakash SM 1*
1. Department of Oral Medicine and Radiology, Subharti Dental College, Swami Vivekanand Subharti University, Subhartipuram, NH-58, Delhi Haridwar Bypass road, Meerut, Uttar Pradesh.
Citation : Sumit G, Sangeeta M, Swati G, Ravi P.SM. Warthin’s Tumor of the Parotid Gland: a Case Report. ARC Journal of Clinical Case Reports. 2016;2(1):14–18.DOI : dx.doi.org/10.20431/2455-9806.0201004
Copyright : © 2016 Ravi P.SM. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Salivary gland tumours represent approximately 3% of all head and neck tumours. Warthin’s tumour, also known as Papillary cystadenoma lymphomatosum (PCL), is the second most frequent benign salivary gland neoplasm usually found in the superficial lobe of the parotid and is strongly associated with smokers. Here, we report a classical case of Warthin’s tumour of ten years duration in a 52- year-old male patient in the left parotid gland with special emphasis on its uniqueness and role of investigations.
1.Introduction
Warthin’s tumor is a benign neoplasm predominantly found in the parotid gland of the salivary glands. It was initially described in 1929 by Aldred Scott Warthin. Warthin’s tumor is synonymous for papillary cystadenoma lymphomatosum, adenolymphoma, and cystadenolymphoma. It makes up 14% to 30% of parotid tumors. It occurs between the sixth and seventh decades of life, with male predominance and has been found to be associated with smoking [1,2].
Various theories have been given to describe pathogenesis of Warthin’s tumor like the development of the tumor from salivary ducts imprisoned in intraparotid or paraparotid lymph nodes; or lymphocytic infiltration in a pre-existing adenoma; or is a delayed hypersensitivity disease. EBV has been detected in Papillary Cystadenoma Lymphomatosum and is proposed to play a part in the development of the tumour, perhaps as an antigenic stimulus. Recent molecular evidence demonstrated the presence of a polyclonal epidermal component and showed no clonal allelic losses suggesting an entity that is not a true neoplasm [1,3].
It has been found that minimally invasive approaches can be performed with confidence with extracapsular dissection or partial superficial parotidectomy resulting in potentially reduced morbidity [4]. Here we report a classical case of Warthin’s tumour in parotid gland in a 52 year old male patient with special emphasis on investigations.
2.Case Report
A 52 year old male patient reported to the outpatient department with the chief complaint of swelling on left side of face. The swelling had been present since past 10 yrs. had gradually increased in size, but since past one month, the swelling was associated with dull and intermittent pain which aggravated during chewing food and relieved on its own. The patient was a chronic smoker since 35 yrs smoking 15 bidis /day. On examination, there was a solitary, well circumscribed swelling in left preauricular region measuring about 2.5* 2.5mm in size, extending superio-inferiorly from left tragus up to left angle of mandible; and anteroposteriorly from 2 cm short of a line dropped from the outer canthus of the left eye and posteriorly up to 1cm beyond the left angle of mandible (Figure.1). The colour and surface texture of the overlying skin was similar to the adjacent skin. On palpation, the swelling was non -tender, non warm, soft to firm in consistency with overlying skin being freely movable. Provisional diagnosis was in favour benign tumour of left Parotid gland.
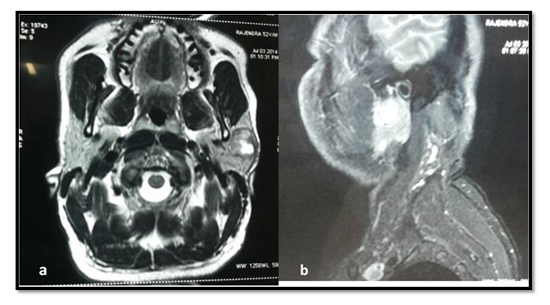
Investigations carried out were ultrasound guided FNAC of left parotid gland and MRI. Ultrasonography revealed well defined, oval, hypo-echoic nodules measuring approximately 26x18x19 mm with areas of cystic necrosis. Fine needle aspiration cytology (FNAC) showed numerous mature and activated lymphoid cells lying in tight cluster and papillaroid structure of oncocytic cell. These findings were suggestive of Warthin’s tumor. MRI findings revealed a well circumscribed lobulated lesion measuring 17x16x27 mm seen in superficial lobe of left parotid gland. The retro-mandibular vein, temporal & zygomatic branches of right facial nerve was postero-medial to the aforesaid lesion. The lesion was hypointense on T1& heterogeneously hyperintense on T2 & STIR images with ill-defined cystic areas (Figure.2a and b). Based on these findings, the final diagnosis was Warthin’s Tumor.
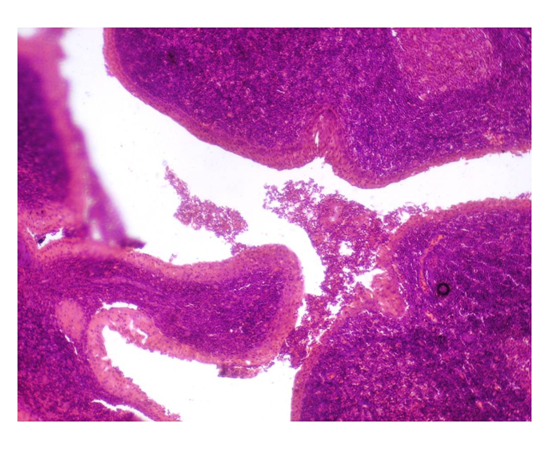
Superficial parotidectomy was then carried out and specimen sent for histopathological examination (Figure.3) which was cellular and revealed bilayered ductal epithelium of multiple papillary infoldings protruding into cystic spaces. The inner luminal layer of epithelium was made up of tall columnar cells with centrally placed, hyperchromatic nucleus. Beneath this layer, the second layer was composed of cuboidal cells. The epithelium was supported by lymphoid stroma showing germinal center formation. The findings were conclusive for Warthin’s tumor. Differential diagnoses considered were pleomorphic adenoma, Warthin’s tumor, oncocytoma, mucoepidermoid carcinoma and adenoid cystic carcinoma.
Superficial parotidectomy was then carried out and specimen was sent for histopathological examination which revealed bilayered ductal epithelium of multiple papillary infoldings protruding into cystic spaces. The inner luminal layer of epithelium was made up of tall columnar cells with centrally placed, hyperchromatic nucleus. Beneath this layer, the second layer was composed of cuboidal cells. The epithelium was supported by lymphoid stroma showing germinal center formation. The findings were conclusive for Warthin’s tumor. He is still under regular follow up and care.
3.Discussion
In Asian population, Warthin Tumor constitutes 25 per cent of all benign parotid tumours with male: female ratio of 4.6: 1 [5]. In a study by Chung et al[5], its ratio to pleomorphic adenomas has been found to be 1: 1.9. When compared to other benign parotid tumors, it has been found to occur in a significantly older age group (mean 60 year vs 48 year) with male gender more prevalent (61% vs 33%) and mostly found in the parotid tail (86% vs 61%) [6].Warthin tumors predominantly have unilateral location of the parotid gland although bilaterality and multiplicity are common features [6]. Clinically, the tumour may be unilateral, bilateral but asymptomatic in 90% of cases. Patients may have facial pain, ipsilateral earache, tinnitus [1,3]. The present case was reported in a 52 year old male patient with 10 years long history.
Smokers have a 40-fold greater risk than non-smokers of developing a Warthin's tumour among Asian population. This is hypothesized to be caused by retrograde flow of substances in tobacco smoke into salivary ducts or by excretion of substances from smoke into the ducts [2,5].
Fine-needle aspiration (FNAC) has played a larger role in recent years. In general, FNAC has good overall accuracy for diagnosing salivary gland neoplasms (87% to 97%), and it has been widely used for the diagnosis of Warthin tumors [2]. In the present case also FNAC was useful in helping us reach the correct diagnosis.
Although fine needle aspiration cytology is the most cost-effective and minimally invasive way to determine the histologic character of a parotid tumor, role of imaging cannot be undermined. Imaging helps not only for assessing the extent of a salivary gland tumor and the relationship to adjacent structures, but also for determining whether the tumor is benign or malignant and thus influencing the choice of surgical procedure. In the present case, the patient underwent utrasonography and MRI. Papillary Cystadenoma Lymphomatosum has been reported as echogenic, strikingly hypoechoic or sonolucent with few internal focal echoes. Further, it shows the coarsest pattern among the benign salivary tumours, which is believed to reflect discrete septation of their cystic components [3]. Most Warthin tumors involve the inferior pole of parotid glands and have a smooth margin on T1- and T2-weighted images. In our patient superficial lobe of parotid was involved. Warthin tumor usually appears as hypointense areas on short tau inversion recovery (STIR) and T2-weighted images; and shows low apparent diffusion coefficient values on diffusion-weighted images[7]. Izzo L et al suggested that when dealing with a poorly vascularised mass at Color/Power Doppler and signal hyperintensity in T2 with marked or partial enhancement after contrast, lesions can be diagnosed as pleomorphic adenoma or Warthin’s tumour, in its cystic variant; whereas, in the case of a reduced signal in T2 and without significant enhancement, lesions can be considered as Warthin’s tumour (solid form) [8]. In our patient, the lesion was hypointense on T1 & heterogeneously hyperintense on T2 & STIR images with ill-defined cystic areas.
Conventional CT or CT sialography permits better definition of the tumour toward surrounding tissue especially the relationship of the facial nerve which is of interest. Warthin’s tumor is patchy and shows more attenuation than homogeneous pleomorphic adenoma. The wash-out image of scintigraphy is important for diagnosing a Warthin's tumour which accumulates and retains 99m Tc-pertechnetate while a normal parotid gland excretes it on stimulation with ascorbic acid; and most other benign tumours do not accumulate it at all [3].
Superficial parotidectomy is the treatment of choice for Warthin’s tumor. The recurrence rate is found to be 0% in the solitary and 10% in the multicentric tumours. Incomplete excision and multicentricity are usual predictors of recurrence [9]. Our patient has been successfully treated with superficial parotidectomy with preservation of facial nerve one year back and is still under regular follow up. The various postsurgical complications of this procedure as documented in the literature are such as paresis of the ear lobe resulting from manipulation and / or section of the auricularis magnus branch of superficial cervical plexus, Frey Syndrome, hematomas, infections, seromas, accumulation of fluid under the flap puncture, paralysis / paresis of the facial nerve [10].
Warthin’s tumor is clinically indistinguishable from other benign lesions of the parotid. Histopathologically, Warthin’s tumor has a highly distinctive morphology and generally poses no problem in diagnosis. It is composed of bilayered oncocytic and basaloid epithelium forming cystic structures, papillae and glands that are accompanied by a dense lymphoid stroma. It needs to be differentiated from oncocytoma, squamous cell or mucoepidermoid carcinoma and a variant of papillary thyroid carcinoma recently reported as “Warthin-like”[1].
Malignant transformation of Warthin's tumour or carcinoma ex-papillary cystadenorna lymphomatosum is extremely rare. Malignant tumours arising in this tumour include squamous carcinoma, undifferentiated carcinoma, oncocytic adenocarcinoma and mucoepidermoid carcinoma, Merkel’s cell tumour [3,10].
Clinically it is difficult to differentiate Warthin’s tumour from other benign parotid tumors although histologically it has quite distinctive picture. This entity must be considered a strong possibility in smokers above 50 years old with suspected benign tumor of salivary gland. Investigations like FNAC and scintigraphy have been of a great help in making the correct diagnosis. Many of the recent studies have emphasized upon the role of imaging like MRI and ultrasonography to be able to distinguish Warthin’s tumor from other benign tumors.
References
- Faur A, Lazăr E, Cornianu M, Dema A, Vidita CG, Găluşcan A. Warthin tumor: a curious entity--case reports and review of literature. Rom J Morphol Embryol .2009; 50(2):269-73.
- Robert L. Hatch, MD, and Sejal Shah, BS. Warthin Tumor: A Common, Benign Tumor Presenting as a Highly Suspicious Mass. J Am Board Fam Pract. 2005; 18(4):320-2.
- Patil K, Mahima V G, Kalia S. Papillary cystadenoma lymphomatosum : Case report and review of literature. Indian J Dent Res 2005;16:153.
- Witt RL, Iacocca M, Gerges F. Contemporary diagnosis and management of Warthin's tumor. Del Med J. 2015 Jan; 87(1):13-6.
- Chung YF1, Khoo ML, Heng MK, Hong GS, Soo KC. Epidemiology of Warthin's tumour of the parotid gland in an Asian population. Br J Surg. 1999 May; 86(5):661-4.
- Patel DK, Morton RP. Demographics of benign parotid tumours: Warthin's tumour versus other benign salivary tumours. Acta Otolaryngol. 2016; 136(1):83-6.
- Ikeda M, Motoori K, Hanazawa T, Nagai Y, Yamamoto S, Ueda T, et al. Warthin tumor of the parotid gland: diagnostic value of MR imaging with histopathologic correlation. Am J Neuroradiol. 2004; 25(7):1256-62.
- Izzo L, Casullo A, Caputo M, et al. Space occupying lesions of parotid gland. Comparative diagnostic imaging and pathological analysis of Echo Color/Power Doppler and of magnetic resonance imaging. Acta Otorhinolaryngologica Italica. 2006; 26(3):147-153.
- Ethunandan M, Pratt CA, Higgins B, Morrison A, Umar T, Macpherson DW, Wilson AW. Factors influencing the occurrence of multicentric and 'recurrent' Warthin's tumour: a cross sectional study. Int J Oral Maxillofac Surg. 2008; 37(9):831-4.
- Chedid HM, Rapoport A, Aikawa KF, Menezes Ados S, Curioni OA. Warthin's tumor of the parotid gland: study of 70 cases. Rev Col Bras Cir. 2011; 38(2):90-4.